CDK4/6 inhibitor trials in breast cancer
Cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitors now represent standard of care for advanced breast cancer. Could they also be beneficial in early breast cancer?
- Find out the results of clinical trials for CDK4/6 inhibitors in early and advanced breast cancer
- Learn the latest CDK4/6 inhibitor survival data from our breast cancer experts
- Optimally manage CDK4/6 inhibitor safety in your patients
CDK4/6 inhibitor clinical trials in early breast cancer
The CDK4/6 inhibitors palbociclib, abemaciclib and ribociclib are approved in the US and Europe for treatment of HR+/HER2− advanced breast cancer (ABC) in combination with endocrine therapy (ET)1. Indeed, combined therapy is now considered standard of care for patients with ABC at high risk of recurrence1.
Investigation to determine whether CDK4/6 inhibition would be beneficial in early disease led to FDA and EMA approval of abemaciclib for high-risk HR+/HER2− early breast cancer based on the outcome for the monarchE trial2–5
CDK4/6 inhibitor treatment in early breast cancer
In October 2021, the US Food and Drug Administration (FDA) extended the indication for abemaciclib to include adjuvant treatment of adult patients with HR+/HER2−, node-positive, early breast cancer (EBC) at high risk of recurrence and a Ki-67 score of ≥20%2. The FDA also approved the Ki-67 IHC MIB-1 pharmDx (Dako Omnis) assay as a companion diagnostic test for selecting patients for this indication2. In April 2022, the European Medicines Agency (EMA) also approved the use of abemaciclib as adjuvant treatment of adults with HR+/HER2−, node-positive, early breast cancer (EBC) at high risk of recurrence; however, the EMA indication for abemaciclib does not require a Ki-67 score of ≥20%3.
Soon after the FDA approved the extended indication for abemaciclib, the American Society for Clinical Oncology (ASCO) updated their guidelines to include abemaciclib for 2 years plus ET for ≥5 years as a treatment option for patients with high-risk HR+/HER2− EBC6. The updated guidelines also define high risk of recurrence according to the monarchE criteria of ≥4 positive axial lymph nodes (ALN) or 1–3 positive ALN and one or more of6:
- histological grade 3 disease
- tumour size ≥5cm
- Ki-67 score ≥20%.
In March 2023, following publication of updated results from the monarchE trial, the FDA removed the requirement of Ki-67 testing to receive abemaciclib for EBC2,7.
To learn more about the FDA and EMA indications as well as the guidelines from ESMO, ASCO and NICE regarding use of abemaciclib for EBC, view the infographic below.
Evidence for CDK4/6 inhibitors in early breast cancer
Following the success of CDK4/6 inhibition in the treatment of ABC, four phase 3 clinical trials were initiated to evaluate efficacy of CDK4/6 inhibitors in combination with ET for treatment of high-risk HR+/HER2− EBC. These trials include the monarchE4,5 trial for abemaciclib, the NATALEE8 trial for ribociclib, and the PALLAS9 and PENELOPE-B10 trials for palbociclib. The trials differed in their definition of high-risk EBC, but nodal involvement was an inclusion criterion in all trials except the PALLAS trial, which recruited a small number of node-negative patients. None of the trials used biomarkers to define high-risk, although the monarchE and NATALEE trials included patients with Ki-67 scores of ≥20. The primary endpoint for each trial was invasive disease-free survival (Table 1).
Table 1. Clinical trials for CDK4/6 inhibitors in HR+/HER2− early breast cancer4,5,8–10. ALN, axial lymph node; bid, twice daily; CPS-EG, clinical-pathological state oestrogen receptor grade; ET, endocrine therapy; HR, hormone receptor; HER2, human epidermal growth factor 2; IDFS, invasive disease-free survival; NACT, neoadjuvant chemotherapy; od, once daily; RT, radiotherapy.
| monarchE | NATALEE | PALLAS | PENELOPE-B | |
| Trial design (n) |
Open label Randomised (n = 5637) |
Open label Randomised (n = 5000) |
Open label Randomised (n = 5760) |
Double-blind Placebo-controlled Randomised (n = 1250) |
| Inclusion criteria | HR+/HER2− Stage II–III 2 cohorts: Cohort 1: ≥4 positive ALN or 1–3 positive ALN with grade 3 or tumour size ≥5 cm Cohort 2: 1–3 positive ALN and Ki-67 ≥20% |
HR+/HER2− Anatomic stage II: node-negative with grade 2–3 and/or Ki-67 ≥20% or 1–3 positive ALN Anatomic stage III |
HR+/HER2− Anatomic stage II–III Node-positive and node-negative |
HR+/HER2− Residual disease after ≥16 weeks of NACT CPS-EG score ≥3 or 2 with nodal involvement after NACT |
| ET treatment, surgery or RT at entry | ≤12 months of starting ET | ≤12 months of starting ET | ≤6 months of starting ET | <16 weeks of surgery or <10 weeks after completing RT |
| Treatment (duration) |
Abemaciclib bid, continuous + ET or ET alone (3 years) |
Ribociclib od, 21 days on/7 days off + ET or ET alone (3 years) |
Palbociclib od, 21 days on/7 days off + ET or ET alone (2 years) |
Palbociclib od, 21 days on/7 days off + ET or Placebo + ET (1 year) |
| Primary endpoint (IDFS) | 85·8% (Abemaciclib + ET) 79·4% (ET alone) HR = 0·664 95% CI 0·57–0·76 (P<0.0001) at 4 years |
Not available | 84.2% (Palbociclib + ET) 84.5% (ET alone) HR = 0.96 95% CI, 0.81–1.14 (P=0.65) at 4 years |
81.2% (Palbociclib + ET) 77.7% (placebo + ET) HR = 0.93 95% CI, 0.74–1.17 (P=0.525) at 3 years |
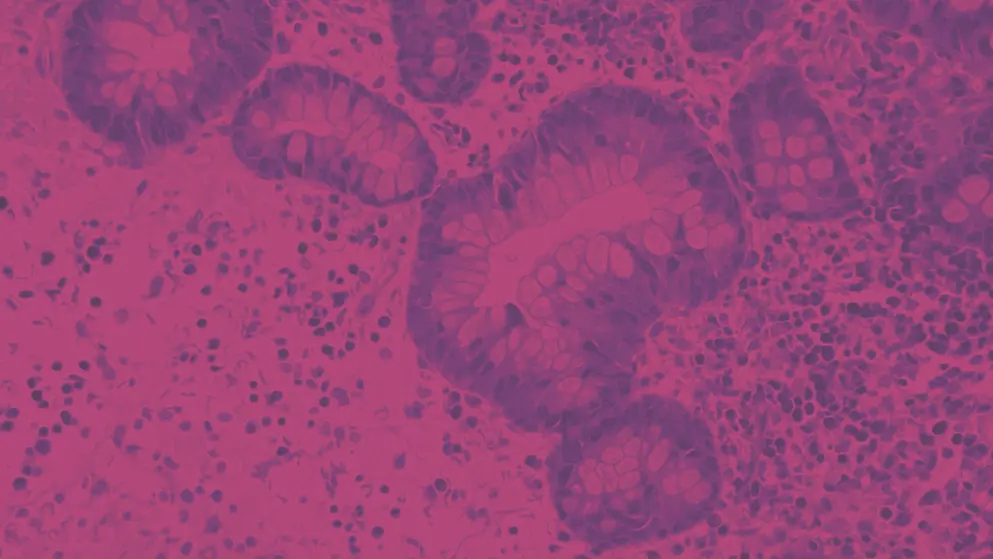
In the monarchE trial, addition of abemaciclib to ET significantly improved invasive disease-free survival (Table 1), regardless of Ki-67 status (Figure 1)4,5. Addition of palbociclib, however, did not confer benefit in either the PALLAS or PENELOPE-B trials (Table 1; Figures 2)9,10. Preliminary results of the NATALEE trial show that ribociclib in combination with ET significantly reduces the risk of disease recurrence11.
Figure 1. Invasive disease-free survival in the monarchE trial for abemaciclib. Shown are the results for abemaciclib + ET, compared with ET alone in cohort 1 Ki-67-high and Ki-67-low populations at 3 years’ follow up (Adapted4). CI, confidence intervals; ET, endocrine therapy; HR, hazard ratio.
Figure 2. Invasive disease-free survival in the A) PALLAS and B) PENELOPE-B trials for palbociclib (Adapted9,10). CI, confidence intervals; ET, endocrine therapy; HR, hazard ratio.
Explanations proposed for the discordant results between the monarchE trial and the PALLAS and PENELOPE-B trials include differences in eligibility criteria, definition of high-risk disease and discontinuation rates. These differences, however, have been ruled out as contributing factors12. Alternatively, studies have shown that in EBC, one week of rest from CDK4/6 inhibition is sufficient to increase cell proliferation1. Although speculative, the different dosing schedules may explain the divergent outcomes in the monarchE trial, where abemaciclib was administered continuously, and the PALLAS and PENELOPE-B trials, where an on/off schedule was used for palbociclib.
