KM55 Monoclonal Antibody Staining in IgA-Dominant Infection-Related Glomerulonephritis
KM55 Monoclonal Antibody Staining in IgA-Dominant Infection-Related Glomerulonephritis
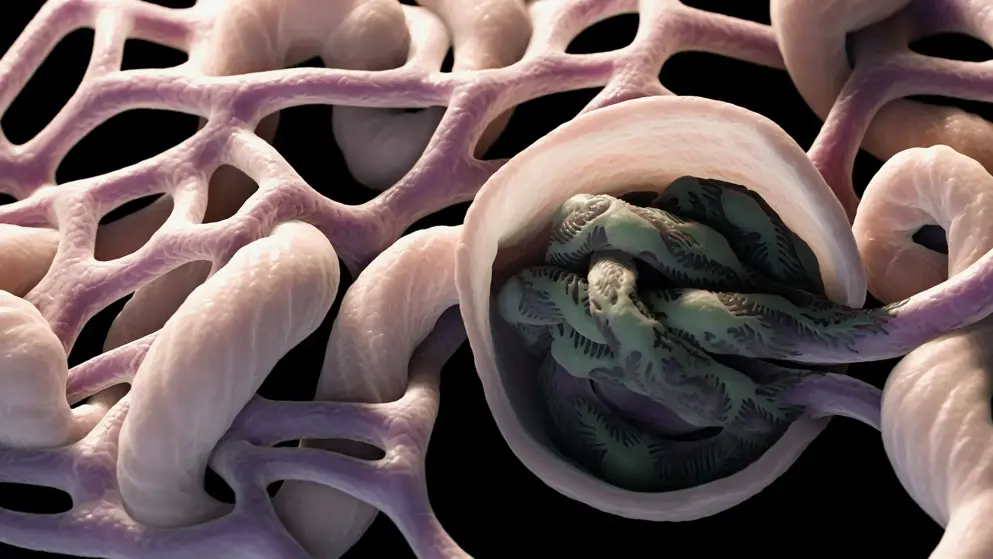
Introduction: IgA-dominant infection-related glomerulonephritis (IgA-IRGN) is a unique form of IRGN, which needs to be distinguished from IgA nephropathy (IgAN), due to overlapping clinical and pathological features. The key factor in the pathogenesis of IgAN is galactose-deficient IgA1 (Gd-IgA1). However, the mechanism of glomerular IgA deposition in patients with IgA-IRGN is unclear. Therefore, we evaluated whether Gd-IgA1 could be a useful biomarker to distinguish between these 2 diseases.
Methods: A case-control study was conducted to analyze the clinical and pathological characteristics of 12 patients with IgA-IRGN. The intensity and distribution of glomerular Gd-IgA1 (KM55) staining in renal biopsies were assessed. The control group consisted of 15 patients diagnosed with IgAN and an additional 17 patients with glomerulopathy involving IgA deposition.
Results: The main clinical manifestations of patients with IgA-IRGN were nephrotic-range proteinuria, hematuria, acute renal injury, and hypocomplementemia. Active lesions were the leading pathological feature, while focal segmental sclerosis was rare. Half of the patients exhibited hump-shaped subepithelial deposits. Glomerular KM55 staining was negative in 7 patients, trace in 4 patients, and 2+ in 1 patient. The median intensity of KM55 staining in IgA-IRGN patients was 0 (range 0∼2+), which was significantly lower than that of primary IgAN patients (median 2+, range 1+∼3+). The receiver operating characteristic analysis demonstrated that the optimal cutoff level to identify these 2 diseases was 0.5+.
Conclusions: Glomerular KM55 staining intensity might be helpful to distinguish IgA-IRGN from primary IgAN. Weak or negative staining may favor IgA-IRGN. In addition, integrated analysis including clinical data, pathological findings, and prognostic information would further improve the differential diagnosis.
Read abstract on library site Access full article