Breast cancer
Early and advanced breast cancer
Cancer is a leading cause of death and a burden to global life expectancy1,2. Breast cancer (BC) in women accounts for 1 in 4 cancer cases, with an estimated 2.3 million new cases in 20201. The increased incidence rates of BC in women reflects reproductive, hormonal, lifestyle risk factors and improved mammographic screening1.
Gene expression and molecular profiles are used to characterise BC subtypes3,4. Progesterone (PR) signalling may play a role in the progression of early breast cancer (EBC)3; oestrogen (ER) or PR receptors can be prognostic of therapy response; ERα is usually maintained in metastatic breast cancer (mBC)4. Gene expression profiling of triple-negative breast cancer (TNBC) has aided in delineating disease subtypes5.
EBC is disease confined to the breast, with or without regional lymph node involvement, and the absence of distant metastatic disease3. Advanced breast cancer (ABC) includes inoperable locally ABC (LABC) and mBC, and is manageable, though incurable, with currently approved treatments4.
- Breast cancer epidemiology
- Factors responsible for increasing global incidence rates of breast cancer
- Early breast cancer
- Advanced breast cancer
- Breast cancer pathophysiology
- Hormone receptors and breast cancer progression
- HER2 and breast cancer progression
- Progression of triple-negative breast cancer
- Review
Breast cancer epidemiology
Cancer is a leading cause of death and an important barrier to increasing life expectancy in every country of the world1,2. According to the World Health Organization (WHO), cancer is the first or second leading cause of death before the age of 70 years in 112 of 183 countries and ranks third or fourth in a further 23 countries (Figure 1)1,2.
Figure 1. National ranking of cancer as a cause of death at ages <70 years in 2020 (Adapted from WHO, 20201).
The increasing prominence of cancer as a leading cause of death partly reflects declines in mortality rates of stroke and coronary heart disease, compared with cancer, in many countries1.
Overall, the burden of cancer incidence and mortality is rapidly growing worldwide. This increase is partly due to ageing and growth of the population, and changes in the prevalence and distribution of the main risk factors for cancer1.
In 2020, breast cancer in women surpassed lung cancer as the leading cause of global cancer incidence, with an estimated 2.3 million new cases, signifying 11.7% of all cancer cases1. It is the fifth leading cause of cancer mortality globally, with 685,000 deaths1
BC in women accounts for 1 in 4 cancer cases, and for 1 in 6 cancer deaths, ranking first for incidence in 159 countries (Figure 2), and for mortality in 110 countries (Figure 3).
Figure 2. Most common type of cancer incidence in women in 2020 by country (Adapted from WHO, 20202).
Figure 3. Most common type of cancer mortality in women in 2020 by country (Adapted from WHO, 20202).
Factors responsible for increasing global incidence rates of breast cancer
The increased incidence rates of BC in women in higher Human Development Index (HDI) countries reflects the influence of several factors1:
- reproductive risk factors (advanced age at first birth, fewer children, less breastfeeding, oral contraceptives)
- hormonal risk factors (early age at menarche, later age at menopause, menopausal hormone therapy)
- lifestyle risk factors (alcohol consumption, obesity, physical inactivity)
- improved cancer detection through organised or opportunistic mammographic screening
Early breast cancer
Early breast cancer (EBC) is confined to the breast, with or without regional lymph node involvement, and the absence of distant metastatic disease3.
This definition is based on several considerations. EBC is potentially curable, whereas inoperable locally advanced breast cancer (LABC) and metastatic breast cancer (mBC) are not.
In top-ranked countries listed in the higher Human Development Index (HDI), more than 80% of patients with EBC have long-term survival following surgery or systemic therapies such as chemotherapy, hormone therapy, targeted therapy, or local radiation. By contrast, patients with LABC and mBC are rarely long-term survivors3.
Approximately 30% of patients with EBC progress to mBC. For hormone receptor-positive (HR+) EBC, a common breast cancer subtype, risk of recurrence is high, even in patients with longer disease-free periods (>5 years) following endocrine therapy (ET)6–8.
Prognostic biomarkers can help identify risk (high/low) and type (early/late) of recurrence in EBC patients, and recently developed risk stratification tools can now assess both clinicopathological and molecular properties of EBC7–11.
Learn more about risk stratification tools for patients at high-risk of cancer recurrence in section 3, ‘Breast cancer stratification3,7
In terms of novel treatments for EBC, ongoing clinical trials are assessing cyclin-dependent kinases 4 and 6 inhibitors (CDK4/6 inhibitors) in the adjuvant setting for HR+/human epidermal growth factor receptor 2-negative (HER2-) EBC.