Safety profile of abemaciclib in the monarchE trial
A detailed safety analysis of abemaciclib was conducted at a median follow-up of 27 months, to assess the incidence, management and outcomes of common and clinically relevant adverse events. In addition, patient-reported health-related quality-of-life, including fatigue and side-effect burden were assessed13.
Abemaciclib was associated with a significantly higher incidence of toxicities, compared with ET alone4. Diarrhoea was the most common adverse event reported by patients who received abemaciclib, but this was typically low grade and manageable with anti-diarrhoeal agents and/or dose reductions. Diarrhoea was usually reported within the first 3 months of treatment and the incidence decreased over time13.
Clinical symptoms, including neutropenia, were also more frequent in patients treated with abemaciclib, but rarely caused serious complications and were also manageable with dose reductions. Adverse events typically associated with ET alone, including arthralgias and hot flushes, were less frequent in patients treated with abemaciclib. Additionally, patient-reported outcomes showed no difference in the burden of side effects between the two treatment groups13.
Given that the most common adverse events were mild-to-moderate and manageable with the appropriate treatment and/or dose adjustments, the safety profile of abemaciclib was considered acceptable and supports a positive benefit-risk balance for patients with high-risk, node-positive early HR+/HER− early breast cancer
Review current recommendations for chemotherapy and endocrine therapy in early breast cancer
Learn more about the CDK4/6 pathway and its role in breast cancer
CDK4/6 inhibitor clinical trials in advanced breast cancer
The cyclin-dependent kinase 4 and 6 inhibitors (CDK4/6 inhibitors) abemaciclib, palbociclib and ribociclib have been approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the treatment of hormone receptor-positive (HR+) and human epidermal growth factor receptor 2 negative (HER2−) advanced breast cancer (ABC)2,3,14–16.
In this video, Dr Gregory Vidal from the West Cancer Centre and Research Institute (University of Tennessee, USA) shares his view on the landmark clinical trials for CDK4/6 inhibitors in patients with HR+/HER2− metastatic breast cancer (mBC).
The patient populations assessed, treatment arms and the key outcomes for the landmark clinical trials for abemaciclib (MONARCH series17–22), palbociclib (PALOMA series23,24) and ribociclib (MONALEESA series25–30) are summarised in Table 2. Note that cross-study comparisons should be avoided because of differences in patient populations assessed, treatment partners used, and study design.
Table 2. Summary of CDK4/6 inhibitor clinical trials in advanced breast cancer.
The efficacy and safety of the CDK4/6 inhibitors in the landmark trials are discussed in detail below.
It is important to note that there are several ongoing clinical trials for CDK4/6 inhibitors that aim to understand their utility in different clinical settings and patient subgroups, such as those with central nervous system involvement or heavily pre-treated disease.
Visit our section on CDK4/6 inhibitor selection
Dr Laura Spring from the Massachusetts General Hospital Cancer Centre (Harvard Medical School, USA) points out that due to the success of the landmark trials, CDK4/6 inhibitors are also being investigated in the adjuvant setting for early breast cancer.
The clinical impact of COVID-19 on CDK4/6 inhibitor treatment
Given the global COVID-19 pandemic and associated changes to the management of patients with metastatic breast cancer, a study was conducted in the UK to evaluate the implementation of new guidelines. In this study of 87 patients with ER+/HER2- metastatic breast cancer who began treatment with a CDK4/6 inhibitor during the pandemic, NICE and international ESMO COVID-19 guidelines were followed, and changes to treatment were documented with respect to delay, omission or reduction31.
Results indicated that CDK4/6 inhibitor treatment was delivered safely, and dose reductions improved tolerability without affecting efficacy. Furthermore, CDK4/6 inhibitor-associated neutropenia was unlikely to contribute to risk of infection with COVID-1931.
Abemaciclib in advanced breast cancer
In the clinical trial MONARCH 1, abemaciclib showed benefit as monotherapy in heavily pre-treated patients with hormone receptor positive/human epidermal growth factor receptor 2 negative (HR+/HER2-) metastatic breast cancer (mBC)17,18. In the MONARCH 2 and 3 trials, adding abemaciclib to endocrine therapy (ET) demonstrated significant and clinically meaningful improvement in median progression-free survival in first- and second-line therapy for HR+/HER2-19–22. Diarrhoea emerged as the predominant abemaciclib-related adverse event, and was managed with conventional anti-diarrhoeal agents or dose reduction19–22.
Exploratory analysis of MONARCH 2 and 3 indicated that adding abemaciclib to ET shows greatest benefit to patient subgroups with high proliferative disease, progesterone receptor-negative status, or liver metastases19,32.
Efficacy
MONARCH 1
The phase 2 MONARCH 1 trial evaluated the efficacy of abemaciclib monotherapy in 132 women with refractory HR+/ HER2− mBC17. Patients had received a median of 3 (range 1–8) lines of prior systemic therapy in the metastatic setting, including a median of 1 (range 1–3) line of chemotherapy (ChT) and 2 (range of 1–6) lines of ET. This heavily pre-treated patient group all had measurable disease at study entry and 90.2% had visceral disease, while 50.8% had 3 or more metastatic sites17.
Treatment with abemaciclib monotherapy benefited some patients with a poor prognosis, showing a confirmed objective response rate (ORR) of 19.7% (95% CI, 13.3–27.5)17. Of these responders, 46.2% received at least 2 prior chemotherapies in the advanced setting. 92.3% had visceral disease, and 46.2% had three or more metastatic sites17.
MONARCH 2
MONARCH 2 was a phase 3 study involving 669 women with HR+/HER2− advanced breast cancer (ABC) who had progressed while receiving neoadjuvant or adjuvant ET ≤12 months from the end of adjuvant ET, or while receiving first-line ET for mBC20.
Study participants were initially given a 200 mg twice-daily dose of abemaciclib; however, a review of safety data and dose reduction rates led to the protocol being amended and the dose reduced to 150 mg for all new and enrolled patients.
Administration of abemaciclib (150 mg, twice daily) on a continuous schedule plus fulvestrant (500 mg) significantly extended progression-free survival versus placebo plus fulvestrant with 16.4 months in the abemaciclib arm and 9.3 months in the placebo arm (P<0.001) (Figure 3)20.
Figure 3. Investigator-assessed progression-free survival following treatment with abemaciclib plus fulvestrant or placebo plus fulvestrant (Adapted from Sledge et al.20). CI, confidence interval; HR, hazard ratio.
Among patients with measurable disease, the overall response rate was 48.1% in patients receiving abemaciclib and 21.3% in the placebo group (P<0.001). Meanwhile, the clinical benefit rates were 72.2% and 56.1%, respectively (P<0.001)20.
Investigators in the MONARCH 2 study also included an exploratory analysis of change in tumour size over time. After 12, 28-day treatment cycles, the mean change in tumour size was −62.5% in the abemaciclib group and −32.8% in the placebo group20.
In a recent updated analysis of the MONARCH 2 cohorts, overall survival (OS) was found to be significantly improved in the abemaciclib plus fulvestrant group, with OS of 46.7 months compared with 37.3 months in the placebo plus fulvestrant group (P=0.01) (Figure 4)19.
Figure 4. Overall survival for all patients in the MONARCH 2 clinical trial (Adapted from Sledge et al.19). CI, confidence interval; HR, hazard ratio.
A 2020 MONARCH 2 efficacy update including East Asian patients with HR+/HER2− ABC, who progressed on ET, showed that OS rates at 42 months were 64% (95% CI, 55.5–71.8) for abemaciclib plus fulvestrant, and 53% (95% CI, 39.9–64.6) for placebo plus fulvestrant. Time to second objective disease progression (PFS2) (HR 0.588 [95% CI, 0.420–0.823; P=0.001]), time to ChT (HR 0.601 [95% CI 0.411–0.877; P=0.008]) and ChT-free survival (HR 0.573 [95% CI 0.402–0.815; P=0.002]) were all significantly improved with abemaciclib plus fulvestrant32.
The objective response rate (ORR) from endocrine-naive participants in MONARCH 2 was recently presented at the European Society for Medical Oncology (ESMO) Congress 2021. In this pooled cohort (N = 110), the primary endpoint of investigator-assessed confirmed ORR was 59.1% (95% CI, 49.9–68.3). The median follow-up was 9.8 months, with no new safety signals reported. The confirmed ORR compares similarly to that reported for fulvestrant monotherapy in patients with similar disease state and demonstrates a similar safety profile to that reported in the main MONARCH 2 primary study. Note that duration of response and progression-free survival data are not yet mature33.
