Disease Management
There will be details of blood coagulation factors II, VII, IX and more; the coagulation cascade; haemorrhagic risk assessment, using the international normalised ratio; the factor Xa inhibitors rivaroxaban, edoxaban or apixaban; the factor IIa (thrombin) inhibitor dabigatran; the risks of warfarin treatment; current national and international guidelines; the use of fresh frozen plasma to reverse vitamin K antagonist (VKA) anticoagulation; plasma and rVIIA; and details of the anticoagulation reversal agents idarucizumab, andexanet alpha and ciraparantag are all included in this section.
Blood Coagulation
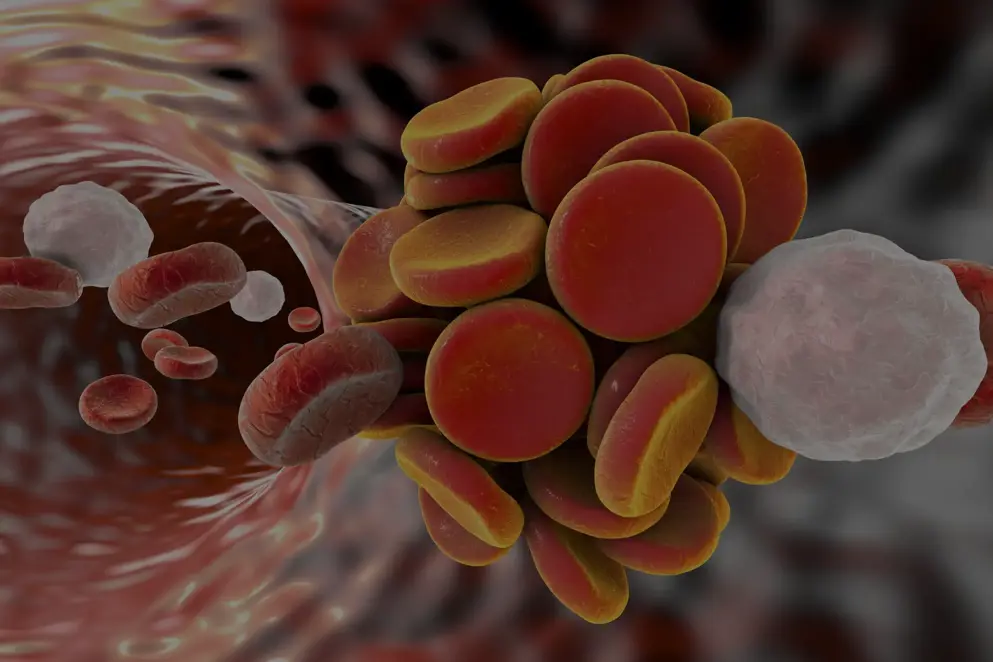
Blood coagulation involves the complex interaction of multiple factors resulting in the generation of an insoluble fibrin clot. Classically blood coagulation was considered to be a cascade involving two convergent pathways: the intrinsic (contact activation) pathway and the extrinsic (tissue factor) pathway. [Monroe and Hoffman 2006; Adams and Bird 2009; Alquwaizani et al., 2013] More recently, blood coagulation is considered to consist of phases, involving initiation, amplification, propagation and finally, clot stabilisation. [Monroe and Hoffman 2006; Adams and Bird 2009] {Figure 1}
A feature of blood coagulation is the activation of multiple inert proenzymes and cofactors (indicated by “a” after the clotting factor numeral), with binding to cell surfaces localising these factors and enzymatic reactions. In the initiation phase, a complex of the transmembrane glycoprotein tissue factor and activated factor VII (FVIIa) activates factors IX and X. Factor Xa, which is bound to tissue factor expressing cells such as fibroblasts and platelets, then generates a small amount of thrombin (FIIa) from prothrombin (FII). The amplification phase involves thrombin activation of platelets, and also of platelet-bound factors V, VIII and XI. This generates increasing amounts of thrombin required for the propagation phase in which fibrin is generated by the catalysis of fibrinogen. A stable fibrin clot is formed following cross linkage of fibrin polymers with factor XIIIa. [Monroe and Hoffman 2006; Adams and Bird 2009]
Figure 1. Outline of the phases of blood coagulation. (CSL Behring, based on Monroe and Hoffman, 2006).
TF, tissue factor; vWF, von Willebrand factor.
of interest
are looking at
saved
next event
Anticoagulation
Coagulation is a rapid and tightly controlled process giving a response to tissue injury and allowing for repair to begin. However, in some acquired or inherited clinical disorders, the coagulation process is aberrantly activated, causing thrombosis. Patients needing anticoagulation therapy for the prevention or treatment of thrombosis have commonly been treated with the oral vitamin K antagonist warfarin, or parenterally with a heparin formulation [Harter et al., 2015]. Coumarin-based oral anticoagulants, which include warfarin, phenprocoumon and acenocoumarol, are used prophylactically for venous thromboembolism, systemic embolism in patients with atrial fibrillation or prosthetic heart valves, acute myocardial infarction in patients with peripheral arterial disease, and stroke or recurrent infarction in patients with acute myocardial infarction. [Ansell et al., 2004; Ansell et al., 2008 Levy et al., 2008]
As a result of warfarin’s narrow therapeutic index and a need for frequent laboratory monitoring during warfarin therapy, novel anticoagulants have been developed in recent years. [Harter et al., 2015] The targets of anticoagulant drugs are variable and are summarised in figure 2 below. Warfarin inhibits the synthesis of functional vitamin K dependent clotting factors II (prothrombin), VII, IX and X (and protein S and protein C which have an anticoagulant regulatory function); rivaroxaban, apixaban and edoxaban are direct inhibitors of factor Xa; and thrombin (factor IIa) inhibitors include the orally administered dabigatran, and the parenteral inhibitors argatroban and bivalirudin. In contrast, unfractionated heparin (UFH) and low molecular weight heparins (LMWH) enhance the activity of antithrombin 3 (AT3), an inhibitor of thrombin and other procoagulant factors. [Hirsh et al., 2003; Alquwaizani et al., 2013; Harter et al., 2015]
Figure 2. The coagulation cascade outlining the interaction with anticoagulants. (Alquwaizani et al., 2013).
LMWH, low-molecular-weight heparins; UFH, unfractionated heparin.
Haemorrhage is an adverse event common to all anticoagulants. [Harter et al., 2015], with acute gastrointestinal (GI) bleeding being the most common adverse event associated with oral anticoagulant therapy. [Radaelli et al., 2015] In clinical practice, major bleeding can be associated with a significant risk of death resulting from intracerebral bleeding or significant GI bleeding; long-term morbidity such as intraocular bleeding or a less severe intracerebral haemorrhage; or bleeding requiring transfusion to maintain an adequate haemoglobin value. [Crowther & Warkentin 2008]
Anti-platelet drugs such as aspirin and clopidogrel are used to prevent cardiovascular disease [Steinhubl et al., 2009] but are associated with bleeding complications such as intracerebral haemorrhage. [Batchelor and Grayson 2012; Suzuki et al., 2014] Anti-platelet drug administration was identified as an independent risk factor for death from intracerebral haemorrhage. [Suzuki et al., 2014] Platelet transfusion is used to reverse the effects of anti-platelet agents, although a meta-analysis of six small studies showed no clear benefit in survival of a platelet transfusion to patients with intracerebral haemorrhage associated with anti-platelet drugs (Odds ratio (OR)=0.77, 95% confidence intervals (CI), 0.41–1.44). [Batchelor and Grayson 2012]
A recent phase 3 trial (Netherlands Trial Register, number NTR1303) comparing platelet transfusion with standard care to reverse spontaneous cerebral haemorrhage associated with anti-platelet therapy concluded that platelet transfusion was inferior to standard care and was not recommended as a therapeutic option. The primary outcome was death or dependence assessed using the modified Rankin Scale at 3 months. The odds of death or dependence were higher in the platelet transfusion group (n=97) than in the standard care group (n=93) (adjusted common odds ratio=2·05; 95% CI 1.18-3.56; P=0·011). [Baharoglu et al. 2016]
of interest
are looking at
saved
next event
Diagnostic Tests
In patients taking oral vitamin K antagonist (VKA) anticoagulants, haemorrhagic risk is assessed by the international normalised ratio (INR) which standardises the prothrombin time (PT), with risk of bleeding increasing exponentially at INR values >5.0. {Figure 3} [Landefeld and Beyth 1993; Cannegieter 1995; Palareti 1996; Makris and Watson 2001]
Figure 3. Bleeding risk in relation to international normalised ratio (INR) (Adapted from: Palareti, 1996; Makris and Watson, 2001).
