Epidemiology, pathogenesis, treatment and outcomes of infection-associated glomerulonephritis
Epidemiology, pathogenesis, treatment and outcomes of infection-associated glomerulonephritis
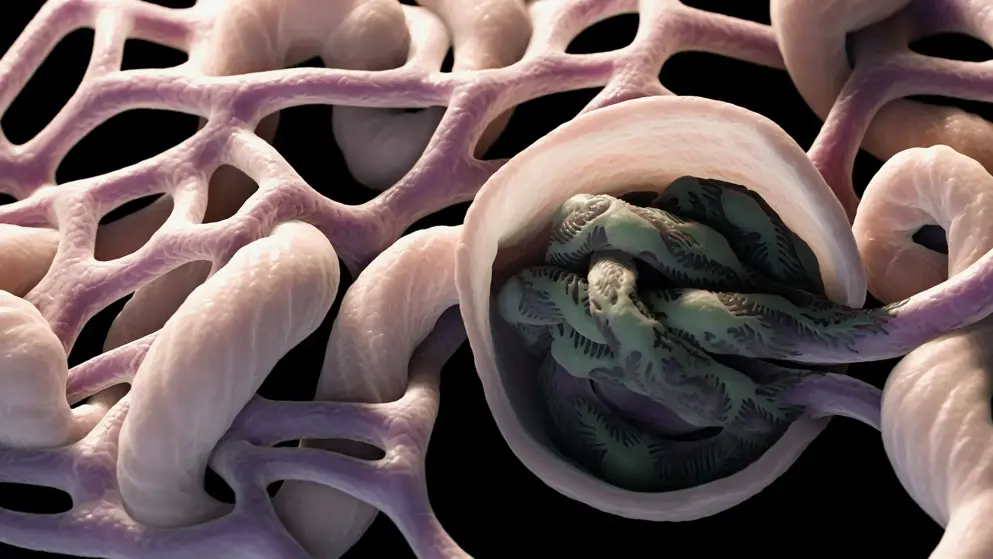
For over a century, acute ‘post-streptococcal glomerulonephritis’ (APSGN) was the prototypical form of bacterial infection-associated glomerulonephritis, typically occurring after resolution of infection and a distinct infection-free latent period. Other less common forms of infection-associated glomerulonephritides resulted from persistent bacteraemia in association with subacute bacterial endocarditis and shunt nephritis. However, a major paradigm shift in the epidemiology and bacteriology of infection-associated glomerulonephritides has occurred over the past few decades. The incidence of APSGN has sharply declined in the Western world, whereas the number of Staphylococcus infection-associated glomerulonephritis (SAGN) cases increased owing to a surge in drug-resistant Staphylococcus aureus infections, both in the hospital and community settings. These Staphylococcus infections range from superficial skin infections to deep-seated invasive infections such as endocarditis, which is on the rise among young adults owing to the ongoing intravenous drug use epidemic. SAGN is markedly different from APSGN in terms of its demographic profile, temporal association with active infection and disease outcomes. The diagnosis and management of SAGN is challenging because of the lack of unique histological features, the frequently occult nature of the underlying infection and the older age and co-morbidities in the affected patients. The emergence of multi-drug-resistant bacterial strains further complicates patient treatment.
Read abstract on library site Access full article