MONARCH 3
The phase 3 MONARCH 3 study assessed abemaciclib (150 mg, twice daily, continuous schedule) plus a non-steroidal aromatase inhibitor (NSAI; 1 mg anastrozole or 2.5 mg letrozole, daily) in postmenopausal patients with HR+/HER2− ABC who had not received prior systemic therapy for their advanced disease21. In the interim analysis, the primary endpoint of investigator-assessed PFS was met with a median PFS of 14.7 months in the placebo arm versus not reached in the abemaciclib arm (HR 0.54; 95% CI, 0.41–0.72; P=0.000021)21. In the final PFS analysis, a median PFS of 14.76 months was observed in the placebo arm versus 28.18 months in the abemaciclib arm (P=0.000002) (Figure 5)22.
Figure 5. Final progression-free survival for patients assessed in the MONARCH 3 clinical trial (Adapted from Johnston et al.22). AI, aromatase inhibitor; CI, confidence interval; HR, hazard ratio.
In patients with measurable disease, the objective response rate was 61.0% in the abemaciclib arm and 45.5% in the placebo arm (P=0.003)22.
Exploratory subgroup analyses for abemaciclib in MONARCH 2 and 3
An exploratory analysis of MONARCH 2 and 3 evaluated prognostic subgroups to identify groups that might receive the largest benefit from abemaciclib, including subgroups for whom endocrine monotherapy could be a suitable initial treatment34.
Prognostic characteristics identified in the retrospective analysis of MONARCH 2 and 3 included in the exploratory analysis were: treatment-free interval; liver metastases; bone-only disease; progesterone receptor status; tumour grade; or ECOG (Eastern Cooperative Oncology Group).
The exploratory analysis found that all subgroups in MONARCH 2 and 3 benefited from the addition of abemaciclib to ET, consistent with the overall study populations in both trials. The greatest improvements from abemaciclib occurred in patient subgroups with more aggressive cancer, such as those with liver metastases, progesterone receptor-negative status, or high-grade tumours35.
Safety
MONARCH 1
The adverse event profile for abemaciclib differed from that of either ribociclib or palbociclib, with diarrhoea emerging as the predominant issue as opposed to neutropenia. The most common treatment-associated adverse events of any grade that were reported in the MONARCH 1 study were17:
- diarrhoea (90.2%)
- fatigue (65.2%)
- nausea (64.4%)
- decreased appetite (45.5%)
- abdominal pain (38.6%)
MONARCH 2
An abemaciclib dose of 150 mg twice daily was used in MONARCH 2 study, as opposed to the 200 mg twice-daily dose used in MONARCH 117,19. As in MONARCH 1, diarrhoea was the most commonly reported adverse event. Incidence of neutropenia, nausea, fatigue and abdominal pain were also high, while febrile neutropenia remained rare (Table 3).
The most frequently occurring serious adverse event was venous thromboembolism (VTE), which occurred in 21 patients (4.8%) receiving abemaciclib, compared with two patients receiving placebo treatment 17,19.
Table 3. Adverse events (≥25%) reported in MONARCH 2 (Adapted from Sledge et al.20).
MONARCH 3
As in the MONARCH 1 and 2 trials, diarrhoea was the most common adverse event in MONARCH 3. However, patients were treated with anti-diarrhoeal agents at first onset and, among those experiencing recurrent or high-grade episodes, abemaciclib dose was reduced21,22.
Dose modification in 43% of patients receiving abemaciclib limited treatment discontinuation due to adverse side effects to 13% in this study21,22.
Monarch 3 reported a higher (6%) incidence of VTE than was seen in Monarch 2, which was a 10-fold increase when compared with placebo 21,22.
Close patient monitoring is suggested because of a significantly higher incidence of venous thromboembolism in patients receiving abemaciclib as shown in the MONARCH 2 and MONARCH 3 trials19–22
Palbociclib in advanced breast cancer
In 2015, the PALOMA-1 trial defined for the first time the efficacy and activity of palbociclib in metastatic breast cancer (mBC)35. PALOMA-1, 2 and 3 achieved their primary endpoint of improvement in progression-free survival (PFS)23,24,35. Most common grade 3–4 adverse events in the combination arms were neutropenia, leucopenia, fatigue (PALOMA-1)38, including anaemia and febrile neutropenia (PALOMA-2)23, and thrombocytopenia (PALOMA-3)24. No cases of febrile neutropenia or neutropenia-related infections were reported in PALOMA-135. Febrile neutropenia was reported in 0.6% of patients in the experimental arm in PALOMA-324. In PALOMA-2, there was a significantly greater improvement in pain in palbociclib plus letrozole23. Patients in PALOMA-3 who received palbociclib showed significant improvement in pain and in time-to-deterioration questionnaire scores24.
Post-hoc analyses were conducted on the PALOMA-2 and PALOMA-3 trials to evaluate time to chemotherapy for the patients enrolled in both trials. Results indicate that palbociclib plus letrozole prolonged time to chemotherapy, compared with placebo plus letrozole, across all subgroups. In addition, there was a longer time to subsequent chemotherapy for patients in PALOMA-2 (palbociclib plus letrozole in the first-line), compared with those in PALOMA-3 (palbociclib plus endocrine after progressing on prior endocrine therapy)36.
Efficacy
PALOMA-2
The PALOMA-2 trial randomised 666 postmenopausal women with hormone receptor positive (HR+)/human epidermal growth factor receptor 2 negative (HER2−) metastatic breast cancer (mBC), who had received no prior treatment for their disease23,24.
The primary endpoint was median mPFS16,24. The combination of palbociclib and letrozole produced an mPFS of 24.8 months (95% CI, 22.1 months, non-estimable) versus 14.5 months (95% CI, 12.9–17.1 months) with placebo plus letrozole (Figure 6)19,20.
Figure 6. Primary endpoint (mPFS) results in the PALOMA-2 trial (Adapted from Finn et al.24). CI, confidence interval; HR, hazard ratio; LET, letrozole; NE, non-estimable; PFS, progression-free survival; PLA, placebo.
Analysis of the secondary outcomes revealed that the number of patients with a confirmed objective response in patients with measurable disease was 55.3% (95% CI, 49.9–60.7) in patients receiving palbociclib and letrozole, compared with 44.4% (95% CI, 36.9–52.2) of the placebo and letrozole group (P=0.03)24.
The results of the clinical benefit response in these patients were also significantly better for the group receiving palbociclib in combination with letrozole versus placebo with letrozole (84.3% vs. 70.8%, P<0.001)24.
Subsequent follow-up data (37.6 months in the palbociclib plus letrozole arm versus 37.3 months in the placebo plus letrozole arm) showed an mPFS of 27.6 months (95% CI, 22.4–30.3) for palbociclib plus letrozole versus 14.5 months (95% CI, 12.3–17.1) for the placebo plus letrozole arm (HR 0.563, P<0.0001)37. The mPFS was also consistently longer across all patient subgroups, including patients with bone-only disease and patients with a longer disease-free interval37.
PALOMA-2 also evaluated patient-reported outcomes (PROs) using the Functional Assessment of Cancer Therapy (FACT)-Breast and EuroQOL 5 dimensions (EQ-5D) questionnaires38. These results showed significantly greater improvement in pain scores in the palbociclib plus letrozole arm (−0.256 versus −0.098; P=0.0183)38.
In a recent analysis of 61 patients with mBC who were HR+/HER2− and starting treatment with palbociclib with letrozole, PFS was calculated from the date of their mBC diagnosis to March 2021. Median PFS was 27.9 months (95% CI, 21.3–34.5), analogous with that in the PALOMA-2 study. The results also revealed that a longer PFS was achieved by patients with performance status of 0, no liver metastases, or bone only (non-visceral) metastases, compared with patients in which these features were present. This analysis suggests that metastatic pattern and performance status can be useful predictors of PFS, and may have a bearing on how regularly one should monitor patients with mBC who are being treated with palbociclib39.
PALOMA-3
The PALOMA-3 study evaluated 521 patients with endocrine-resistant mBC, who had either progressed on/within 12 months of completion of adjuvant endocrine therapy (ET) or on/within 1 month after ET for mBC23. Pre-/perimenopausal and postmenopausal women were included23.
The primary endpoint of PALOMA-3 was mPFS, which doubled for patients receiving palbociclib with fulvestrant, compared with those receiving placebo with fulvestrant (9.5 months vs. 4.6 months; HR 0.46; 95% CI, 0.36–0.59; P<0.0001)23. Importantly, the improvements in mPFS were observed consistently across pre-defined patient sub-groups23.
In patients with measurable disease, an objective response rate of 25% (95% CI, 19.6–30.2) was seen in patients receiving palbociclib with fulvestrant, compared with 11% (95% CI, 6.2–17.3) in patients who received placebo with fulvestrant (OR 2.69; P=0.0012)23.
Similar results were observed for the clinical benefit response with 64% (95% CI, 57.7–69.6) of palbociclib plus fulvestrant patients achieving this versus 36% (95% CI, 28.2–44.8) of placebo plus fulvestrant patients (OR 3.10; P<0.0001)23.
A follow-up study revealed that the mPFS for palbociclib with fulvestrant, compared with placebo plus fulvestrant was 11.2 months vs. 4.6 months, respectively (HR 0.497, 95%CI, 0.398–0.620; P<0.0001)40.