UK and USA guidelines for the optimal use of oral VKA anticoagulation for a range of indications have been published and recommend a target INR within the range of 2.0–3.0, although this can be adjusted based on individual patient circumstances. [Keeling et al., 2011; Holbrook et al., 2012]
In contrast, no routine monitoring of the factor Xa inhibitors rivaroxaban, edoxaban or apixaban or the factor IIa (thrombin) inhibitor dabigatran is required, since they are given at fixed doses and have predictable pharmacokinetic and pharmacodynamic responses (in patients with adequate renal function who are not taking other interacting drugs). [Steffel et al., 2018] However, monitoring of these anticoagulants is necessary in a range of circumstances including bleeding, perioperative management, reversal of anticoagulation, and suspicion of overdose. [Baglin et al., 2013]
The PT is relatively insensitive to dabigatran and the INR is not suitable for measurement of the factor IIa inhibitor. However, the thrombin time (TT) is sensitive to dabigatran's antithrombin effect, with methods establishing a linear concentration response relationship over the therapeutic range of the drug. Guidelines recommend use of the activated partial thromboplastin time (APTT) to determine the degree of anticoagulation by dabigatran in an emergency or urgent clinical situation. [Baglin et al., 2013]
Recommendations suggest using the PT assay with a plain thromboplastin for determining the relative intensity of anticoagulation caused by rivaroxaban in an emergency or urgent clinical situation. [Baglin et al., 2013]
of interest
are looking at
saved
next event
Bleeding Risks of Anticoagulants
As with all therapies, there are sometimes serious side effects. When treating with anticoagulation therapy, monitoring is essential to ensure that the anticoagulant effects are not detrimental to patients' health. Risk of haemorrhage is likely if there is a high level of anticoagulant within the blood stream. It is all about creating a fine pharmacokinetic balance, however if the patient is in danger of haemorrhage there are oral anticoagulation reversal treatments that should be administered urgently.
Vitamin K Antagonists
The main determinants of bleeding induced by VKA therapy are the intensity of the anticoagulant effect, duration of therapy, underlying patient characteristics including age, and the concomitant use of interfering drugs. [van der Meer et al., 1993; Levine et al., 2004]
Clinical trials have reported that warfarin treatment is associated with a significant risk of haemorrhage, with the risk of fatal or life-threatening bleeding as high as 1–3% per year. [Lankiewicz et al. 2006] In randomised trials of VKA therapy following an acute episode of ischaemic cerebrovascular disease, the risk of major bleeding, assessed from multiple studies, ranged from 2–13% with a mean duration of follow-up ranging from 6 to 30 months. [Levine et al., 2004] The risk per year of major bleeding following VKA therapy in these randomised trials ranged from 1–8.3% in patients with prosthetic heart valves; 0–6.6% in patients with atrial fibrillation (AF); 0–19.3% in patients with ischaemic heart disease; and 0–16.7% in patients with venous thromboembolism (VTE) [Levine et al., 2004]
Improved rates of major haemorrhage are achieved when patients are treated by specialist anticoagulation management service (AMS) teams rather than by a personal physician. Rates of major haemorrhage were 2.8–8.1% per patient-year of therapy for care by personal physicians (usual care) and 1.4–3.3% per patient-year of therapy for care provided by AMS. [Ansell et al., 2008]
In recent years, the use of oral anticoagulants, especially vitamin K antagonists, has increased the incidence of coagulopathy-associated intracranial haemorrhage, and accounts for up to 15% of all cases [de Oliveira Manoel et al., 2016]. A meta-analysis review of data from 20 randomised clinical trials (RCTs) of 91,671 atrial fibrillation patients reported a greater risk of intracranial haemorrhage in patients treated with warfarin compared to those treated with the NOACs edoxaban (30 mg, OR 3.42, 95% CI 1.22-7.22) and dabigatran (110 mg, OR 3.56, 95% CI 1.10-8.45). [Xu et al., 2017]
A recent multicentre study of 2,192 patients taking oral anticoagulants, including warfarin, who developed major bleeding requiring hospitalisation reported high rates of mortality in these patients, with 21% likely to die within 30 days of admission, rising to 33% for patients with intracranial haemorrhage. [Green et al., 2018]
The incidence of bleeding defined as "major" or "minor" has varied considerably between studies. [Hanley 2004] This may be due, in part at least, to the inconsistency of definitions between classification schemes in clinical research studies. [Ansell et al., 2004]
Non-Vitamin K Oral Anticoagulants
The majority of studies report that the risk of gastrointestinal (GI) bleeding with non-vitamin K oral anticoagulants (NOACs) is similar to that with warfarin [Abraham et al., 2015; Chang et al., 2015; Caldeira et al., 2015; Burr et al., 2017]; although one study comparing dabigatran with warfarin reported an increase in GI bleeding and major bleeding with dabigatran [Hernandez et al., 2015], and another reported that dabigatran reduced rates of morbidity and mortality in elderly patients compared with warfarin. [Graham et al., 2015]
The overall risk of GI bleeding associated with the novel oral anticoagulants, dabigatran and rivaroxaban was found to be similar to that for warfarin in new users of these anticoagulants. However, there was an increased risk of GI bleeding in older patients aged over 75 years, in patients taking dabigatran or rivaroxaban. [Abraham et al., 2015] A recent literature review by Cheung and Leung reported an increased risk of GI bleeding with high-dose dabigatran (150 mg bid), rivaroxaban and high-dose edoxaban (60 mg daily). [Cheung & Leung, 2017]
In patients with AF the incidence of GI bleeding events associated with dabigatran was calculated as 2.29 per 100 patient years (95% CI, 1.88–2.79); and with warfarin as 2.87 per 100 patient years (95% CI, 2.41–3.41). The incidence of GI bleeding in AF patients treated with rivaroxaban was 2.84 per 100 patient years (95% CI, 2.30–3.52); and with warfarin was 3.06 per 100 patient years (95% CI, 2.49–3.77). In non-atrial fibrillation patients, the incidence of GI bleeding with dabigatran was 4.10 per 100 patient years (95% CI, 2.47–6.80); in comparison with 3.71 per 100 patient years (95% CI, 2.16–6.40) with warfarin. The incidence of GI bleeding in non-atrial fibrillation patients was 1.66 (95% CI, 1.23–2.24) per 100 patient years with rivaroxaban; and 1.57 per 100 patient years (95% CI, 1.25–1.99) with warfarin. [Abraham et al., 2015]
The risk of GI bleeding in AF patients aged ≥76 years was higher in patients taking dabigatran than warfarin: with a calculated hazard ratio (HR) of 2.49 (95% CI, 1.61 to 3.83). In ≥76 years old patients taking rivaroxaban there was a higher risk of GI bleeding compared to warfarin in both patients with AF (HR = 2.91; 95% CI, 1.65 to 4.81) and in non-atrial fibrillation patients (HR = 4.58; 95% CI, 2.40 to 8.72). [Abraham et al., 2015]
A large retrospective cohort study of over 46,000 patients treated with dabigatran, rivaroxaban or warfarin found that the rate of Gl bleeding was highest in dabigatran users (9.01/100 person years), and lowest in rivaroxaban users (3.41/100 person years), with the rate being 7.02 per 100 person years with warfarin. However, following adjustment for potentially confounding factors there was no significant difference between dabigatran or rivaroxaban when compared to warfarin. [Chang et al., 2015]
Recent meta-analyses of the risk of major GI bleeding with NOACs which evaluated studies of apixaban, dabigatran, edoxaban and rivaroxaban concluded that these drugs are not associated with an increased risk of GI bleeding when compared to other anticoagulants (VKAs or LMW heparin). [Caldeira et al., 2015]
Evaluation of five randomised controlled trials (RCTs) of nearly 73,000 patients with AF which compared NOACs with VKAs, showed that there was no association of increased risk of major GI bleeding with NOACs (estimated risk ratio (RR) = 1.08, 95% CI, 0.85–1.36). A total of nearly 30,000 patients with VTE evaluated in seven RCTs produced a RR of 0.77 (95% CI, 0.49–1.21) for a risk of major GI bleeding when comparing NOACs with VKAs (with or without the initial treatment with LMW heparin). Similarly, the risk of major GI bleeding was not significantly different for a comparison of NOACs with LMW heparin in 27,371 patients (eight RCTs) undergoing major orthopaedic surgery for the prevention of thrombosis. [Caldeira et al., 2015]
A retrospective cohort study, reported that the risk of bleeding with dabigatran use (n = 1302) in AF patients was generally higher than that with warfarin use (n = 8102). Hazard ratios for bleeding associated with dabigatran compared to warfarin were 1.58 (95% CI, 1.36–1.83) for major bleeding; 1.85 (95% CI, 1.64–2.07) for GI bleeding; and 1.30 (95% CI, 1.20–1.41) for any bleeding event. However, the risk of intracranial haemorrhage was higher in warfarin users, with a hazard ratio of 0.32 (95% CI, 0.20–0.50) for dabigatran compared with warfarin. [Hernandez et al., 2015]
Comparison of dabigatran with warfarin in 134,414 elderly patients aged ≥65 years reported reduced rates of morbidity and mortality with dabigatran. Hazard ratios comparing dabigatran with warfarin were 0.80 (95% CI, 0.67–0.96) for ischaemic stroke; 0.34 (95% CI, 0.26–0.46) for intracranial haemorrhage; 1.28 (95% CI, 1.14–1.44) for major GI bleeding; 0.92 (95% CI, 0.78–1.08) for acute myocardial infarction; and 0.86 (95% CI, 0.77–0.96) for death. [Graham et al., 2015]