Advanced breast cancer
Advanced breast cancer (ABC) includes inoperable LABC and mBC4.
ABC is largely an incurable disease, with a median overall survival (OS) of approximately 3 years and a 5-year survival rate of roughly 25%4. Survival is strongly associated with BC subtype, with major advances observed in human epidermal growth factor receptor 2-positive (HER2+) ABC4.
Despite being incurable, ABC is a manageable disease. However, the impact of available therapies on survival and quality of life (QoL) of ABC patients has been slow and different, compared with recurrent ABC, with recurrent ABC which is harder to manage4.
Outcomes for patients with ABC are associated with access to the best available care, which includes the best available medicines, multidisciplinary, specialised care, implementation of guidelines, high-quality pathology, imaging and radiotherapy (RT).
Mortality rates for ABC have decreased in the majority of higher HDI countries; most ABC-related deaths occur in less developed countries, and access issues partly account for many of these inequalities4.
Learn clinical trial data on CDK4/6 inhibitors in managing advanced breast cancer
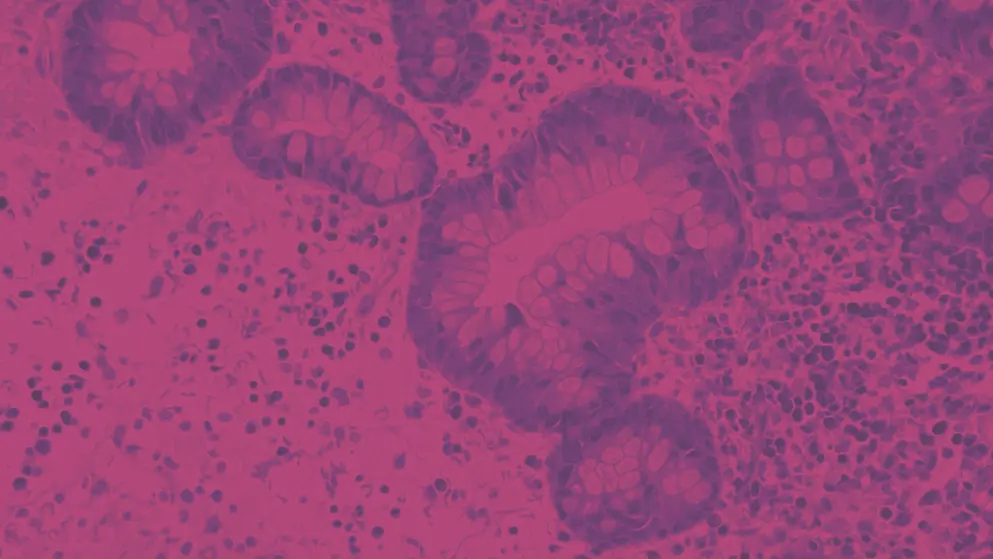
Breast cancer pathophysiology
BC is a heterogeneous disease clinically classified by immunohistochemical (IHC) staining of three receptors:
- oestrogen receptor (ER)
- progesterone receptor (PR)
- human epidermal growth factor receptor 2 (HER2)
Studies conducted in the early 2000s demonstrated that gene expression signatures could classify BC into distinct and reproducible molecular subgroups (Table 1)12–14.
Table 1. Classification of breast cancer on the basis of receptor expression profile (Adapted from Makki et al.12; Tungsukruthai et al.13; Cardoso et al.14).
| ER, oestrogen receptor; HER2, human epidermal growth factor receptor-2; Ki-67, proliferation marker protein Ki-67; PR, progesterone receptor. | |
| Molecular subtype | Expression profile |
| Luminal-type A | ER+ and/or PR+, HER2- |
| Luminal-type B | ER+ and/or PR+, HER2+ or HER2- and high Ki-67 |
| HER2-enriched | ER-, PR-, HER2+ |
| Triple-negative/basal-like | ER-, PR-, HER2- |
Luminal A-like tumours are typically low grade, strongly ER+/PR+, HER2- and have low proliferative fraction. Luminal B-like tumours are ER+, but may have variable degrees of ER/PR expression, are higher grade and have higher proliferative fraction4.
Given the heterogeneity of breast cancer and the different molecular drivers, treatment needs to be tailored to the individual and the characteristics of their condition
The importance of assessing the expression profiles for HER2 and HR, such as ER or PR, is shown by the fact that they can be both prognostic and predictive of therapy response15.