In addition to the primary endpoint of mPFS, a key secondary endpoint of PALOMA-3 was overall survival (OS).
A six-year follow-up of the phase 3 PALOMA-3 trial showed that palbociclib plus fulvestrant produced a clinically meaningful long-term improvement in OS (P=0.0221) in patients with HR+/HER2− advanced breast cancer (ABC) (Table 4)41.
Table 4. Updated overall survival for the PALOMA-3 trial in the intent-to-treat population and by sub-group (Adapted from Cristofanilli et al.41). ABC, advance breast cancer; CI, 95% confidence interval; ET, endocrine therapy; FUL, fulvestrant; ITT, intent-to-treat; OS, overall survival; PAL, palbociclib; PBO, placebo.
| Subgroup | N (%) | Hazard Ratio (CI) | PAL+FUL median OS (CI) |
PBO+FUL median OS (CI) |
1-sided P value |
| ITT population | 521 (100) | 0.81 (0.65–0.99) |
34.8 (28.8–39.9) |
28.0 (23.5–33.8) |
0.0221 |
| Sensitivity to prior ET | 410 (78.7) | 0.76 (0.60–0.96) |
39.7 (34.4–45.7) |
29.5 (23.5–36.3) |
0.011 |
| No sensitivity to prior ET | 111 (21.3) | 0.97 (0.62–1.5) |
19.9 (17.4–26.4) |
26.2 (17.5–31.8) |
0.440 |
| Prior chemotherapy in ABC | 177 (34.0) | 0.97 (0.69–1.4) |
24.6 (21.3–30.0) |
24.3 (18.9–36.3) |
0.432 |
| No prior chemotherapy in ABC | 344 (66.0) | 0.72 (0.55–0.94) |
39.3 (34.5–44.4) |
29.7 (23.8–35.5) |
0.008 |
The 5-year OS rate for the palbociclib plus fulvestrant and fulvestrant plus placebo groups were 23.3% (95% CI, 18.7–28.2) and 16.8% (95% CI, 11.2–23.3), respectively41.
OS with palbociclib plus fulvestrant compared with fulvestrant plus placebo was also maintained, regardless of the status of ESR1, PIK3CA, and TP53 gene mutations, as determined by treatment circulating tumour (ctDNA) polymerase chain reaction (PCR) sequencing analysis41.
PALOMA-4
In the PALOMA-2 trial, a subgroup analysis revealed that palbociclib plus letrozole may be an effective first-line treatment in postmenopausal Asian women with oestrogen receptor-positive (ER+)/HER2– ABC. This is especially promising given the increased incidence of breast cancer in Asian women over the past 40 years. The PALOMA-4 trial was conducted to assess efficacy and safety of palbociclib plus letrozole in Asian patients.
This phase 3 international, double-blind, randomised trial investigated postmenopausal Asian women who had not received prior systemic therapy for ER+/HER2– ABC. Kaplan-Meier analysis of investigator-assessed PFS was the primary endpoint, comparing between-arms using a stratified log-rank test. Objective response rate and safety (descriptively summarised) were amongst the secondary endpoints.
The primary results from PALOMA-4 confirmed that treating postmenopausal Asian women with ER+/HER2– ABC in the first line with palbociclib plus letrozole, was efficacious and safe. Median PFS based on investigator assessment at the data cutoff date was 21.5 months for the experimental arm (palbociclib + letrozole) versus 13.9 months for the placebo arm (placebo + letrozole) (HR 0.68; 95% CI, 0.53–0.87; P=0.0012). The objective response rate based on investigator assessment was 37.3% versus 31.6% among all patients (P=0.154), and 43.4% versus 38.0% in patients with measurable disease (P=0.206)42.
Safety
The most common all-grade adverse events based on a pooled dataset from across the PALOMA programme were14:
- neutropenia (82.1%)
- infections (59.2%)
- leucopenia (48.6%)
- fatigue (41.5%)
- nausea (36.0%)
- stomatitis (30.3%)
- anaemia (29.6%)
- alopecia (26.8%)
- diarrhoea (27.3%)
It is worth noting, however, that these adverse events were generally manageable.
Despite the high levels of neutropenia, febrile neutropenia was reported in 1.4% of cases, resulting in palbociclib discontinuation in ≤1.6% of patients across both studies14,23,24.
Beyond results from these pivotal clinical trials, clinicians in daily practice encounter a wide variety of clinical presentations. The growing body of real-world studies provide important information on the ‘real-world’ performance of palbociclib. These studies confirm the results of the PALOMA trials, as palbociclib plus ET appear to be effective and safe also in unselected patients43. Efficacy was related to the line of treatment in which palbociclib was used; trials enrolling heavily pre-treated patients reported low efficacy of the combination43.
Real-world effectiveness of palbociclib
In a retrospective analysis of 785 older patients (median age 74.0 years) with advanced breast cancer, real-world progression-free survival and overall survival were compared between patients treated with palbociclib plus letrozole versus letrozole alone. In the palbociclib plus letrozole cohort, median real-world progression-free survival was 22.2 months (95%CI, 20.0–30.4), compared to 15.8 months (95% CI, 12.9–18.9) in the letrozole cohort (HR 0.59; 95% CI, 0.47–0.74; P<0.0001)44.
In the palbociclib plus letrozole cohort, median overall survival was not reached, versus 43.4 months (95% CI, 30.0–NR) in the letrozole cohort (HR 0.55; 95% CI, 0.42–0.72, P<0.0001)44.
These results support the effectiveness of palbociclib plus letrozole as a standard first-line treatment for older HR+/HER2- advanced breast cancer patients48.
In another study the use, efficacy and toxicity of palbociclib was examined in the first National Health Service patients in the UK, who were treated with CDK4/6 inhibitors outside of a clinical trial. These patients had been treated in the first-line setting between April and December 2017. At the end of the 24-month observation period, median progression-free survival was 22.5 months, median overall survival was not reached, median progression-free survival and median overall survival was not reached for de novo patients nor for patients who relapsed >12 months from the end of adjuvant treatment (n=41)45.
These real-world results add evidence to the effectiveness and tolerability of palbociclib45.
In another real-world study of older patients with advanced HR+/HER2− breast cancer, the tolerability and efficacy of palbociclib combined with an aromatase inhibitor as first-line treatment was investigated. 276 patients were eligible to participate in this retrospective national study in the UK, which was the largest known dataset of tolerability and efficacy of palbociclib in women aged ≥75 years. Results indicated that this therapy is effective and well-tolerated, with very low levels of adverse events leading to hospitalisations due to appropriate management (dose delays/reductions)46.
Real-world use of palbociclib was also examined in a prospective, real-world, noninterventional study of patients with HR+/HER2‒ advanced breast cancer. In this study, treatment patterns were examined in Black and Indigenous peoples and people of colour: groups commonly underrepresented in clinical trials. The interim analysis reveals that in clinical practice, palbociclib was normally prescribed in this patient group, and that this treatment was well tolerated. Results also indicated that there were similar rates of dose modifications and adverse events, regardless of the treatment partner47.
Ribociclib in advanced breast cancer
The MONALEESA clinical trials demonstrate the treatment benefit and manageable safety profile of ribociclib in combination with aromatase inhibitors or fulvestrant, compared with placebo, in hormone receptor positive and human epidermal growth factor receptor 2 negative (HR+/HER2−) advanced breast cancer (ABC)25–30. Many adverse events reported were consistent across all trials25–30. The most common adverse events of any grade that occurred in ≥25% of patients were neutropenia, leukopenia and nausea.
The MONALEESA clinical programme for ribociclib includes diverse patient populations in different treatment settings25–30. In addition to the data provided by this programme, ongoing clinical investigations are evaluating other applications and characteristics of ribociclib with different combination drugs, in different patient populations and in other treatment settings. Overall survival data with ribociclib for the treatment of HR+/HER2− ABC in a phase 3 setting have not been published. Combining ribociclib with other therapeutic agents has become an option to improve PFS and overcome endocrine therapy (ET) resistance48.
At the European Society for Medical Oncology (ESMO) Congress in 2021, the results of a phase 3b, multicentre, open-label study of ribociclib plus letrozole were revealed. In this study, the patient settings were broader than those explored in the MONALEESA studies. This study recruited patients of any menopausal status with HR+/HER2– ABC who were not responsive to curative treatment. The secondary endpoints that were reported confirmed the previous findings of MONALEESA in a wider population49.
Efficacy
MONALEESA-2
The MONALEESA-2 trial included 668 postmenopausal women with HR+/HER2- metastatic or recurrent BC who had received no prior treatment for their advanced disease25,26.
The trial met its primary endpoint (median progression free-survival [mPFS]) and demonstrated superiority of ribociclib plus letrozole versus placebo plus letrozole. At the point of analysis, the ribociclib group had not reached the median duration of PFS (95% CI, 19.3–not reached) compared with 14.7 months (95% CI, 13.0–16.5) in the placebo group (Figure 7)25,26.