of interest
are looking at
saved
next event
Disease Burden and Treatment
Disease burden
A retrospective analysis of data from patients with AF treated from 2003 to 2007 in the USA showed that the mean costs of warfarin-associated bleeding were $41,903 for intracranial haemorrhage, and $40,586 and $24,347 for major and minor GI bleeding respectively. [Ghate et al., 2011]
Treatment
Clear strategies to swiftly and completely reverse oral anticoagulation, especially in patients experiencing a serious bleed are imperative. [Hirsh 2003; Hanley 2004] In addition, anticoagulated patients who require emergency surgery or invasive diagnostic procedures, or those with very high INRs, are also candidates for urgent anticoagulation reversal. [Hirsh et al., 2003; Hanley 2004]
For patients anticoagulated with VKAs with a high INR three options exist to lower the INR. The first is to cease warfarin therapy; the second is to administer vitamin K; and the third, for an effective rapid response, is to infuse fresh plasma or prothrombin complex concentrate. Normalisation of high INRs following cessation of warfarin therapy commonly takes several days to achieve, with INRs being normalised within 24 hours following addition of vitamin K. More rapid reversal with fresh frozen plasma or prothrombin complex concentrates will typically normalise INR within an hour. [Hirsh 2003; Hanley 2004; Imberti et al., 2011]
Vitamin K Antagonist Associated Bleeding
Vitamin K Antagonist Associated Bleeding
Bleeding is the most significant adverse effect with warfarin therapy, being directly related to the level of INR. Warfarin has a narrow therapeutic index and is influenced by drug interactions, notably anti-platelet drugs, and environmental factors. Treatment with VKAs increases the risk of major bleeding by 0.3–0.5 % per year and the risk of intracranial haemorrhage by around 0.2 % per year in comparison to controls. [Alquwaizani et al., 2013; Harter et al., 2015]
Risk factors for warfarin-related haemorrhage include intensity of anticoagulant effect, time within the therapeutic range, advanced age, and serious comorbid conditions including cancer, prior stroke, chronic kidney disease (CKD), liver dysfunction, arterial hypertension and alcohol abuse. [Alquwaizani et al., 2013; Harter et al., 2015]
Current Guidelines
Guidelines have been published by the American College of Chest Physicians (ACCP) for the perioperative management of antithrombotic therapy, which addresses the management of patients who are receiving VKA anticoagulant therapy and require an elective surgery or procedure. Assessment of perioperative bleeding risk is considered but no guidance on reversal of bleeding associated with VKAs is provided. [Douketis et al., 2012]
European Society of Cardiology (ESC) guidelines for the management of AF which were updated in 2016, include antithrombotic management of patients using VKA anticoagulant therapy. These guidelines include the use of NOACs for antithrombotic therapy (See Bleeding associated with NOACs; guidelines). Although bleeding risk is assessed, no guidance on reversal of bleeding with anticoagulants is provided. [Kirchhof et al., 2016]
American College of Chest Physicians (ACCP) guidelines for the evidence-based management of anticoagulant therapy include recommendations for the prevention and management of bleeding complications with VKAs. These include the use of four-factor (4F) PCCs (Prothrombin complex concentrates), rather than plasma for major bleeding associated with VKAs. [Holbrook et al., 2012]
European Society of Anaesthesiology guidelines for the management of severe perioperative bleeding recommends that patients on oral anticoagulant therapy should be given prothrombin complex concentrate (PCC) and vitamin K before any other coagulation management steps for treating severe perioperative bleeding. [Kozek-Langenecker et al., 2017]
European guidelines for the management of bleeding and coagulopathy following major trauma recommend the early use of PCC for the emergency reversal of VKAs. [Roussaint et al., 2016]
Guidelines for the reversal of antithrombotics in intracranial haemorrhage have recently been published by the Neurocritical Care Society and Society of Critical Care Medicine. [Frontera et al., 2016]
Prothrombin Complex Concentrates
A number of randomised controlled trials (RCTs) have been conducted on the use of PCCs for VKA reversal. PCCs contain varying amounts of vitamin K dependent coagulation factors II, VII, IX and X. Literature reports suggest that 3-PCC may be less effective than 4-PCC in warfarin reversal, due to a lower factor VII content. [DeAngelo et al., 2017; Holt et al., 2018]
A prospective study of 43 patients requiring emergency VKA reversal (26 required interventional procedures and 17 experienced acute bleeding) received an infusion of 4-factor (4F) PCC which contains coagulation factors II, VII, IX, and X, and the anticoagulant proteins C and S. PCC infusion at a median rate of 7.5 mL/min (188 IU/min), produced a decline in INR to <1.3 in 93% of patients. Normalisation of INR was sustained for 48 hr post PCC infusion with median INR values of 1.2–1.3 being attained. There was a marked increase in coagulation factors II, VII, IX, and X and the thrombo-inhibitor proteins C and S following PCC infusion within 30 min, with levels of these coagulation factors and proteins C and S remaining at normal or near normal levels over the next 48 hours. One serious adverse event (SAE) possibly related to PCC was a suspected pulmonary embolism resulting in the death of a patient (aged 70 years with metastatic cancer), while five other SAEs were judged to be unrelated to PCC. [Pabinger et al., 2008]
Rapid infusion of PCC, with infusion rates varying from 2.0 to 40.0 mL/min (median of 7.5 mL/min), did not compromise its safety or efficacy, when used for emergency VKA reversal in 43 patients. [Pabinger 2010]
A retrospective study of VKA reversal using PCC treatment evaluated case notes from 50 surgical patients requiring reversal of an oral VKA (n=12) or with severe coagulopathic perioperative bleeding (n=38). Following PCC infusion in VKA reversal patients baseline INR was significantly reduced from 2.8±0.2 to 1.5±0.1 (p<0.001). In bleeding patients, PCC infusion significantly reduced the INR from 1.7±0.1 at baseline to 1.4±0.1 (p<0.001), with no major bleeding occurring during subsequent surgery. [Schick et al., 2009]
A randomised study of PCC and fresh frozen plasma (FFP) for the reversal of VKAs in 40 patients undergoing cardiopulmonary bypass surgery showed that 15 min after surgery significantly more patients reached INR target with PCC (7/16) than FFP (0/15; p=0.007). This difference was not apparent 1 hour after surgery. The safety profile was good for both treatment groups, with minor bleeding reported for two cases in the FFP group. [Demeyere et al., 2010]
A three-factor (3F) PCC was effective in the emergency reversal of VKA anticoagulation (warfarin or acenocoumarol) in 46 patients with intracranial haemorrhage. Patients had a median INR at presentation of 3.5 (INR range 2–9), and at 30 minutes following PCC infusion median INR values were significantly reduced to 1.3 (range, 0.9–3; p<0.0001). INRs declined to <1.5 in 75% of patients – the primary end-point of the study. [Imberti et al., 2011]
Two RCTs compared 4F-PCC (containing vitamin K–dependent factors plus proteins C and S) with plasma in patients receiving VKAs and presenting with acute major bleeding [Sarode et al., 2013 {NCT00708435}], or in need of urgent surgical or invasive procedures. [Goldstein, et al., 2015 {NCT00803101}]
A randomised, plasma-controlled, phase III study of 4F-PCC in 202 patients on VKAs presenting with acute major bleeding showed that 4F-PCC was non-inferior to plasma for haemostatic efficacy. Effective haemostasis was achieved in 72.4% of patients receiving 4F-PCC and 65.4% receiving plasma (difference=7.1%; 95% CI, –5.8 to 19.9). 4F-PCC was superior to plasma for rapid INR reduction (INR ≤1.3 at 30 min after end of infusion) with 62.2% of patients receiving 4F-PCC and 9.6% receiving plasma achieving this goal (difference=52.6%; 95% CI, 39.4 to 65.9). The safety profile was similar between treatment groups with 64.1% (66 of 103) in the 4F-PCC group and 65.1% (71 of 109) in the plasma group of patients experiencing ≥1 adverse event. Thromboembolic AEs were reported in 8 patients in the 4F-PCC group and 7 in the plasma group. [Sarode et al., 2013 {NCT00708435}]
4F-PCC was superior to plasma for the primary endpoint of haemostasis (90% vs. 75%; difference = 14.3%, 95% CI, 2.8–25.8; p=0·014) in the second randomized controlled trial in 168 patients on VKAs needing urgent reversal prior to surgery or an invasive procedure. [Goldstein et al 2015] The co-primary endpoint of rapid INR reduction (INR ≤1.3 at 30 min after end of infusion) also showed superiority of 4F-PCC over plasma (55% vs. 10%; difference = 45.3%, 95% CI, 31.9–56.4; p<0·0001). The safety profile was generally similar in both groups: 56% of patients receiving 4F-PCC had adverse events compared with 60% patients receiving plasma; fluid overload occurred less frequently in patients receiving 4F-PCC (3% vs 13%). [Goldstein, et al., 2015]
An analysis of pooled data from these two studies [Sarode et al., 2013; Goldstein, et al., 2015] showed that 7.3% (14 of 191) patients in the 4F-PCC group and 7.1% (14 of 197) in the plasma group developed thromboembolic events after VKA reversal (risk difference 0.2%; 95% CI, -5.5% to 6.0%). Serious adverse events were reported in 16 patients, 8 in each group. [Milling et al., 2016] Fluid overload events occurred more frequently in the plasma group than the 4F-PCC group (25 [12.7%] and 9 [4.7%], respectively).