In our next section, we discuss more about the clinical assessment of breast cancer risk
Hormone receptors and breast cancer progression
The majority of BCs are hormone receptor positive (HR+). This means that ≥1% of tumour cells have positive nuclear staining for ER and/or PR via immunohistochemistry (IHC)16. A cut-off of 1% is used, as patients with even these low levels may benefit from hormonal therapy17. The increase in hormone receptor expression commonly observed in BC cells suggests a switch from paracrine to autocrine signalling by steroid hormones18-20.
Concerns have been raised, however, on the benefit of endocrine therapy for tumours with 1–10% ER expression, termed ‘ER‐low positive’21,22. This subgroup accounts for 2–3% of all ER-positive tumours and is less responsive to endocrine therapy than ER-high positive tumours21,22. The data regarding the efficacy and benefit of endocrine therapy for ER-low-positive BC is limited, 21,22.
Concerns have been raised, however, on the benefit of endocrine therapy for tumours with 1–10% ER expression, termed ‘ER‐low positive’21,22. This subgroup accounts for 2–3% of all ER-positive tumours and is less responsive to endocrine therapy than ER-high positive tumours21,22. The data regarding the efficacy and benefit of endocrine therapy for ER-low-positive BC is limited, but suggests possible benefit, so patients are still considered eligible. There are data to suggest that invasive ER-low positive cancers exhibit behaviour and gene profiles more similar to ER-negative cancers, making it critical that molecular and genetic tools are used to accurately assess the molecular nature of ER-low positive tumours and the optimal treatment strategy for this subgroup21,22.
Interestingly, the expression of ERα, the predominant form of the receptor in the mammary epithelium, is frequently maintained in mBC, and is still expressed in 65–70% of distant metastases23. Signalling via ERα has been shown to promote cell proliferation, survival, migration and epithelial-mesenchymal transition—all key factors in the development of many cancers (Figure 4)23.
Figure 4. Nuclear and extranuclear actions of ERα signalling in breast cancer (Adapted from Saha Roy & Vadlamudi23). EMT, epithelial-mesenchymal transition; ER, oestrogen receptor; MMP, matrix metalloproteinases.
Triple-negative breast cancer (TNBC) lacks ERα and PR, and has few (if any) HER2 receptors; however, expression of ERβ and G protein-coupled oestrogen receptor 1 (GPER-1) triggers oestrogen-responsivity in BC24. Oestrogen signalling in TNBC can also be activated and modulated by oestrogen-related receptors (ERRs). TNBC, therefore, may be responsive to oestrogen through ERα-independent pathways24.
ER-positive (ER+) BC can recur beyond 5 years, and before 5 years, from diagnosis7. Clinical and genomic expression models can help stratify these patients for risk of late recurrence7.
The signalling pathways activated as a consequence of elevated PR levels are less well defined.
Progesterone has been observed to stimulate mammary stem cells and promote cell proliferation resulting in a hypothesis that progesterone signalling plays a role in the progression of EBC25.
However, its role appears to be context dependent. Where it may play a role in the early stages of BC, in breast carcinoma, it can antagonise oestrogen signalling and its presence is associated with favourable prognosis, less aggressive cancer and better overall survival26.
HER2 and breast cancer progression
HER2 is a proto-oncogene encoding a transmembrane tyrosine kinase growth factor that is a member of the epidermal growth factor receptor (EGFR) family. Approximately 20% of breast cancers are positive for HER2, with assessment usually by IHC, although fluorescent in situ hybridisation (FISH) can be used when IHC is equivocal17,27.
Activation and dimerisation of the HER2 receptor with another member of the HER family of receptors results in activation of intracellular signalling pathways promoting cell proliferation, growth, survival and motility (Figure 5)28.
Figure 5. HER2 activation and signalling in breast cancer (Adapted28). 611 CTF, 611 carboxy-terminal fragment; AKT, protein kinase B; HER1, 2 or 3, human epidermal growth factor receptor 1, 2 or 3; mTOR, mammalian target of rapamycin; PI3K, phosphatidylinositol 3-kinase.
Progression of triple-negative breast cancer
TNBC, without the characteristic ERα, PR and/or HER2 expression of most (80–85%) BCs, is a complex and aggressive subtype that causes a disproportionate number of deaths (~25%)29,30.
TNBCs are more likely than non-TNBCs to metastasise within 5 years of diagnosis, while the median time to death and overall survival are also worse31,32.