Figure 7. Median progression-free survival following treatment with ribociclib plus letrozole or placebo plus letrozole (Adapted from Hortobagyi et al.25). CI, confidence interval; HR, hazard ratio; PFS, progression free survival.
At the time of the second interim analysis (median 26.4 months of follow-up), mPFS rates for ribociclib plus letrozole were 25.3 months vs. 16.0 months for the placebo plus letrozole group (HR 0.568; 95% CI, 0.457–0.704; log-rank P=9.63 x 10-8)26.
The ORR for all patients was 42.5% in the ribociclib plus letrozole arm versus 28.7% in the placebo plus letrozole arm (P=9.18 x 10-5)26.
In patients with measurable disease at baseline, the overall response rate was 54.5% in patients receiving ribociclib and 38.8% in the placebo group (P=2.54 x 10-4)26.
MONALEESA-3
Results from the MONALEESA-3 trial were published in 201829. The primary endpoint was met with a mPFS of 20.5 months for patients receiving ribociclib (n = 484) and 12.8 months for patients receiving placebo (n = 242) (HR 0.59; 95% CI, 0.48–0.73; P<0.001).
Similar benefits were observed in patients who had received prior ET, compared with those who had not. The risk of disease progression was reduced by 42% in treatment-naive patients receiving ribociclib, who had not received prior ET for advanced disease and 43% in patients who received ribociclib and had one previous ET treatment28.
The objective response rate (ORR) was 32.4% for all patients in the ribociclib plus fulvestrant group versus 21.5% for the placebo plus fulvestrant group (P<0.001). In patients with measurable disease at baseline, the ORR was also significantly improved in patients receiving ribociclib, compared with patients in the placebo group (40.9% vs. 28.7%, respectively; P=0.003)28.
In a follow up to this study, the overall survival at 42 months was found to be 57.8% (95% CI, 52.0–63.2) in the ribociclib group compared to 45.9% (95% CI, 36.9–54.5) in the placebo group (Figure 8)27. This equates to a 28% difference in the relative risk of death27.
Figure 8. Overall survival in the overall population for MONALEESA-3 (Adapted from Slamon et al.27). Note, the dashed lines represent the estimated overall survival at 36 months and 42 months. CI, confidence interval.
The results of an exploratory analysis of MONALEESA-3, with an extended follow-up, assessed the long-term overall survival (OS) benefits of ribociclib after an additional median follow-up of 16.9 months50.
At the data cut-off, the median follow-up was 56.3 months. At this point, 14.0% of patients were still on ribociclib with fulvestrant, and 8.7% of patients were on fulvestrant with placebo treatment.
The extended follow-up showed that ribociclib with fulvestrant continued to provide more than one year OS benefit (53.7 months), compared with fulvestrant plus placebo (41.5 months) (HR 0.73; CI, 0.59–0.90)50.
In the first-line subgroups, patients treated with ribociclib plus fulvestrant had prolonged OS, compared with patients receiving fulvestrant plus placebo (median, not reached vs 51.8 months; HR 0.64; 95% CI, 0.46–0.88)50. Second-line subgroups showed that ribociclib plus fulvestrant produced a 6 month longer median OS compared to placebo plus fulvestrant (median, 39.7 vs 33.7 months; HR 0.78; CI, 0.59–1.04)50.
Characterisation of the post-progression endpoints (Table 5) showed that time to second objective disease progression, time to chemotherapy (ChT), and ChT-free survival were more favourable in the ribociclib plus fulvestrant group than in fulvestrant plus placebo group.
Table 5. Characterisation of the post-progression endpoints in the MONALEESA-3 trial (Adapted from Slamon et al.50). CI, 95% confidence interval; CT, time to chemotherapy; FUL, fulvestrant; HR, hazardratio; MO, months; PBO, placebo; PFS2, second objective disease progression, RIB, ribociclib.
| Post-progression endpoints | RIB + FUL (n=484) | PBO + FUL (n=242) |
| PFS2 events, n (%) | 265 (54.8) | 163 (67.4) |
| Median, mo. | 37.4 | 28.1 |
| HR (CI) | 0.69 (0.57–0.84) | |
| Time to first CT, events, n (%) | 215 (44.4) | 131 (54.1) |
| Median, mo. | 48.1 | 28.8 |
| HR (CI) | 0.70 (0.57–0.88) | |
| CT-free survival, events, n (%) | 287 (59.3) | 178 (73.6) |
| Median, mo. | 32.3 | 22.4 |
| HR (CI) | 0.69 (0.57–0.83) | |
Further analyses highlighted a consistent OS benefit across the majority of subgroups compared with the intent-to-treat population and no new safety signals were reported during the follow-up50.
The final analysis of the key secondary endpoint of overall survival results from MONALEESA-2 were recently discussed at European Society for Medical Oncology (ESMO) 2021. At data cut-off on 10 June 2021, 47 patients remained on treatment (treatment arm: 30 [9.0%]; placebo arm: 17 [5.1%]) of the intention-to-treat population of 668 patients (treatment arm: 334; placebo arm: 334). The median follow-up was 79.7 months and final overall survival was assessed after 400 deaths (treatment arm: 181 [54.2%]; placebo arm: 219 [65.6%]). A significant overall survival benefit was observed in the treatment arm (ribociclib + letrozole), compared to the placebo arm (placebo + letrozole) (median, 63.9 vs 51.4 mo; HR 0.76; 95% CI, 0.63–0.93; P=0.004)51.
The estimated 6-year overall survival was 44.2% for ribociclib versus 32.0% for placebo, with time to first chemotherapy (median, 50.6 vs 38.9 mo; HR 0.74; 95% CI, 0.61–0.91) and chemotherapy-free survival (median, 39.9 vs 30.1 mo; HR 0.74; 95% CI, 0.62–0.89) also demonstrating positive results. In addition, no new safety signals were seen51.
Overall survival improvement was over 12 months after a median follow-up of over 6.5 years, in first-line ribociclib + letrozole versus placebo + letrozole. According to the authors, these results represent the first report of statistically significant overall survival benefit in postmenopausal patients with HR+/HER2− ABC treated with a CDK4/6 inhibitor in the first line51.
MONALEESA-7
The MONALEESA-7 trial included 672 pre-/perimenopausal women with HR+/HER2- metastatic or recurrent BC29. Patients received either ribociclib with a NSAI or tamoxifen plus goserelin or placebo with a NSAI or tamoxifen plus goserelin. The primary endpoint, mPFS, was 23.8 months (95% CI, 19.2–not reached) in the group treated with ribociclib and 13.0 months (95% CI, 11.0–16.4) in the placebo group (HR 0.55; 95% CI, 0.44–0.69; log-rank P<0.0001)29.
In addition, a prespecified interim analysis found that overall survival (OS) was significantly longer among those treated with a CDK4/6 inhibitor plus endocrine therapy as compared to those treated with ET alone30. At 42 months, estimated OS was 70.2% (95% CI, 63.5–76.0) among patients receiving ribociclib and 46.0% (95% CI, 32.0–58.9) among those receiving the placebo (Figure 9)30.
Figure 9. Overall survival in all patients assessed in the MONALEESA-7 clinical trial (Adapted from Im et al.30). NE indicates that the value could not be estimated. CI, confidence interval; HR, hazard ratio.
Safety
The most common adverse events recorded in the MONALEESA-2 trial are shown in Table 6. As in the PALOMA programme, despite the high frequency of neutropenia reported in association with ribociclib use, febrile neutropenia was only reported in 1.5% of cases25.
Table 5. Adverse events (≥25%) reported in MONALEESA-2 (adapted from Hortobagyi et al.25).
Ribociclib had a comparable safety profile in the MONALEESA-7 study trial. Neutropenia was the most common Grade 3/4 adverse event, followed by hot flush and leucopenia29.
The adverse event profiles were also similar between MONALEESA-2 and MONALEESA-3, including an increased incidence of Grade 3/4 elevated liver enzymes with ribociclib compared to placebo27.
A high rate of thromboembolic events was observed in the MONALESSA-3 study, with 23 patients (4.8%) experiencing pulmonary embolism after receiving treatment 27,28.
MONALEESA-2 and MONALEESA-3 also highlighted a need for careful patient monitoring, as prolongation of the QT interval by Fredericia was reported as a rare, but serious adverse event. This being said, most of the adverse events associated with ribociclib use can be managed, and dose modification recommendations are available27,28.
Dalpiciclib in advanced breast cancer
The DAWNA-1 trial was a randomised, double-blind, phase 3 trial of the investigational CDK4/6 inhibitor dalpiciclib (SHR6390) as monotherapy for pre-treated HR+/HER2− advanced breast cancer (ABC) or metastatic breast cancer (mBC) patients who had relapsed or progressed on previous endocrine therapy (ET)52,53.
361 patients were randomised (2:1) to receive the investigational drug dalpiciclib plus fulvestrant (n = 241) or placebo plus fulvestrant (n = 120). At baseline, approximately 60% of patients had visceral metastases and 45% were premenopausal or perimenopausal. The primary endpoint was investigator assessed progression-free survival (PFS) and as of November 2020, 71.4% of the total projected PFS events had occurred, and a pre-planned interim analysis was carried out52.