A pharmacovigilance study of the long-term safety (15 years) and efficacy of a 4F-PCC showed that the incidence of thromboembolic events was approximately one in 31,000, with 21 thromboembolic events possibly related to 4F-PCC administration in ~647,250 standard applications of the 4F-PCC being reported. No cases of viral transmission or heparin-induced thrombocytopaenia were documented. The incidence rate of thromboembolic events is comparable to those observed with other 4F-PCCs. [Hanke et al., 2013]
A systematic review of reversal of VKA treatment by PCCs in bleeding and non-bleeding patients identified four RCTs [Boulis et al., 1999; Demeyere et al., 2010; Sarode et al., 2013; Majeed et al., 2014] with a total of 453 participants. Three of the trials provided data on mortality, with a meta-analysis of the effect of PCCs on overall mortality showing no statistical effect (Relative Risk (RR) = 0.93, 95% CI, 0.37–2.33) although the quality of evidence was judged to be very low due to the high risk of bias and underpowered nature of the trials reviewed. [Johansen et al., 2015]
A recent meta-analysis of 5 randomised and 8 observational studies which compared PCC with fresh frozen plasma (FFP) for warfarin reversal concluded that PCC use significantly reduced all-cause mortality (OR=0.56, 95 % CI, 0.37–0.84, p=0.006), produced a more rapid INR reduction (OR=10.80, 95 % CI, 6.12–19.07), with less volume overload (OR=0.27, 95 % CI, 0.13–0.58) and without an increased risk of thromboembolic events (OR=0.91, 95 % CI, 0.44–1.89). [Chai-Adisaksopha et al., 2016]
The effect of a simplified dosing protocol (RAPID) for 4F-PCC (25 IU/kg) was assessed in a retrospective audit of 17 patients with warfarin-associated bleeding. The intervention involved standardisation of the initial dose and simplification of dose calculations. Using the protocol, 15 patients with warfarin-associated bleeding (88.2%) achieved a post-treatment INR ≤1.5; with reversal of warfarin-associated bleeding within 8 h reported in 14 (82.4%). Compared with the retrospective cohort, RAPID was associated with a reduced administration interval (mean 37.7 vs 76 min, p=0.031) and an increased proportion of patients treated within 30 min (58.8 vs 6.7%, p=0.009). [Appleby et al., 2016]
The efficacy of PCC versus fresh frozen plasma has been further assessed in a retrospective chart review of 120 patients with traumatic intracranial haemorrhage. This study compared outcomes in patients with INR ≤ 1.4 after receiving activated PCC (aPCC) versus FFP within 24 hours and reported that INR was more effectively reversed in patients treated with aPCC (90.3%) versus FFP (69.7%; p=0.029). Median time to reversal (hours) was also significantly shorter with PCC vs FFP (3.75 hours vs 6.75 hours; p=0.003). Mortality rates and incidences of thrombosis did not differ between the two treatment groups. [Carothers et al., 2018]
Vitamin K & Plasma
Vitamin K
In French clinical practice guidelines, vitamin K is advocated for VKA overdose when the INR is above 6, and when bridging therapy with heparin for an elective surgical procedure is required (in patients with an INR >1.5 the evening before the procedure). It is also recommended in cases of severe bleeding, regardless of the initial INR. [Pernod et al., 2010]
American College of Chest Physicians (ACCP) guidelines suggest the administration of oral vitamin K for patients taking VKAs with INRs >10.0 and with no evidence of bleeding, but not if the INR is between 4.5 and 10. [Holbrook et al., 2012]
Reversal of anticoagulation with vitamin K is achieved more rapidly with intravenous (iv) rather than oral administration. However, in an emergency situation vitamin K treatment alone is not sufficiently rapid as it takes 4–6 hours for INR normalisation following iv administration of vitamin K. [Levy et al., 2008]
Plasma
Use of fresh frozen plasma (FFP) for reversing the effects of VKA anticoagulation is limited by the volume of plasma required to effect complete reversal. [Evans et al., 2001]
Many current guidelines, including European and American guidelines, consider that human plasma is no longer the treatment of choice to reverse VKA anticoagulation. [Board of the German Medical Association 2009; Pernod et al., 2010; Keeling et al., 2011; Holbrook et al., 2012; Roussaint et al., 2016; Kozek-Langenecker et al., 2017]
Two phase III trials comparing plasma with 4F-PCC for the rapid reversal of VKAs or in need of urgent surgical or invasive procedures showed that 4F-PCC was superior to plasma for rapid INR reversal [Sarode et al., 2013; Goldstein, et al., 2015] and effective haemostasis. [Goldstein, et al., 2015] These, and other studies, are discussed in more detail within the PCCs section.
NOACs and Associated Bleeding
In common with all anticoagulants, haemorrhage, notably gastrointestinal bleeding and intracranial haemorrhage, is the primary adverse effect with both Xa inhibitors (rivaroxaban, apixaban, edoxaban) and direct IIa inhibitors (dabigatran). [Alquwaizani et al., 2013; Harter et al., 2015]
A recent analysis of 61 patients with non-traumatic NOAC-associated intracerebral haemorrhage reported a mortality rate of 28% at 3 months, with substantial haematoma expansion occurring in 38% (17 of 45) of evaluated patients, and new or increased intraventricular haemorrhage being observed in 18% (8 of 45) of patients. [Purrucker et al. 2016]
Current Guidelines
The ESC guidelines for management of AF, published in 2012, include the use of NOACs (dabigatran, rivaroxaban or apixaban) for antithrombotic therapy. [Camm et al., 2012] Practical guidance on how to improve the implementation of the ESC guidelines for anticoagulation in AF using NOACs has recently been published. [Kirchhof et al., 2016]
Consensus European guidelines for antithrombotic therapy in non-valvular AF patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions has also recently been published. [Lip et al., 2014] Combined guidelines from multiple US organisations published in 2014 for the management of patients with AF include recommendations for risk-based anticoagulation therapy, with options for anticoagulation of non-valvular AF including the use of warfarin (INR 2.0–3.0), dabigatran, rivaroxaban or apixaban. [January et al., 2014]
Although these detailed guidelines discuss the risk of bleeding with NOACs, strategies for the reversal of bleeding associated with NOACs are not discussed, and specific reversal agents for NOACs in the event of major bleeding were not available at the time of publication. Some guidance is available for the reversal of oral IIa and factor Xa inhibitors, [Camm et al., 2012; Radaelli et al., 2015; Steffel et al., 2018]. Idarucizumab (Praxbind®) has since been approved for specific reversal of the anticoagulant action of dabigatran [European Medicines Agency, 2015a; FDA, 2015] as well as andexanet alfa for the reversal of rivaroxaban and apixaban [FDA, 2018].
An Anticoagulation Education Task Force White Paper on the management of reversal of direct oral anticoagulants in emergency situations was recently published. Recommendations are provided for situations when a reversal agent is definitely required e.g. life-threatening bleeding, bleeding into an organ or closed space, persistent bleeding despite local haemostatic measures, and the need for urgent interventions and/or interventions that carry a high bleeding risk. Conditions when a reversal agent may be helpful or is generally not needed are also considered. [Ageno et al., 2016] An algorithm for the management of bleeding and urgent surgery in patients receiving NOACs is shown in the Figure below.
Figure 4. Algorithm for management of patients treated with a NOAC who present with mild, moderate–severe, or life-threatening bleeding, or who require emergency surgery.
