Nephrology
Browse a range of interactive resources, including expert interviews and patient case animations, plus highlights from recent congresses.
Medical conditions
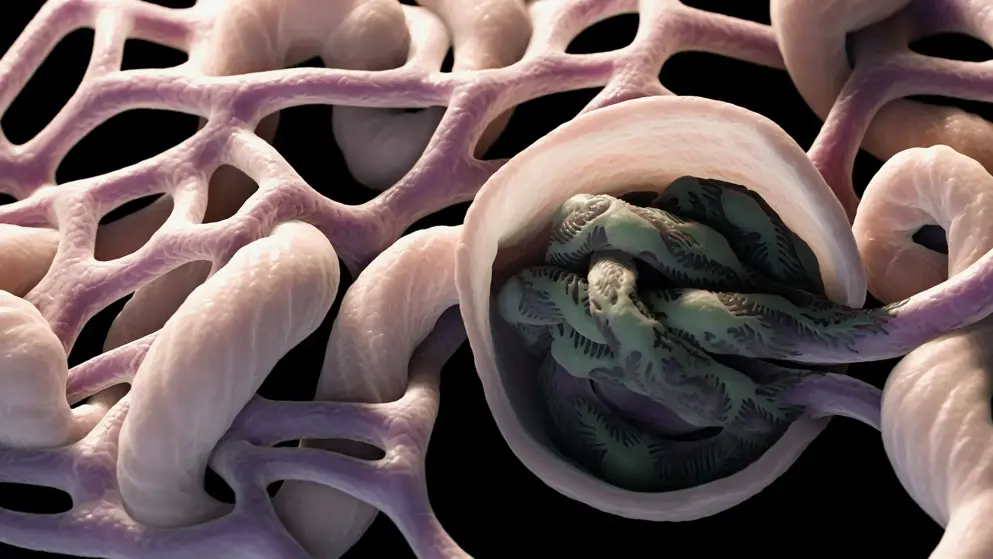
Chronic kidney disease
Expert insights on diagnosis and novel treatments
Glomerulonephritis
Unmet needs, latest news, and guideline updates
Hyperkalemia
Disease information, latest news, and guidelines
Lupus
Expert congress highlights and disease awareness
Polycystic kidney disease
Latest news, insights, and guideline updates