Efficacy
DAWNA-1
The investigator-assessed PFS was 15.7 months in the dalpiciclib-fulvestrant arm and 7.2 months in the placebo-fulvestrant arm (P<0.0001). The median PFS based on an independent review committee (IRC) assessment (Table 7) was 13.6 months and 7.7 months, respectively (P<0.0001)52.
In all prespecified subgroups, PFS favoured dalpiciclib plus fulvestrant, with a hazard ration (HR) of <1 irrespective of menopausal status, presence of visceral metastasis, or prior ET. Investigator and IRC assessed overall response rate (ORR) and clinical benefit rate (CBR) were observed to be higher in the dalpiciclib-fulvestrant group, compared with the placebo-fulvestrant group (Table 7)52.
Table 7. PFS based on independent review committee and investigator assessment (adapted52). CI, 95% confidence interval; CMH P, Cochran–Mantel–Haenszel p-value; Dalp, dalpiciclib; fulv, fulvestrant; HR, hazard ratio; IRC, independent review committee; INV, investigator; Mo, months; PBO, placebo; PFS, progression-free survival; ORR, overall response rate; NR, not reported; TFSCT, time to first subsequent chemotherapy.
| *1-sided stratified | ||||
| DALP-FULV (INV, n=241) |
PBO-FULV (INV, n=120) |
DALP-FULV (IRC, n=241) |
PBO-FULV (IRC, n=120) |
|
| Median PFS (CI), mo | 15.7 (11.1–NR) |
7.2 (5.6–9.2) |
13.6 (11.3–NR) |
7.7 (5.6–10.9) |
| PFS HR (CI) | 0.42 (0.31–0.58) |
- | 0.45 (0.32–0.64) |
- |
| Log-rank P* | <0.0001 | - | <0.0001 | - |
| Median TFSCT (CI), mo | NR (NR-NR) | 14.2 (9.7–NR) |
- | - |
| TFSCT HR (CI) | 0.47 (0.32–0.69) |
- | - | - |
| Log-rank P* | <0.0001 | - | - | - |
| ORR% (CI) | 27.0 (21.5–33.0) |
20.0 (13.3–28.3) |
30.3 (24.6–36.5) |
15.8 (9.8–23.6) |
| CMH P | 0.0727 | - | 0.0015 | - |
The benefit of dalpiciclib, a currently unapproved investigational CDK4/6 inhibitor, versus placebo extended beyond the initial study treatment with time to first subsequent chemotherapy (ChT) (Table 7). The risk of initiating the first subsequent ChT was reduced by 53% in the dalpiciclib-fulvestrant group compared to the placebo-fulvestrant group (P<0.0001)52.
The median duration of exposure was 9.4 and 9.9 months for dalpiciclib and fulvestrant in the dalpiciclib-fulvestrant group, respectively. In the placebo-fulvestrant group, the median duration of exposure was 6.1 months for fulvestrant52.
Safety
The most common adverse events in the dalpiciclib-fulvestrant group were neutropenia (84.2% dalpiciclib; 0% placebo) and leukopenia (62.1% dalpiciclib; 0% placebo)52.
Overall, the rates of serious adverse events and fatal adverse events were low and comparable between the treatment groups. Two patients in the dalpiciclib group (0.8%) and 4 in the placebo group (3.3%) had a fatal adverse event. Treatment was discontinued due to adverse events in 2.5% of patients in the dalpiciclib arm and 3.3% in the placebo arm52.
Dalpiciclib + pyrotinib: interim results of a phase 2 trial
Interim results of a phase II trial evaluating the novel CDK4/6 inhibitor dalpiciclib combined with pyrotinib for HER2+ ABC were recently presented at the European Society for Medical Oncology (ESMO) Congress 2021. The trial recruited patients who had HER2+ ABC, had received up to one line of systemic therapy in the advanced setting, and had not previously been treated with CDK4/6 inhibitors nor HER2-targeted tyrosine kinase inhibitors. The primary endpoint was objective response rate per RECIST 1.1. Of the 23 patients who were evaluable as of 13 April 2021, 65.2% achieved confirmed objective response rate (15 partial response, 6 stable disease, 2 progressive disease). Most of the adverse events experienced were tolerable, with only one patient requiring a reduction of dose. This investigational drug combined with pyrotinib shows promising efficacy and tolerable toxicity, and represents a potential future option as a completely oral, chemotherapy-free treatment regimen for HER2+ ABC patients. Second stage enrolment is currently underway54.
CDK4/6 inhibitor side-effect management
The cyclin-dependent kinase 4 and 6 inhibitors (CDK4/6 inhibitors) abemaciclib, palbociclib and ribociclib, show similar side effects, though with some differences13–15. Similar side effects associated with CDK4/6 inhibitor-based combination treatments include neutropenia or gastrointestinal events3,13–15.
Abemaciclib is structurally distinct from palbociclib and ribociclib, and is more selective for CDK4 than CDK63. CDK4 is important for breast tumorigenesis, while CDK6 is important in haematopoietic stem cell differentiation. CDK4 is associated with higher rates of diarrhoea and fatigue than CDK6, but lower rates of haematological side effects, including neutropenia3,14–15. In contrast to palbociclib, ribociclib has a higher incidence of QT interval prolongation14,15. The most common side effect for palbociclib and ribociclib is neutropenia14,15.
CDK4/6 inhibitor-associated toxicity can be managed by dose reductions or dose modifications3,14,48. Early monitoring with regular clinical assessments and management of side effects is important3,14,48. Accurate communication between the patient and clinician can avert treatment-related misunderstandings3,14,48.
Dr Laura Spring, a clinical/translational investigator and breast medical oncologist at the Massachusetts General Hospital Cancer Center and Harvard Medical School, summarises the CDK4/6 inhibitor toxicities as reported in pivotal clinical trials.
Not all CDK4/6 inhibitor-related side-effects observed in the clinical management of breast cancer have been reported in clinical trials. In our next videos, Dr Veronique Dieras and Professor Nadia Harbeck explain what additional CDK4/6 inhibitor-related side-effects clinicians could observe in clinical practice.
Management of CDK4/6 inhibitor-related haematological side effects
Neutropenia
The main CDK4/6-associated toxicities are neutropenia and leukopenia13–15. Neutropenia typically manifests 15 days following the first dose of palbociclib or ribociclib. With abemaciclib, neutropenia occurs within the first two cycles and infrequently in later cycles. The timing of patient monitoring is therefore important.
For a correct evaluation of the different blood cell counts, it is recommended to evaluate the complete blood count prior to the start of CDK4/6 inhibitor-based treatment, at the beginning of each new treatment cycle and on day 14 or 15 of cycle 1 and 2 (Table 8)3,14,15,54-56.
Table 8. Requirements for monitoring complete blood count during the treatment with CDK4/6 inhibitors (Adapted from Ettl et al.56).
Neutropenia is managed by dose interruption and dose modification of the CDK4/6 inhibitor while continuing endocrine agents (Table 9)3,14,15,54-56.
Interestingly, a retrospective study of 78 patients who commenced treatment with palbociclib between December 2016 and January 2021 found a significant association between early treatment-related neutropenia and prolonged overall survival. The results suggest that palbociclib dosing could be guided by neutropenia, potentially serving as a pharmacodynamic marker57.
Table 9. Dosing recommendations for CDK4/6 inhibitors in combination with endocrine therapy inhibitors (Adapted from Ettl et al.56).
| Dose level | Palbociclib | Ribociclib | Abemaciclib |
| Recommended starting dose | 125 mg daily 3/4 weeks |
600 mg daily 3/4 weeks |
200 mg twice daily |
| First dose reduction | 100 mg daily 3/4 weeks |
400 mg daily 3/4 weeks |
150 mg twice daily |
| Second dose reduction | 75 mg daily 3/4 weeks |
200 mg daily 3/4 weeks |
100 mg twice daily |
CDK4/6 inhibitor-related nonhaematological adverse events
QTc prolongation
Long QT syndrome can cause fast, irregular heartbeats. QTc prolongation is distinguished into three clinically relevant categories. In women, the cut-off points as measured by electrocardiogram (ECG) are ≤450 ms (normal), 450–470 ms (borderline), and more than 470 ms (prolonged).
ECGs can be assessed prior to initiation of CDK4/6 inhibitor treatment. ECG assessment can be repeated at approximately day 14 or 15 of the first cycle, and at the beginning of the second cycle, or as clinically indicated3,14,15,54-56.
Ribociclib prolongs the QT interval in a concentration-dependent manner15. Therefore, regular ECG monitoring is required (Table 10)15,56.