*Idarucizumab is the preferred treatment for dabigatran reversal [Ageno et al., 2016]
European Heart Rhythm Association (EHRA) practical guidance on the use of NOACs in patients with non-valvular AF includes the management of bleeding complications with these anticoagulants. A range of measures are suggested to combat bleeding associated with NOACs including the use of prothrombin complex concentrate (PCC) for life threatening bleeding. [Steffel et al., 2018]
European guidelines for the management of bleeding and coagulopathy following major trauma suggest the measurement of substrate-specific anti-factor Xa activity in patients treated or suspected of being treated with oral inhibitors of factor Xa (rivaroxaban, apixaban or edoxaban). High dose PCC (25 to 50 U/kg) is suggested for the reversal of rivaroxaban, apixaban and edoxaban if bleeding is life threatening. [Roussaint et al., 2016]
Proposals from a working group on perioperative haemostasis on the management of patients on long-term treatment with NOACs (dabigatran and rivaroxaban) suggest either activated prothrombin complex concentrate (aPCC) 30–50 U/kg) or non-activated PCC (50 U/kg) as first line therapy for serious bleeding. [Pernod et al., 2013; Faraoni et al., 2015]
Prothrombin Complex Concentrates
PCCs potentially have a role in the reversal of the anticoagulant effect of NOACs, although clinical data supporting this use are generally lacking. [Pengo et al., 2011; Ghanny et al., 2012; Kaatz et al., 2012; Roussaint et al., 2016; Steffel et al., 2018]
PCCs were recently recommended for the reversal of life-threatening bleeding by the Anticoagulation Education Task Force. [Ageno et al., 2016]
Preclinical studies
Animal models have illustrated the potential of PCCs to reverse the effects of NOACs:
- A porcine model of trauma showed that PCCs were effective in reducing the anticoagulant effects of dabigatran, as was idarucizumab (aDabi-Fab, [Das et al., 2015]) the specific reversal agent for dabigatran, which was the most effective agent tested. [Grottke et al., 2014]
- Rabbit models of acute bleeding have been used to assess the effect of reversal of a 4F-PCC following administration of edoxaban [Herzog et al., 2015a], rivaroxaban [Herzog et al., 2015b], dabigatran [Herzog et al., 2014] or apixaban [Herzog et al., 2015c]. The 4F-PCC was effective in significantly reducing edoxaban-associated haemorrhage [Herzog et al., 2015a]; reducing bleeding to control levels following administration of rivaroxaban [Herzog et al., 2015b]; reversing excessive bleeding following dabigatran administration whilst retaining the protective anticoagulation activity of dabigatran [Herzog et al., 2014]; and reducing bleeding time and volume following administration of apixaban. [Herzog et al., 2015c]
- Reversal of dabigatran-induced bleeding by six different coagulation factor concentrates comprising 3F-PCC, 4F-PCCs, an activated PCC and rVIIa was demonstrated in a rat-tail bleeding model. These coagulation factor concentrates significantly decreased (P<0.001) the prolonged bleeding time induced by dabigatran over 30 min, although none of the coagulation factor concentrates had a concomitant effect on coagulation assays. [van Ryn et al., 2014]
- In a porcine polytrauma model a 4F-PCC was effective in treating blood loss following dabigatran administration. Blood loss was significantly lower with 4F-PCC administered at 50 U/kg (1,749 ± 47 ml) or 100 U/kg (1,692 ± 97 ml) compared to dabigatran treated controls (3,855 ± 258 ml). [Honickel et al., 2015]
Studies in healthy human volunteers
A number of phase I studies have demonstrated the potential of PCCs for reversing the effects of anticoagulants in humans:
- Twelve healthy male volunteers received rivaroxaban or dabigatran for 2.5 days, followed by either a 50 IU/kg bolus of 4F-PCC (human plasma-derived factors II, VII, IX and X, as well as antithrombin and proteins C and S) or a saline placebo. After a washout period, the procedure was repeated with the alternate anticoagulant, again followed by 4F-PCC or saline. 4F-PCC completely reversed the anticoagulant effects of rivaroxaban, but had no influence on the effects of dabigatran. [Eerenberg et al., 2011]
- Thirty-five healthy adults received rivaroxaban for 4 days, and on day 5 received a 50 IU/kg bolus of either 3F-PCC (including factors II, IX and X), 4F-PCC (including factors II, VII, IX and X) or saline. Both PCCs showed at least partial reversal of rivaroxaban’s actions: the thrombin generation effect of rivaroxaban was more effectively reversed by 3F-PCC than 4F-PCC, while the increase in prothrombin time with rivaroxaban was more effectively reversed by 4F-PCC than 3F-PCC. [Levi et al., 2014]
- One hundred and ten healthy adults took part in a study in which they received a single dose of edoxaban followed by different doses of 4F-PCC (including factors II, VII, IX and X) or placebo. The reversal of edoxaban’s effects was observed in a dose-dependent manner, with the 50 IU/kg dose providing complete reversal of the effect on bleeding duration and endogenous thrombin potential, and partial reversal of the increased prothrombin time. [Zahir et al., 2015]
- The reversal of apixaban’s effects was investigated in a study of six healthy volunteers, given 25 IU/kg or 37.5 IU/kg doses of 4F-PCC, or saline placebo, following 3 days of apixaban treatment. Both doses of 4F-PCC at least partially restored coagulation parameters, but not to pre-apixaban levels, suggesting that the doses used were too low to fully reverse the anticoagulation effect of apixaban. [Cheung et al., 2015] Corresponding investigations by the same research group into lower doses of 4F-PCC (or placebo) on the actions of rivaroxaban in six healthy volunteers were undertaken. Results showed that both doses restored prothrombin time prolongation, but that 25 IU/kg was not different from placebo in restoring endogenous thrombin potential or thrombin generation, while 37.5 IU/kg partially restores both measures. [Barco et al., 2016]
Reports from bleeding episodes in clinical practice
A retrospective review of 18 patients treated with direct factor Xa inhibitors (n=16 with rivaroxaban; n=2 with apixaban) presenting with traumatic and spontaneous intracranial haemorrhage summarised treatment with 4F-PCC for the reversal of anticoagulation. Favourable outcomes at 90 days were observed in one third of patients (n=6). Worsening of bleeding was found in one patient; six patients (33.3%) died in hospital (four following family withdrawal of care; two due to pneumonia); and one patient had a thromboembolic complication. The use of 4F-PCC was considered to be safe. [Grandhi et al., 2015]
Analysis of 1082 bleeding events in a registry of rivaroxaban patients identified six patients whose serious bleeding events were treated with PCC (of unspecified composition); five of these showed stabilisation of haemorrhage, and four were without sequelae at 90 days post-bleeding. The patient whose haemorrhage was not stabilised was judged to have had too low a dose (18 IU/kg) and had a 5.5 hour delay from admission to PCC application; the patient with sequelae by 90 days died of septic pneumonia on day 16. [Beyer-Westendorf et al., 2014]
A recent review of PCCs and activated PCCs for the reversal of dabigatran-induced anticoagulation concluded that their use was warranted in patients with life-threatening haemorrhage if idarucizumab was unavailable. [Grottke et al., 2016]
Plasma & rVIIa
Plasma
Use of fresh frozen plasma (FFP) for reversing the effects of VKA anticoagulation is limited by the volume of plasma required to effect complete reversal. [Evans et al., 2001; Refaai et al., 2015]
Many current guidelines, including European and American guidelines, consider that human plasma is no longer the treatment of choice to reverse VKA anticoagulation. [German Medical Association 2009; Pernod et al., 2010; Keeling et al., 2011; Holbrook et al., 2012; Roussaint et al., 2016; Kozek-Langenecker et al., 2017]
Two phase III trials comparing plasma with 4F-PCC for the rapid reversal of VKAs or in need of urgent surgical or invasive procedures showed that 4F-PCC was superior to plasma for rapid INR reversal [Sarode et al., 2013; Goldstein, et al., 2015] and effective haemostasis. [Goldstein, et al., 2015] These, and other studies are discussed in more detail in the Prothrombin complex concentrates (PCCs) section.
rVIIa
Off-label use by the administration of rVIIa may be considered for bleeding which cannot be stopped by conventional means and/or there is a failure of comprehensive coagulation therapy. [Kozek-Langenecker et al., 2017] Although there is no formal review of clinical experience for NOAC reversal, anecdotal evidence for the use of rVIIa is inconsistent. [Lazo-Langner et al., 2013]
Idarucizumab
Idarucizumab is a humanised monoclonal Fab antibody fragment that specifically binds to dabigatran, thereby neutralising the anticoagulant. [Das & Liu 2015; European Medicines Agency 2015b] Idarucizumab recently received fast-track marketing authorisation from the European Medicines Agency (EMA) as a specific reversal agent for dabigatran etexilate when rapid reversal of anticoagulation is required. [European Medicines Agency 2015a]
EMA approval for idarucizumab was based on data from three placebo-controlled phase I RCTs involving 283 subjects [European Medicines Agency 2015b] including a study in healthy volunteers [Glund et al., 2015] (NCT01688830) and the RE-VERSE AD trial (NCT02104947) [Pollack et al., 2015] for the reversal of the factor IIa inhibitor, dabigatran.
