Respiratory medicine
This specialty hub covers a range of topics, from obstructive sleep apnea to tobacco dependency, and includes expert opinion, guideline updates, and treatment strategies.
Medical conditions
Allergic rhinitis
Latest news, insights, and guideline updates
Asthma
Latest news, insights, and guideline updates
Chronic cough
Latest news, insights, and guideline updates
COPD
Latest news, insights, and guideline updates
Cystic fibrosis
Latest news, insights, and guideline updates
Idiopathic pulmonary fibrosis
Latest news, insights, and guideline updates
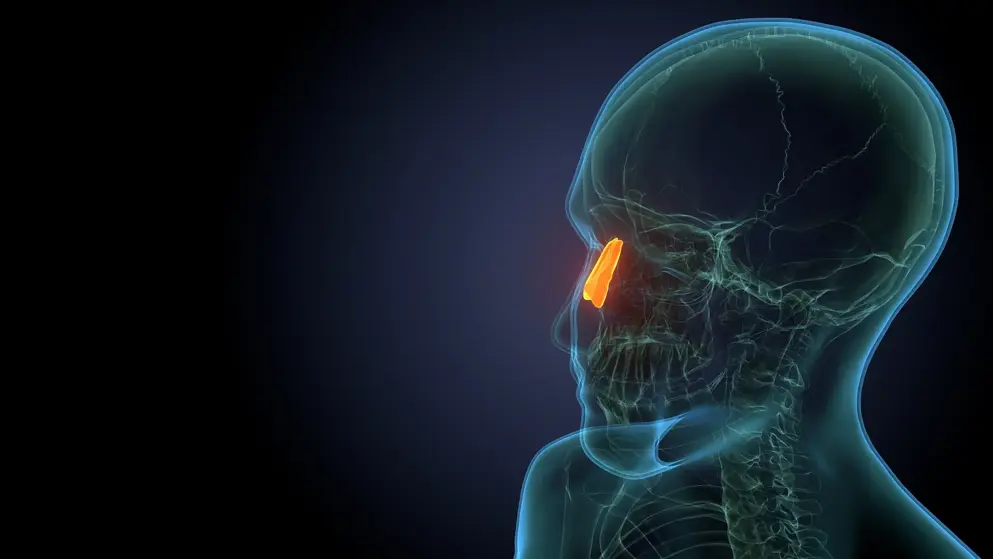
Nasal polyposis
Disease information and guideline updates
Respiratory syncytial virus
Latest news, insights, and take our quick quiz
Sleep apnea
Latest insights and spotlight article
Smoking cessation
Patient case studies and expert opinions
Latest resources
TK2d symposium
Gain expert insights into diagnosing and treating thymidine kinase 2 deficiency in pediatric patients.
Smartwatch can detect sleep apnea
How does it compare to polysomnography? Read about the evidence and potential benefits of Samsung’s sleep apnea feature.
Respiratory syncytial virus quiz
What are the risk factors and management recommendations for severe RSV infection? Who does the disease normally affect? Find out by taking this quiz and learn more with additional content on Medthority.
Browse older resources
Idiopathic Pulmonary Fibrosis
Find out more about IPF in the disease awareness section, such as epidemiology, pathophysiology, symptoms and diagnosis. Learn about the latest interventions available for patients in the treatment section, including treatment pathways and guideline recommendations.
Respiratory Syncytial Virus (RSV) in Adults
Learn more about respiratory syncytial virus (RSV) in adults. Explore RSV diagnosis, management, treatment and the burden of RSV on the patient.
Very Brief Advice for Tobacco Dependency
Are you giving VBA? Very Brief Advice on smoking (VBA) is designed to be used by primary care physicians to raise the subject of stopping smoking and encourage an attempt.
of interest
are looking at
saved
next event