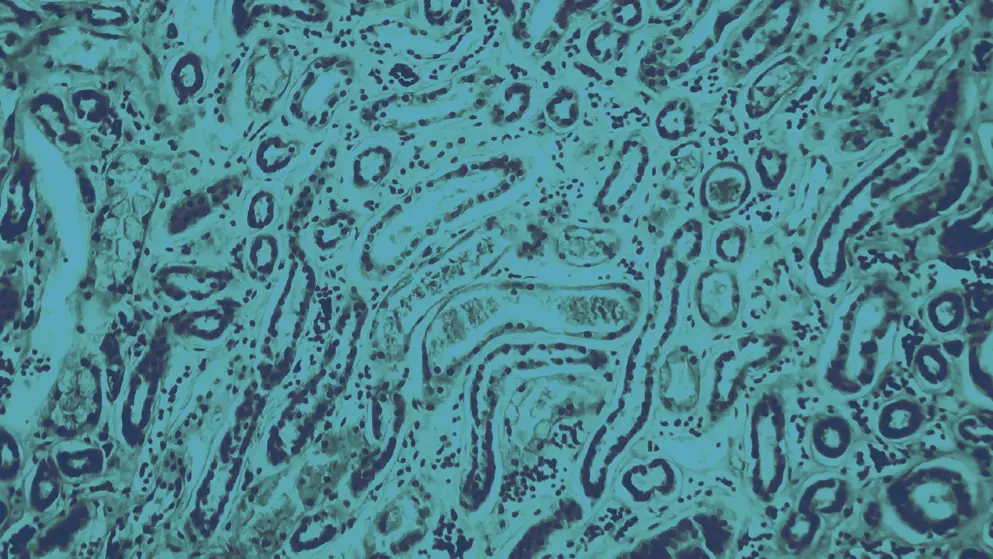
Glomerulonephritis
Glomerulonephritis refers to a group of renal diseases caused by immune-mediated damage to the glomerular basement membrane, mesangium, or capillary endothelium. It accounts for ~10% of acute kidney injuries in adults.
There are two main forms:
- Primary glomerular disease – occurs in isolation
- Secondary glomerular disease – part of a multisystem condition (e.g., systemic lupus erythematosus, polyarteritis nodosa)
Prognosis varies by subtype, making early diagnosis and appropriate management essential. Most forms are progressive and, without timely treatment, may advance to chronic glomerulonephritis, characterized by tubulointerstitial fibrosis, declining glomerular filtration rate, and accumulation of uremic toxins. This can lead to chronic kidney disease and end-stage renal disease, often with cardiovascular complications.
What are the main subtypes of glomerulonephritis?
Glomerulonephritis comprises five pathogenic types:
- Immune-complex glomerulonephritis (e.g., IgA nephropathy, lupus nephritis)
- Pauci-immune glomerulonephritis (e.g., MPO-ANCA glomerulonephritis)
- Anti–glomerular basement membrane (anti-GBM) glomerulonephritis
- Monoclonal immunoglobulin glomerulonephritis (e.g., immunotactoid glomerulopathy)
- C3 glomerulopathy (e.g., dense deposit disease)
What are the symptoms of glomerulonephritis?
Common features of glomerulonephritis include hematuria (microscopic or macroscopic), hypertension, and edema. Patients may also present with oliguria, azotemia, and signs of fluid overload (e.g., pulmonary crackles, raised jugular venous pressure). In systemic forms, symptoms may reflect the underlying condition, such as rash, arthralgia, or hemoptysis.
How is glomerulonephritis diagnosed?
A diagnosis of glomerulonephritis involves blood tests (renal function, electrolytes, complement levels, autoantibodies), urinalysis (including red cell casts), imaging (chest X-ray, renal ultrasound), and renal biopsy to confirm subtype and severity.
What are the treatments for glomerulonephritis?
Primary glomerulonephritis is treated with supportive care and disease-modifying therapy. Secondary forms require treatment of the underlying condition. Immunosuppressive options include corticosteroids, rituximab, cytotoxic agents, and plasma exchange. Controlling blood pressure and monitoring renal function are also key.
Developed by EPG Health for Medthority, independently of any sponsor.