The RE-VERSE AD trial included 301 patients with uncontrolled bleeding (group A), and 202 patients requiring an urgent procedure (group B), across 173 sites in 39 countries. All patients (100%) achieved complete reversal of the anticoagulant effect of dabigatran determined by diluted thrombin time (dTT) or ecarin clotting time (ECT) in the first 4 hours after administration of idarucizumab. {Figure 5 below} Reversal of anticoagulation was rapid and was independent of age, sex, renal function and dabigatran concentration at baseline. The estimated 90-day mortality rate was 18.8% in group A and 18.9% in group B. Thrombotic events were reported within 90 days in 14 patients in group A (4.8%) and in 15 patients in group B (6.8%). There were no serious adverse safety signals with most adverse events appearing to be worsening of an index event or a coexisting condition. [Pollack et al., 2017]
Figure 5. Reversal, by idarucizumab, of dabigatran-induced clotting time prolongation determined by dTT in (A) 293 patients with uncontrolled bleeding (group A) and (B) 195 patients requiring an urgent procedure (group B) from the RE-VERSE AD trial [Pollack et al., 2017].
Andexanet Alfa
Andexanet alfa is a recombinant protein that when bound, inactivates direct factor Xa inhibitors. [Das & Liu 2015] The effect of andexanet alfa for the reversal of the factor Xa inhibitors, apixaban (5 mg twice daily) or rivaroxaban (20 mg daily) was assessed in a placebo-controlled trial of healthy volunteers (aged 50–75 years) using the mean percentage change in anti–factor Xa activity (which is a measure of factor Xa inhibition by the anticoagulants) as the primary outcome. Adexanet alfa significantly reduced anti-factor Xa activity, compared to placebo, in participants treated with either apixaban (94±2% vs.21±9%; p<0.001) or rivaroxaban (92±11% vs. 18±15%; p<0.001). No serious or severe adverse events were reported, with thrombotic events being absent. All adverse events relating to andexanet administration were mild. [Siegal et al., 2015]
The single-arm open-label ANNEXA-4 trial in 228 patients experiencing acute bleeding whilst taking a factor Xa inhibitor (of which 132 patients were adjudicated for efficacy), has released early results demonstrating that andexanet alfa rapidly reversed factor Xa activity when administered as a bolus, which was sustained when followed by a 120-minute infusion. Haemostasis was achieved in 83% of these patients, whilst rates of thrombotic events (11%) and mortality (12%) were consistent with earlier study findings. Andexanet alfa gained approval from the U.S. Food and Drug Administration in 2018 and is currently under review by the European Medicines Agency. [FDA, 2018; Portola Pharmaceuticals Press Release, 2018]
Ciraparantag (Arapazine, PER977)
Ciraparantag (arapazine, PER977) is a small water-soluble molecule which binds to direct inhibitors of factor Xa and IIa, and also to heparin-based anticoagulants, thereby antagonising their effects. [Das & Liu 2015; Siegal, 2015; Milling Jr and Kaatz, 2016] The safety and efficacy of ciraparantag (5–300 mg iv) was studied following its administration to healthy people in a double-blind placebo-controlled trial who were treated with a 60 mg oral dose of the factor Xa inhibitor, edoxaban. The anticoagulant effect of edoxaban, and its reversal by ciraparantag was assessed by whole-blood clotting time (WBCT). Edoxaban increased the mean WBCT by 37% from baseline values, with a single iv dose of ciraparantag (100–300 mg) administered 3 hours post edoxaban reducing the WBCT to within 10% of baseline values in ≤10 min. In contrast, a comparable level of WBCT in patients receiving placebo was reached in approximately 12 to 15 hours. Adverse events potentially related to ciraparantag were mild. [Ansell et al., 2014] A further dose-escalation study by the same group (NCT01826266) reported that 100–300 mg ciraparantag restored haemostasis within 10–30 mins, and sustained this for 24 hours in 83 healthy subjects. [Ansell et al., 2017; US National Library of Medicine 2018)
of interest
are looking at
saved
next event
Disease Management References
Abraham NS, Singh S, Alexander GC, Heien H, Haas LR, Crown W, et al. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin. BMJ. 2015;350:h1857.
Adams RL, Bird RJ. Coagulation cascade and therapeutics update: relevance to nephrology. Part 1: Overview of coagulation, thrombophilias and history of anticoagulants. Nephrology (Carlton). 2009;14:462-70.
Ageno W, Büller HR, Falanga A, Hacke W, Hendriks J, Lobban T, et al. Managing reversal of direct oral anticoagulants in emergency situations. Anticoagulation Education Task Force White Paper. Thromb Haemost. 2016;116(6):1003-10.
Alquwaizani M, Buckley L, Adams C, Fanikos J. Anticoagulants: A Review of the Pharmacology, Dosing, and Complications. Curr Emerg Hosp Med Rep. 2013;1:83-97.
Ansell JE, Bakhru SH, Laulicht BE, Steiner SS, Grosso M, Brown K, et al. Use of PER977 to reverse the anticoagulant effect of edoxaban. N Engl J Med. 2014;371:2141-2.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G, et al. Pharmacology and management of the vitamin K antagonists: American College of Chest. Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:160S-198S.
Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:204S-33S.
Appleby N, Groarke E, Crowley M, Wahab FA, McCann AM, Egan L, et al. Reversal of warfarin anticoagulation using prothrombin complex concentrate at 25 IU kg-1 : results of the RAPID study. Transfus Med. 2016 Oct 7. doi: 10.1111/tme.12371. [Epub ahead of print]
Baglin T, Hillarp A, Tripodi A, Elalamy I, Buller H, Ageno W. Measuring Oral Direct Inhibitors (ODIs) of thrombin and factor Xa: A recommendation from the Subcommittee on Control of Anticoagulation of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2013;11:756-60.
Baharoglu MI, Cordonnier C, Salman RA, de Gans K, Koopman MM, Brand A, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016 May 9. pii: S0140-6736(16)30392-0. [Epub ahead of print]
Barco S, Cheung YW, Coppens M, Hutten BA, Meijers JC, Middeldorp S. In vivo reversal of the anticoagulant effect of rivaroxaban with four-factor prothrombin complex concentrate. Br J Haematol. 2016;172:255-61.
Batchelor JS, Grayson A. A meta-analysis to determine the effect on survival of platelet transfusions in patients with either spontaneous or traumatic antiplatelet medication-associated intracranial haemorrhage. BMJ Open. 2012;2:e000588.
Beyer-Westendorf J, Förster K, Pannach S, Ebertz F, Gelbricht V, Thieme C, et al. Rates, management, and outcome of rivaroxaban bleeding in daily care: results from the Dresden NOAC registry. Blood. 2014;124:955-62.
Boulis NM, Bobek MP, Schmaier A, Hoff JT. Use of factor IX complex in warfarin-related intracranial hemorrhage. Neurosurgery 1999;45:1113-8.
Burr N, Lummis K, Sood R, Kane JS, Corp A, Subramaniam V. Risk of gastrointestinal bleeding with direct oral anticoagulants: a systematic review and network meta-analysis. Lancet Gasteroenterol Hepatol. 2017;2:85-93.
Caldeira D, Barra M, Ferreira A, Rocha A, Augusto A, Pinto FJ, et al. Systematic review with meta-analysis: the risk of major gastrointestinal bleeding with non-vitamin K antagonist oral anticoagulants. Aliment Pharmacol Ther. 2015;42:1239-49.
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010;12:1360-420.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH et al. Focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33:2719-47
Camm AJ, Pinto FJ, Hankey GJ, Andreotti F, Hobbs FD; Writing Committee of the Action for Stroke Prevention alliance. Non-vitamin K antagonist oral anticoagulants and atrial fibrillation guidelines in practice: barriers to and strategies for optimal implementation. Europace. 2015;17:1007-17.
Cannegieter SC, Rosendaal FR, Wintzen AR, van der Meer FJ, Vandenbroucke JP, Briët E. Optimal oral anticoagulant therapy in patients with mechanical heart valves. N Engl J Med. 1995;333:11-7.
Carothers C, Giancarelli A, Ibrahim J, Hobbs B. Activated prothrombin complex concentrate for warfarin reversal in traumatic intracranial hemorrhage. J Surg Res. 2018;223:183-7.
Chai-Adisaksopha C, Hillis C, Siegal DM, Movilla R, Heddle N, Iorio A, et al. Prothrombin complex concentrates versus fresh frozen plasma for warfarin reversal. A systematic review and meta-analysis. Thromb Haemost. 2016;116(5):879-90.
Chang HY, Zhou M, Tang W, Alexander GC, Singh S. Risk of gastrointestinal bleeding associated with oral anticoagulants: population based retrospective cohort study. BMJ. 2015;350:h1585.