Table 10. ECG and QTc monitoring with ribociclib (Adapted from Ettl et al.56).
| Before treatment | Cycle 1 | Cycle 2 | Cycle 3+ | ||
| day 1 | day 14 | day 1 | day 14 | day 1 | |
| x | x | x | as indicated | ||
It is recommended that patients who are at risk of developing QTc prolongation are not treated with ribociclib15,56. Palbociclib has had no clinically relevant effect on the QTc interval in breast cancer14,54,56.
Elevation of liver enzymes
A side effect observed with anti-endocrine CDK4/6 inhibitor-based combination treatment is an asymptomatic increase of the liver enzymes alanine aminotransferase (ALT) and aspartate transaminase (AST)3,14,15,56.
Regular liver function tests can identify abnormal liver function following CDK4/6 inhibitor-based treatment (Table 11). Concomitant medication, alcohol abuse and hepatitis in medical history are recommended for evaluation3,14,15,56.
Table 11. Liver function monitoring requirements with ribociclib and abemaciclib (Adapted from Ettl et al.56).
| a If grade ≥2 abnormalities are noted, more frequent monitoring is recommended. | |||||||
| Cycle 1 | Cycle 2 | Cycles 3–4 | Cycles 5–6 | Cycles 6+ | |||
| day 1 | day 14 | day 1 | day 14 | day 1 | day 1 | ||
| Ribocicliba | x | x | x | x | x | x | as indicated |
| Abemaciclib | x | x | x | x | as indicated | as indicated | as indicated |
In clinical practice, routine monitoring procedures are conducted in patients treated with CDK4/6 inhibitors, including performing complete blood counts, liver function tests, and evaluation of the QTc interval3,14,15,48
Some clinicians manage CDK4/6 inhibitor-related side effects in unique ways. Watch Dr Laura Spring and Professor Nadia Harbeck describe some of these ways.
Gastrointestinal toxicities
Gastrointestinal CDK4/6 inhibitor-related side effects are nausea, vomiting and diarrhoea13,14,15. For palbociclib and ribociclib, these toxicities occur at low grades; abemaciclib has a different gastrointestinal toxicity profile and a higher rate of grade 3 diarrhoea3,14,15,54–56.
Diarrhoea requires regular monitoring. Following symptom manifestation, diarrhoea should be treated with hydration and dietary modifications, provided no signs of infection are detected. Blood tests can identify alterations in changed electrolyte levels due to diarrhoea. Anti-diarrhoeal medications, such as loperamide, can prevent complications. Nausea and vomiting are managed with antiemetics3,14,15,54–56.
Pulmonary embolism
CDK4/6 inhibitor-based combination treatment is rarely associated with thromboembolic events, which however, can be severe. Typical symptoms include shortness of breath, hypoxia, chest pain, rapid breathing, or rapid heart rate. Patients should be frequently monitored for signs and symptoms of a pulmonary embolism3,14,15,56.
For a patient who has not been initiated on CDK4/6 inhibitors for breast cancer, do the potential benefits of these drugs outweigh the potential side effects?
Dr Laura Spring responds to this question in this video.
References
- Gil-Gil M, Alba E, Gavilá J, de la Haba-Rodríguez J, Ciruelos E, Tolosa P, et al. The role of CDK4/6 inhibitors in early breast cancer. Breast. 2021;58:160-169.
- Abemaciclib, VERZENIO® | Highlights of Prescribing Information. 2023. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/208716s006s007s008lbl.pdf. Accessed 2023.
- Abemaciclib, Verzenios® SmPC. 2022. Available at: https://www.medicines.org.uk/emc/product/9532/smpc.
- Harbeck N, Rastogi P, Martin M, Tolaney SM, Shao ZM, Fasching PA, et al. Adjuvant abemaciclib combined with endocrine therapy for high-risk early breast cancer: updated efficacy and Ki-67 analysis from the monarchE study. Ann Oncol. 2021;32(12):1571-1581.
- Johnston SRD, Harbeck N, Hegg R, Toi M, Martin M, Shao ZM, et al. Abemaciclib Combined With Endocrine Therapy for the Adjuvant Treatment of HR+, HER2-, Node-Positive, High-Risk, Early Breast Cancer (monarchE). J Clin Oncol. 2020;38(34):3987-3998.
- Giordano SH, Freedman RA, Somerfield MR, Chemotherapy ftOA, Panel TTGE. Abemaciclib With Endocrine Therapy in the Treatment of High-Risk Early Breast Cancer: ASCO Optimal Adjuvant Chemotherapy and Targeted Therapy Guideline Rapid Recommendation Update. J Clin Oncol. 2022;40(3):307-309.
- Johnston SRD, Toi M, O'Shaughnessy J, Rastogi P, Campone M, Neven P, et al. Abemaciclib plus endocrine therapy for hormone receptor-positive, HER2-negative, node-positive, high-risk early breast cancer (monarchE): results from a preplanned interim analysis of a randomised, open-label, phase 3 trial. The Lancet Oncology. 2023;24(1):77-90.
- Slamon DJ, Fasching PA, Patel R, Verma S, Hurvitz SA, Chia SKL, et al. NATALEE: Phase III study of ribociclib (RIBO) + endocrine therapy (ET) as adjuvant treatment in hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2–) early breast cancer (EBC). Journal of Clinical Oncology. 2019;37(15_suppl):TPS597-TPS597.
- Gnant M, Dueck AC, Frantal S, Martin M, Burstein HJ, Greil R, et al. Adjuvant Palbociclib for Early Breast Cancer: The PALLAS Trial Results (ABCSG-42/AFT-05/BIG-14-03). J Clin Oncol. 2022;40(3):282-293.
- Loibl S, Marmé F, Martin M, Untch M, Bonnefoi H, Kim SB, et al. Palbociclib for Residual High-Risk Invasive HR-Positive and HER2-Negative Early Breast Cancer-The Penelope-B Trial. J Clin Oncol. 2021;39(14):1518-1530.
- . Novartis Kisqali® Phase III NATALEE trial meets primary endpoint at interim analysis demonstrating clinically meaningful benefit in broad population of patients with early breast cancer [press release]. Available at: https://www.novartis.com/news/media-releases/novartis-kisqali-phase-iii-natalee-trial-meets-primary-endpoint-interim-analysis-demonstrating-clinically-meaningful-benefit-broad-population-patients-early-breast-cancer. Accessed May 2023.
- Mayer EL, Fesl C, Hlauschek D, Garcia-Estevez L, Burstein HJ, Zdenkowski N, et al. Treatment Exposure and Discontinuation in the PALbociclib CoLlaborative Adjuvant Study of Palbociclib With Adjuvant Endocrine Therapy for Hormone Receptor-Positive/Human Epidermal Growth Factor Receptor 2-Negative Early Breast Cancer (PALLAS/AFT-05/ABCSG-42/BIG-14-03). J Clin Oncol. 2022;40(5):449-458.
- Rugo HS, O'Shaughnessy J, Boyle F, Toi M, Broom R, Blancas I, et al. Adjuvant abemaciclib combined with endocrine therapy for high-risk early breast cancer: safety and patient-reported outcomes from the monarchE study. Ann Oncol. 2022;33(6):616-627.
- Palbociclib, IBRANCE® SmPC. 2020. Available at: https://www.ema.europa.eu/en/documents/product-information/ibrance-epar-product-information_en.pdf.
- Ribociclib, KISQALI® SmPC. 2020. Available at: https://www.ema.europa.eu/en/documents/product-information/kisqali-epar-product-information_en.pdf.
- Palbociclib, IBRANCE® | Highlights of Prescribing Information. 2019. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212436lbl.pdf. Accessed 2020.
- Dickler MN, Tolaney SM, Rugo HS, Cortes J, Dieras V, Patt D, et al. MONARCH 1, a phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, n patients with refractory HR+/HER2- metastatic breast cancer. Clinical Cancer Research. 2017;23(17):5218-5224.
- Rugo HS, Tolaney SM, Cortés J, Diéras V, Patt DA, Wildiers H, et al. Abstract CT044: MONARCH 1: Final overall survival analysis of a phase 2 study of abemaciclib, a CDK4 and CDK6 inhibitor, as monotherapy, in patients with HR+/HER2- breast cancer, after chemotherapy for advanced disease. Presented at the Cancer Research 2017, 2017/7//.
- Sledge GW, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. The Effect of Abemaciclib Plus Fulvestrant on Overall Survival in Hormone Receptor-Positive, ERBB2-Negative Breast Cancer That Progressed on Endocrine Therapy - MONARCH 2: A Randomized Clinical Trial. JAMA Oncology. 2020;6(1):116-124.
- Sledge GW, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2-advanced breast cancer who had progressed while receiving endocrine therapy. Journal of Clinical Oncology. 2017;35(25):2875-2884.
- Goetz MP, Toi M, Campone M, Trédan O, Bourayou N, Sohn J, et al. MONARCH 3: Abemaciclib as initial therapy for advanced breast cancer. Journal of Clinical Oncology. 2017;35(32):3638-3646.
- Johnston S, Martin M, Di Leo A, Im SA, Awada A, Forrester T, et al. MONARCH 3 final PFS: a randomized study of abemaciclib as initial therapy for advanced breast cancer. npj Breast Cancer. 2019;5(1):1-8.
- Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. The Lancet Oncology. 2016;17(4):425-439.
- Finn RS, Martin M, Rugo HS, Jones S, Im S-A, Gelmon K, et al. Palbociclib and Letrozole in Advanced Breast Cancer. New England Journal of Medicine. 2016;375(20):1925-1936.
- Hortobagyi GN, Stemmer SM, Burris HA, Yap Y-S, Sonke GS, Paluch-Shimon S, et al. Ribociclib as First-Line Therapy for HR-Positive, Advanced Breast Cancer. New England Journal of Medicine. 2016;375(18):1738-1748.
- Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Annals of Oncology. 2018;29(7):1541-1547.
- Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im S-A, et al. Overall Survival with Ribociclib plus Fulvestrant in Advanced Breast Cancer. New England Journal of Medicine. 2020;382(6):514-524.
- Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im SA, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. Journal of Clinical Oncology. 2018;36(24):2465-2472.
- Tripathy D, Im SA, Colleoni M, Franke F, Bardia A, Harbeck N, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. The Lancet Oncology. 2018;19(7):904-915.
- Im S-A, Lu Y-S, Bardia A, Harbeck N, Colleoni M, Franke F, et al. Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. New England Journal of Medicine. 2019;381(4):307-316.
- Fouda MM, Kuriakose V. CDK4/6 inhibitors in clinical practice during COVID-19 pandemic: Comparative analysis of the clinical impact of the pandemic for metastatic breast cancer patients during first and second waves in the UK. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 243P.2021.
- Huang CS, Toi M, Im YH, Iwata H, Sohn J, Wang HC, et al. 45O Abemaciclib plus fulvestrant in East Asian women with HR+, HER2- advanced breast cancer: Overall survival from MONARCH 2. Annals of Oncology. 2020;31(S6):S1258-S1259.
- Trujillo JL-G, Gomez ME, Sohn JH, Im Y, Wang H, Cussac AL, et al. Abemaciclib plus fulvestrant in participants with HR+/HER2- advanced breast cancer: A pooled analysis of the endocrine therapy naïve (EN) participants in MONARCH 2. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 241P.2021.
- Di Leo A, O’Shaughnessy J, Sledge GW, Martin M, Lin Y, Frenzel M, et al. Prognostic characteristics in hormone receptor-positive advanced breast cancer and characterization of abemaciclib efficacy. npj Breast Cancer. 2018;4(1):41-41.
- Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): A randomised phase 2 study. The Lancet Oncology. 2015;16(1):25-35.
- Rugo HS, Im S, Joy AA, Yaroslav S, Walshe JM, Sleckman B, et al. Effect of palbociclib (PAL) + endocrine therapy (ET) on time to chemotherapy (TTC) across subgroups of patients (pts) with hormone receptor-positive/human epidermal growth factor receptor 2-negative (HR+/HER2-) advanced breast cancer (ABC): Post hoc analy. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 234P2021.
- Rugo HS, Finn RS, Diéras V, Ettl J, Lipatov O, Joy AA, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Research and Treatment. 2019;174(3):719-729.
- Rugo HS, Diéras V, Gelmon KA, Finn RS, Slamon DJ, Martin M, et al. Impact of palbociclib plus letrozole on patient-reported health-related quality of life: Results from the PALOMA-2 trial. Annals of Oncology. 2018;29(4):888-894.
- Behrouzi R, Moon S, Eaton D. Predictors of progression-free survival in patients with metastatic breast cancer receiving palbociclib with letrozole. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 327P.2021.
- Turner NC, André F, Cristofanilli M, Verma S, Iwata H, Loi S, et al. Abstract P4-22-06: Treatment postprogression in women with endocrine-resistant HR+/HER2- advanced breast cancer who received palbociclib plus fulvestrant in PALOMA-3. Presented at the Cancer Research 2017, 2017/2//.
- Cristofanilli M, Rugo HS, Im S-A, Slamon DJ, Harbeck N, Bondarenko I, et al. Overall survival (OS) with palbociclib (PAL) + fulvestrant (FUL) in women with hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2–) advanced breast cancer (ABC): Updated analyses from PALOMA-3. Presented at the American Society of Clinical Oncology (ASCO) congress 2021, 4–8 June 2021, Virtual. 1000.2021.
- Xu B, Hu X, Li W, Sun T, Shen K, Wang S, et al. PALOMA-4: Primary results from a phase III trial of palbociclib (PAL) + letrozole (LET) vs placebo (PBO) + LET in Asian postmenopausal women with estrogen receptor–positive/human epidermal growth factor receptor 2–negative (ER+/HER2–) advanced breast canc. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 228MO.2021.
- Serra F, Lapidari P, Quaquarini E, Tagliaferri B, Sottotetti F, Palumbo R. Palbociclib in metastatic breast cancer: Current evidence and real-life data. Drugs in Context. 2019;8:212309-212309.
- Rugo HS, Liu X, Li B, McRoy L, Layman R, Brufsky A. Real-world comparative effectiveness of palbociclib plus letrozole vs letrozole in older patients with metastatic breast cancer. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 236P.2021.
- Palmieri C, Musson A, Harper-wynne C, Wheatley D, Bertelli G, MacPherson I, et al. A real-world data analysis: The first United Kingdom experience of cyclin-dependent kinase 4/6 inhibitor in advanced breast cancer in the National Health Service within an access program. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 240P.2021.
- Badri SE, Tahir B, Balachandran K, Bezecny P, Britton F, DeSouza K, et al. Palbociclib combined with aromatase inhibitors (AIs) in women ≥75 years with oestrogen receptor positive (ER+ve), human epidermal growth factor receptor 2 negative (HER2-ve) advanced breast cancer: A real-world multicentre UK study. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 245P.2021.
- Rocque G, Blum J, Montero A, Sonnier S, McCune S, Gallagher C, et al. Treatment patterns in black and indigenous people and people of color (BIPOC) receiving palbociclib for hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2-) advanced breast cancer (ABC) in a real-world setting: POLARIS. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 315P.2021.
- Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Annals of Oncology. 2020;31(12):1623-1649.
- Decker T, Fasching PA, Nusch A, Hartkopf A, Heinrich BJ, Kurbacher CM, et al. 247P Efficacy and safety of ribociclib (RIB) in combination with letrozole (LET) in patients with estrogen receptor–positive advanced breast cancer (ABC): Secondary and exploratory results of phase 3b RIBECCA study. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 247P.2021.
- Slamon DJ, Neven P, Chia SKL, Jerusalem GHM, De Laurentiis M, Im S-A, et al. Updated overall survival (OS) results from the phase III MONALEESA-3 trial of postmenopausal patients (pts) with HR+/HER2- advanced breast cancer (ABC) treated with fulvestrant (FUL) ± ribociclib (RIB). Presented at the American Society of Clinical Oncology (ASCO) congress 2021, 4–8 June 2021, Virtual. 1001.2021.
- Hortobagyi GN, Stemmer SM, Iii HAB, Yap YS, Sonke GS, Hart L, et al. Overall survival (OS) results from the phase III MONALEESA-2 (ML-2) trial of postmenopausal patients (pts) with hormone receptor positive/human epidermal growth factor receptor 2 negative (HR+/HER2−) advanced breast cancer (ABC) treated with endocrine the. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. LBA17_PR.2021.
- Xu B, Zhang Q, Zhang P, Hu X, Li W, Tong Z, et al. Dalpiciclib or placebo plus fulvestrant in hormone receptor-positive and HER2-negative advanced breast cancer: a randomized, phase 3 trial. Nat Med. 2021;27(11):1904-1909.
- Xu B, Zhang Q, Zhang P, Hu X, Li W, Tong Z, et al. Dalpiciclib versus placebo plus fulvestrant in HR+/HER2- advanced breast cancer that relapsed or progressed on previous endocrine therapy (DAWNA-1): A multicenter, randomized, phase 3 study. Presented at the American Society of Clinical Oncology (ASCO) congress 2021, 4–8 June 2021, Virtual. 1002.2021.
- Spring LM, Zangardi ML, Moy B, Bardia A. Clinical Management of Potential Toxicities and Drug Interactions Related to Cyclin‐Dependent Kinase 4/6 Inhibitors in Breast Cancer: Practical Considerations and Recommendations. The Oncologist. 2017;22(9):1039-1048.
- Thill M, Schmidt M. Management of adverse events during cyclin-dependent kinase 4/6 (CDK4/6) inhibitor-based treatment in breast cancer. Therapeutic Advances in Medical Oncology. 2018;10:1-12.
- Ettl J. Management of adverse events due to cyclin-dependent kinase 4/6 inhibitors. Breast Care. 2019;14(2):86-92.
- Sala XF, Mestres JA, Conde D. Palbociclib: Early treatment-related neutropenia as a potential pharmacodynamic marker? Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 250P.2021.
This content has been developed independently by Medthority who previously received educational funding from Eli Lilly in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