Gene expression profiling of TNBC has helped characterise four subtypes (basal-like-1, basal-like-2, luminal androgen receptor and mesenchymal)5. However, significant molecular heterogeneity is observed within these subtypes and each of the four subtypes has been observed to co-occur within a single tumour33,34.
Review
- In 2020, breast cancer in women accounted for an estimated 2.3 million new cases1
- Incidence of breast cancer in women is influenced by reproductive, hormonal, lifestyle risk factors, and improved mammographic screening1
- Early breast cancer is confined to the breast, without distant metastatic disease, and with or without regional lymph node involvement3
- Advanced breast cancer is inoperable locally advanced breast cancer and metastatic breast cancer, and is manageable, but incurable4
- Oestrogen or progesterone receptors can be prognostic of therapy response3,4
- Gene expression profiling of triple-negative breast cancer has described some subtypes of breast cancer5
Approximately one-third of patients with early breast cancer progress to metastatic breast cancer1. Risk of cancer recurrence is high in patients with hormone receptor positive early breast cancer1
Breast cancer risk
Women at high risk of breast cancer (BC) are those with35
- a strong family history of breast, ovarian or pancreatic cancer
- diagnosis of BC before the age of 50 years
- diagnosis of triple-negative breast cancer (TNBC) before the age of 60 years
- personal history of ovarian cancer or second BC
Phenotypic markers that identify people who carry pathogenic mutations that increase the risk of BC are not currently known. A family history evaluation is therefore necessary to assess the risk of predisposing genes for BC in a family4,35.
More than 90% of patients with BC are diagnosed with early-stage disease, of whom approximately 70% have cancers that are hormone receptor-positive (HR+) and human epidermal growth factor receptor 2-negative (HER2-)14.
Although many patients with HR+/HER2- BC will not have recurrence, or distant recurrence on standard adjuvant endocrine therapy (ET), up to 20% of patients may have recurrence in the first 10 years, often with distant metastases, at which time the disease is incurable36.
For those patients with high-risk clinical and/or pathological features, risk of recurrence is higher, especially during the first few years on adjuvant ET37.
It is therefore critical to optimise risk assessment and adjuvant therapy to prevent early recurrences and metastases3. This section focuses on current tools and approaches used in BC risk assessment.
Assessment of breast cancer risk
Healthcare professionals may assess BC risk using these approaches8,14,35:
- Identify patients at risk of a germline mutation and offer them formal genetic testing
- For patients who do not meet the criteria for genetic testing, or who test negative for germline mutations, quantify the risk of developing cancer over a specified length of time
With the resulting assessment information, surveillance or lifestyle, pharmacological or surgical interventions can be administered to improve a patient’s risk profile (Figure 6)35.
Figure 6. Assessment in women at risk of breast cancer (Adapted35).
BC risk is multifactorial. Hence, optimal risk assessment of BC involves consideration of clinicopathological, molecular and genetic factors.
Risk assessment of breast cancer: clinicopathological factors
Important clinicopathological factors used in BC risk assessment are3,4:
- expression of ER/PR, HER2 and proliferation markers, such as Ki-67
- gene expression assay
- number of involved regional lymph nodes
- tumour histology
- tumour stage (tumour size, presence of peritumoural vascular invasion)
- histological grade
Immunohistochemically detected tumour markers are incorporated into the eighth edition of the American Joint Committee on Cancer (AJCC) Tumour, Node, Metastasis (TNM) to improve risk assessment, which also uses genomic assays to downstage some ER+, lymph node-negative tumours3,4.
As asymptomatic distant metastases are rare, comprehensive laboratory testing, including tumour markers and radiological staging, is not necessary for all patients. Minimum blood work-up, including a full blood count, liver and renal function tests, alkaline phosphatase and calcium levels, is advised before surgery and systemic (neo)adjuvant therapy3.
In patients at higher risk of BC—high tumour burden, aggressive biology, signs, symptoms or laboratory values suggesting the presence of metastases—imaging of chest, abdomen and bone is recommended. 18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET)/computed tomography (CT) scanning may be useful when conventional methods are inconclusive, and may replace traditional imaging for staging in high-risk patients3.
At a general level, clinicopathological parameters can fail to characterise the biological heterogeneity of tumours, which has important implications for treatment benefit. Traditional clinicopathological-based adjuvant chemotherapy (ChT) may not permit accurate individualised treatment. ChT overexposure is possible in low-risk groups, or in those who are already cured, and it can limit optimal treatment planning for groups at high risk of recurrence7.