Cheung YW, Barco S, Hutten BA, Meijers JC, Middeldorp S, Coppens M. In vivo increase in thrombin generation by four-factor prothrombin complex concentrate in apixaban-treated healthy volunteers. J Thromb Haemost. 2015;13:1799-805.
Cheung KS, Leung WK. Gastrointestinal bleeding in patients on novel oral anticoagulants: risk, prevention and management. World J Gasteroenterol. 2017;23:1954-63.
Crowther MA, Warkentin TE. Bleeding risk and the management of bleeding complications in patients undergoing anticoagulant therapy: focus on new anticoagulant agents. Blood. 2008;111:4871-9.
CSL Behring. Factors for Life. Available from: http://www.cslbehring.com/docs/578/927/CSL%20Behring%20Factors%20for%20Life_Coagulation%20Disorders.pdf. (Accessed 8 January 2016).
Das A, Liu D. Novel antidotes for target specific oral anticoagulants. Exp Hematol Oncol. 2015;15;4:25.
DeAngelo J, Jarell D, Cosgrove R, Camamo J, Edwards C, Patanwala AE. Comparison of 3-factor versus 4-factor prothrombin complex concentrate with regard to warfarin reversal, blood product use, and costs. Am J Ther. 2017; [epub ahead of print].
Demeyere R, Gillardin S, Arnout J, Strengers PF. Comparison of fresh frozen plasma and prothrombin complex concentrate for the reversal of oral anticoagulants in patients undergoing cardiopulmonary bypass surgery: a randomized study. Vox Sang. 2010;99:251-60.
de Oliveira Manoel AL, Goffi A, Zampieri FG, Turkel-Parrella D, Duggal A, Marotta TR, Macdonald RL, et al. The critical care management of spontaneous intracranial hemorrhage: a contemporary review. Crit Care. 2016;20:272.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest. Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e326S-350S.
Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124:1573-9.
European Medicines Agency. EMA fast-tracks antidote to anticoagulant Pradaxa. September 2015a; Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2015/09/news_detail_002399.jsp&mid=WC0b01ac058004d5c1 (Accessed 5 February 2016).
European Medicines Agency. Summary of Product Characteristics. Praxbind. December 2015b; Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003986/human_med_001938.jsp&mid=WC0b01ac058001d124 (Accessed 5 February 2016).
Evans G, Luddington R, Baglin T. Beriplex P/N reverses severe warfarin-induced over anticoagulation immediately and completely in patients presenting with major bleeding. Br J Haematol. 2001;115:998-1001.
Faraoni D, Levy JH, Albaladejo P, Samama CM; Groupe d’Intérêt en Hémostase Périopératoire. Updates in the perioperative and emergency management of non-vitamin K antagonist oral anticoagulants. Crit Care. 2015;19:203.
FDA, 2015. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/761025Orig1s000Approv.pdf (accessed October 2018).
FDA, 2018. Available from: https://www.fda.gov/downloads/BiologicsBloodVaccines/CellularGeneTherapyProducts/ApprovedProducts/UCM606687.pdf (accessed October 2018).
Frontera JA, Lewin III JJ, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, et al. Guideline for Reversal of Antithrombotics in Intracranial Hemorrhage: A Statement for Healthcare Professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care. 2016;24(1):6-46.
German Medical Association. Cross-sectional guidelines for therapy with blood components and blood derivatives; plasma for therapeutic use. Transfus Med Hemother. 2009;36:345–492.
Ghanny S, Warkentin TE, Crowther MA. Reversing anticoagulant therapy. Curr Drug Discov Technol. 2012;9:143-9.
Ghate SR, Biskupiak J, Ye X, Kwong WJ, Brixner DI. All-cause and bleeding-related health care costs in warfarin-treated patients with atrial fibrillation. J Manag Care Pharm 2011;17:672-84.
Glund S, Stangier J, Schmohl M, Gansser D, Norris S, van Ryn J, et al. Safety, tolerability, and efficacy of idarucizumab for the reversal of the anticoagulant effect of dabigatran in healthy male volunteers: a randomised, placebo-controlled, double-blind phase 1 trial. Lancet. 2015;386:680-90.
Goldstein JN, Refaai MA, Milling TJ Jr, Lewis B, Goldberg-Alberts R, et al. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet. 2015;385(9982):2077-87.
Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131:157-64.
Grandhi R, Newman WC, Zhang X, Harrison G, Moran C, Okonkwo DO, et al. Administration of 4-Factor Prothrombin Complex Concentrate as an Antidote for Intracranial Bleeding in Patients Taking Direct Factor Xa Inhibitors. World Neurosurg. 2015;84:1956-61.
Green L, Tan J, Morris JK, Alikhan R, Curry N, Everington T, et al. A three-year prospective study of the presentation and clinical outcomes of major bleeding episodes associated with oral anticoagulant use in the UK (ORANGE study). Haematologica. 2018;103:738-45.
Grottke O, Van Ryn J, Spronk HM, Rossaint R. Prothrombin complex concentrates and a specific antidote to dabigatran are effective ex-vivo in reversing the effects of dabigatran in an anticoagulation/ liver trauma experimental model. Crit Care. 2014;18:R27.
Grottke O, Aisenberg J, Bernstein R, Goldstein P, Huisman MV, Jamieson DG, et al. Efficacy of prothrombin complex concentrates for the emergency reversal of dabigatran-induced anticoagulation. Crit Care. 2016;20(1):115.
Hanley JP. Warfarin reversal. J Clin Pathol. 2004;57:1132-9.
Harter K, Levine M, Henderson SO. Anticoagulation drug therapy: a review. West J Emerg Med. 2015;16:11-7.
Herzog E, Kaspereit FJ, Krege W, Doerr B, van Ryn J, Dickneite G, et al. Thrombotic safety of prothrombin complex concentrate (Beriplex P/N) for dabigatran reversal in a rabbit model. Thromb Res. 2014;134:729-36.
Herzog E, Kaspereit F, Krege W, Doerr B, Mueller-Cohrs J, Pragst I, et al. Effective reversal of edoxaban-associated bleeding with four-factor prothrombin complex concentrate in a rabbit model of acute hemorrhage. Anesthesiology. 2015a;122:387-98.
Herzog E, Kaspereit F, Krege W, Mueller-Cohrs J, Doerr B, Niebl P, et al. Correlation of coagulation markers and 4F-PCC-mediated reversal of rivaroxaban in a rabbit model of acute bleeding. Thromb Res. 2015b;135:554-60.
Herzog E, Kaspereit F, Krege W, Mueller-Cohrs J, Doerr B, Niebl P, et al. Four-factor prothrombin complex concentrate reverses apixaban-associated bleeding in a rabbit model of acute hemorrhage. J Thromb Haemost. 2015c;13:2220-6.
Hirsh J, Fuster V, Ansell J, Halperin JL; American Heart Association/American College of Cardiology Foundation. American Heart Association/ American College of Cardiology Foundation guide to warfarin therapy. J Am Coll Cardiol. 2003;41:1633-52.
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, et al. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest. Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e152S-84S.
Holt T, Taylor S, Abraham P, McMillan W, Harris S, Curtis J, Elder T et al. Three- versus four-factor prothrombin complex concentrate for the reversal of warfarin-induced bleeding. Int J Crit Illn Inj Sci. 2018;8:36-40.
Honickel M, Braunschweig T, van Ryn J, Ten Cate H, Spronk HM, Rossaint R, et al. Prothrombin complex concentrate is effective in treating the anticoagulant effects of dabigatran in a porcine polytrauma model. Anesthesiology. 2015;123(6):1350-61.
Imberti D, Barillari G, Biasioli C, Bianchi M, Contino L, Duce R, et al. Emergency reversal of anticoagulation with a three-factor prothrombin complex concentrate in patients with intracranial haemorrhage. Blood Transfus. 2011;9:148-55.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1-76.
Johansen M, Wikkelsø A, Lunde J, Wetterslev J, Afshari A. Prothrombin complex concentrate for reversal of vitamin K antagonist treatment in bleeding and non-bleeding patients. Cochrane Database Syst Rev. 2015;7:CD010555.
Kaatz S, Kouides PA, Garcia DA, Spyropolous AC, Crowther M, Douketis JD, et al. Guidance on the emergent reversal of oral thrombin and factor Xa inhibitors. Am J Hematol. 2012;87(Suppl 1):S141-5.
Keeling D, Baglin T, Tait C, Perry D, Baglin C, Kitchen S, et al. Guidelines on oral anticoagulation with warfarin - fourth edition. Br J Haematol. 2011;154:311-24.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37:2893-962.
Kozek-Langenecker SA, Ahmed A, Afshari A, Albaladejo P, Aldecoa P, Barauskas G, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2017;34:332-95.
Landefeld CS, Beyth RJ. Anticoagulant-related bleeding: clinical epidemiology, prediction, and prevention. Am J Med. 1993;95:315-28.
