Factors Affecting the Progression of Infection-Related Glomerulonephritis to Chronic Kidney Disease
Factors Affecting the Progression of Infection-Related Glomerulonephritis to Chronic Kidney Disease
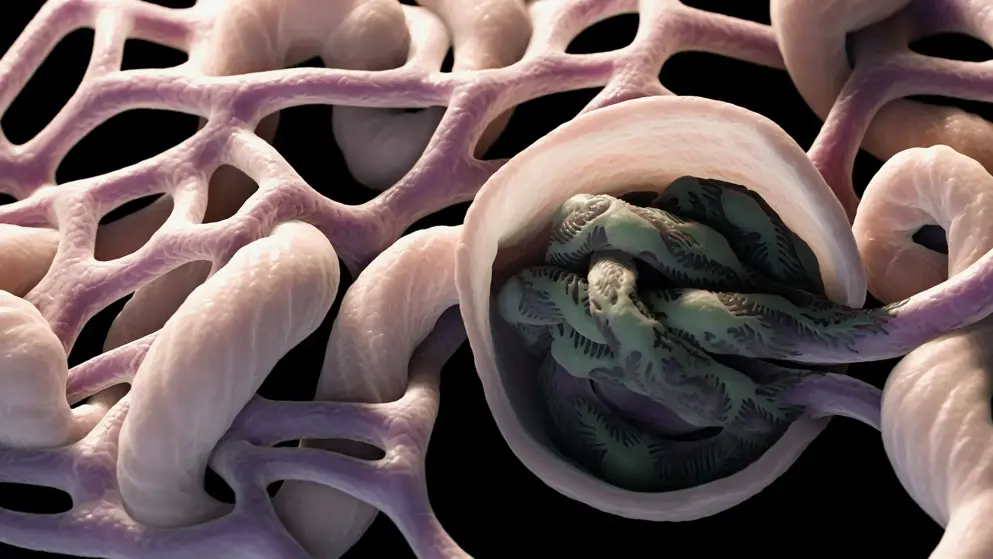
Acute glomerulonephritis (AGN) triggered by infection is still one of the major causes of acute kidney injury. During the previous two decades, there has been a major paradigm shift in the epidemiology of AGN. The incidence of poststreptococcal acute glomerulonephritis (PSAGN), which develops after the cure of group A Streptococcus infection in children has decreased, whereas adult AGN cases have been increasing, and those associated with nonstreptococcal infections, particularly infections by Staphylococcus, are now as common as PSAGN. In adult AGN patients, particularly older patients with comorbidities, infections are usually ongoing at the time when glomerulonephritis is diagnosed; thus, the term "infection-related glomerulonephritis (IRGN)" has recently been popularly used instead of "post-infectious AGN". The prognosis of children with PSAGN is generally considered excellent compared with that of adult IRGN cases. However, long-term epidemiological analysis demonstrated that an episode of PSAGN in childhood is a strong risk factor for chronic kidney disease (CKD), even after the complete remission of PSAGN. Although the precise mechanism of the transition from IRGN to CKD remains unknown, its clarification is important as it will lead to the prevention of CKD. In this review, we therefore focus on the possible factors that may contribute to the progression of IRGN into CKD. Four factors, namely, persistent infection, genetic background of the host's complement system, tubulointerstitial changes, and pre-existing histological damage, are discussed.
Read abstract on library site Access full article