Lankiewicz MW, Hays J, Friedman KD, Tinkoff G, Blatt PM. Urgent reversal of warfarin with prothrombin complex concentrate. J Thromb Haemost. 2006;4:967-70.
Lazo-Langner A, Lang ES, Douketis J. Clinical review: Clinical management of new oral anticoagulants: a structured review with emphasis on the reversal of bleeding complications. Crit Care. 2013;17:230.
Levi M, Moore KT, Castillejos CF, Kubitza D, Berkowitz SD, Goldhaber SZ, et al. Comparison of three-factor and four-factor prothrombin complex concentrates regarding reversal of the anticoagulant effects of rivaroxaban in healthy volunteers. J Thromb Haemost. 2014;12(9):1428-36.
Levine MN, Raskob G, Beyth RJ, Kearon C, Schulman S. Hemorrhagic complications of anticoagulant treatment: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:287S-310S.
Levy JH, Tanaka KA, Dietrich W. Perioperative hemostatic management of patients treated with vitamin K antagonists. Anesthesiology. 2008;109:918-26.
Lip GY, Windecker S, Huber K, Kirchhof P, Marin F, Ten Berg JM, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a join consensus document of the European Society of Cardiology Working Group on Thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacific Heart Rhythm Society (APHRS). Eur Heart J. 2014;35:3155-79.
Majeed A, Meijer K, Larrazabal R, Arnberg F, Luijckx GJ, Roberts RS, et al. Mortality in vitamin K antagonist-related intracerebral bleeding treated with plasma or 4-factor prothrombin complex concentrate. Thromb Haemost. 2014;111:233-9.
Makris M, Watson HG. Annotation: The management of coumarin-induced over-anticoagulation. Br J Haematol. 2001;114:271-80.
Milling TJ Jr, Kaatz S. Preclinical and Clinical Data for Factor Xa and "Universal" Reversal Agents. Am J Med. 2016;129(11S):S80-S8.
Milling TJ Jr, Refaai MA, Goldstein JN, Schneider A, Omert L, Harman A, et al. Thromboembolic Events After Vitamin K Antagonist Reversal With 4-Factor Prothrombin Complex Concentrate: Exploratory Analyses of Two Randomized, Plasma-Controlled Studies. Ann Emerg Med. 2016;67:96-105.e5.
Monroe DM, Hoffman M. What does it take to make the perfect clot? Arterioscler Thromb Vasc Biol. 2006;26:41-8.
Pabinger I, Brenner B, Kalina U, Knaub S, Nagy A, Ostermann H, et al. Prothrombin complex concentrate (Beriplex® P/N) for emergency anticoagulation reversal: a prospective multinational clinical trial. J Thromb Haemost. 2008;6:622-31.
Pabinger I, Tiede A, Kalina U, Knaub S, Germann R, Ostermann H, et al. Impact of infusion speed on the safety and effectiveness of prothrombin complex concentrate: a prospective clinical trial of emergency anticoagulation reversal. Ann Hematol. 2010;89:309-16.
Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D'Angelo A, et al. Bleeding complications of oral anticoagulant treatment:an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. Lancet. 1996;348:423-8.
Pengo V, Crippa L, Falanga A, Finazzi G, Marongiu F, Palareti G, et al. Questions and answers on the use of dabigatran and perspectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Centers (FCSA). Thromb Haemost. 2011;106:868-76.
Pernod G, Godier A, Gozalo C, Tremey B, Sié P; French National Authority for Health. French clinical practice guidelines on the management of patients on vitamin K antagonists in at-risk situations (overdose, risk of bleeding, and active bleeding). Thromb Res. 2010;126:e167-74.
Pernod G, Albaladejo P, Godier A, Samama CM, Susen S, Gruel Y, et al. Management of major bleeding complications and emergency surgery in patients on long-term treatment with direct oral anticoagulants, thrombin or factor-Xa inhibitors: proposals of the working group on perioperative haemostasis (GIHP) - March 2013. Arch Cardiovasc Dis. 2013;106:382-93.
Pollack CV Jr, Reilly PA, Eikelboom J, Glund S, Verhamme P, Bernstein RA, et al. Idarucizumab for dabigatran reversal. N Engl J Med. 2015;373:511-20.
Pollack CV, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA, et al. Idarucizumab for dabigatran reversal – full cohort analysis. New Engl J Med. 2017;377:431-41.
Portola Pharmaceuticals. Press release. Portola Pharmaceuticals Announces New Interim Results from Ongoing ANNEXA-4 Study of Factor Xa Inhibitor Reversal Agent AndexXa® (Andexanet Alfa) in Patients with Life-Threatening Bleeding. Available at: https://globenewswire.com/news-release/2018/03/12/1420761/0/en/Portola-Pharmaceuticals-Announces-New-Interim-Results-from-Ongoing-ANNEXA-4-Study-of-Factor-Xa-Inhibitor-Reversal-Agent-AndexXa-Andexanet-Alfa-in-Patients-with-Life-Threatening-Ble.html (accessed April 2018).
Purrucker JC, Haas K, Rizos T, Khan S, Wolf M, Hennerici MG, et al. Early Clinical and Radiological Course, Management, and Outcome of Intracerebral Hemorrhage Related to New Oral Anticoagulants. JAMA Neurol. 2016;73(2):169-77.
Radaelli F, Dentali F, Repici A, Amato A, Paggi S, Rondonotti E, et al. Management of anticoagulation in patients with acute gastrointestinal bleeding. Dig Liver Dis. 2015;47:621-7.
Refaai MA, Goldstein JN, Lee ML, Durn BL, Milling TJ Jr, Sarode R. Increased risk of volume overload with plasma compared with four-factor prothrombin complex concentrate for urgent vitamin K antagonist reversal. Transfusion. 2015;55:2722-9.
Roussaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, et al. The European guideline on the management of major bleeding and coagulopathy following trauma: fourth edition. Crit Care. 2016;20:100.
Sarode R, Milling TJ Jr, Refaai MA, Mangione A, Schneider A, Durn BL, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation. 2013;128:1234-43.
Schick KS, Fertmann JM, Jauch KW, Hoffmann JN. Prothrombin complex concentrate in surgical patients: retrospective evaluation of vitamin K antagonist reversal and treatment of severe bleeding. Crit Care. 2009;13:R191.
Siegal DM. Managing target-specific oral anticoagulant associated bleeding including an update on pharmacological reversal agents. J Thromb Thrombolysis. 2015;39:395-402.
Siegal DM, Curnutte JT, Connolly SJ, Lu G, Conley PB, Wiens BL, et al. Andexanet Alfa for the Reversal of Factor Xa Inhibitor Activity. N Engl J Med. 2015;373:2413-24.
Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018; [epub ahead of print].
Steinhubl SR, Bhatt DL, Brennan DM, Montalescot G, Hankey GJ, Eikelboom JW, et al. Aspirin to prevent cardiovascular disease: the association of aspirin dose and clopidogrel with thrombosis and bleeding. Ann Intern Med. 2009;150:379-86.
Suzuki Y, Kitahara T, Soma K, Konno S, Sato K, Suzuki S, et al. Impact of platelet transfusion on survival of patients with intracerebral hemorrhage after administration of anti-platelet agents at a tertiary emergency center. PLoS One. 2014;9:e97328.
US Food and Drug Administration, 2018. Available from: https://www.fda.gov/downloads/BiologicsBloodVaccines/CellularGeneTherapyProducts/ApprovedProducts/UCM606687.pdf (accessed October 2018).
US National Library of Medicine. Available from: https://clinicaltrials.gov/ct2/show/NCT01826266 (accessed April 2018).
van der Meer FJ, Rosendaal FR, Vandenbroucke JP, Briët E. Bleeding complications in oral anticoagulant therapy. An analysis of risk factors. Arch Intern Med. 1993;153:1557-62.
van Ryn J, Schurer J, Kink-Eiband M, Clemens A. Reversal of dabigatran-induced bleeding by coagulation factor concentrates in a rat-tail bleeding model and lack of effect on assays of coagulation. Anesthesiology. 2014;120:1429-40.
Xu W, Hu S, Wu T. Risk analysis of new oral anticoagulants for gastrointestinal bleeding and intracranial hemorrhage in atrial fibrillation patients: a systematic review and network meta-analysis. J Zhejiang Univ-Sci B (Biomed & Biotechnol). 2017;18:567-76.
Zahir H, Brown KS, Vandell AG, Desai M, Maa JF, Dishy V, et al. Edoxaban effects on bleeding following punch biopsy and reversal by a 4-factor prothrombin complex concentrate. Circulation. 2015;131:82-90.
of interest
are looking at
saved
next event
Job number: KCT16-01-0010
Developed by EPG Health for Medthority in collaboration with CSL Behring, with content provided by CSL Behring.
Not intended for Healthcare Professionals outside Europe.