Patients with low-risk HR+/HER2- breast cancers can be spared the toxicities of cytotoxic chemotherapies without compromising cancer prognosis7,9,11.
Most recurrences after 5 years of endocrine therapy are not preventable by extending treatment beyond the initial 5 years. Ongoing adjuvant trials for the cyclin-dependent kinases 4 and 6 (CDK4/6) inhibitors may improve outcomes7
Several gene expression profiles are available to complement the limitations of clinicopathological factors in BC risk assessment. Used together, they are more accurately predictive of BC risk and benefit of adjuvant ChT3.
Risk assessment of breast cancer: molecular factors
Gene-based assays deploy gene-expression profiling in determining the molecular subtype of the cancer, including traditional molecular biomarkers, such as ER, PR or HER2. Traditional biomarkers are described in more detail in the breast cancer stratification section.
Genetic assays supplement the traditional histopathological markers in BC risk assessment and can help identify patients at high risk of recurrence. They also provide a more quantitative approach to risk assessment and facilitate individualisation of treatment.
Such advantages can benefit quality of life and healthcare costs, because patients who will not benefit from a certain treatment can be spared both the toxicity and the expense.
Gene-based assays include MammaPrint®, Oncotype DX Recurrence Score®, Prosigna®, EndoPredict® and Breast Cancer Index® (BCI)3. Apart from MammaPrint®, these assays were designed for patients with ER+ BC only3.
Mostly, the genes assessed in these assays are involved in the regulation of the cell cycle and ER responses.
The Oncotype DX Recurrence Score® is a molecular tool that uses reverse transcription polymerase chain reaction (RT-PCR) assays, and incorporates 21 genes (including six housekeeping genes) related to proliferation, survival, invasion and oestrogen signaling. Expression levels of these genes equal a low, intermediate or high recurrence score (RS), thereby evaluating the likelihood of distant metastasis within the subsequent 10 years. It has shown prognostic value for the risk of recurrence 0–10 years after diagnosis, and may enable the prediction of benefit from adjuvant chemotherapy3,7.
The clinical utility of MammaPrint® and Oncotype DX® has been, or is still being prospectively evaluated, in large randomised clinical trials such as MINDACT for MammaPrint®, West German Study Group (WSG) PLAN B trial, TAILORx and RxPONDER (SWOG 1007) for Oncotype DX®38–40.
A level of evidence (LoE) and grade of recommendation (GoR) of [I, A] (Table 2) have been achieved through the MINDACT trial for the prognostic value and clinical utility (for ChT decision making) of MammaPrint (for clinical high risk, low genomic score), and for Oncotype DX® through the TAILORx and PLAN B trials3. MammaPrint® and Oncotype DX® are able to identify patients with an ultra-low risk of death from BC at 10 or 20 years41,42.
At the European Society for Medical Oncology congress in 2021, results from a single centre retrospective cohort study were revealed, showing that patients with low risk Oncotype DX scores® who had high Ki67 tumours have a greater risk of relapse. Therefore, Ki67 status may be a helpful indicator of low risk Oncotype DX®-scoring patients in which adjuvant chemotherapy may be of benefit43.
Table 2. Levels of evidence and grades of recommendation (Adapted44).
| Levels of evidence | Grades of recommendation |
| I: Evidence from at least one large randomised, controlled trial of good methodological quality (low potential for bias) or meta-analyses of well-conducted randomised trials without heterogeneity. II: Small randomised trials or large randomised trials with a suspicion of bias (lower methodological quality) or meta-analyses of such trials or of trials with demonstrated heterogeneity. III: Prospective cohort studies. IV: Retrospective cohort studies or case–control studies; V: Studies without control group, case reports, expert opinions |
A: Strong evidence for efficacy with a substantial clinical benefit, strongly recommended. B: Strong or moderate evidence for efficacy but with a limited clinical benefit, generally recommended. C: Insufficient evidence for efficacy or benefit does not outweigh the risk or the disadvantages (adverse events, costs, etc.), optional. D: Moderate evidence against efficacy or for adverse outcome, generally not recommended. E: Strong evidence against efficacy or for adverse outcome, never recommended. |
The PAM50 score combines the expression levels of 50 genes and tumour size, which are used to define the intrinsic subtypes of BC, and information from a set of proliferation-related genes for prognostic purposes. PAM50 has prognostic value for the prediction of recurrence risk between year 0 and year 10, with similar performance for the prediction of risk at years 0–5 and 5–103,7.
EndoPredict® is a 12-gene expression panel that is combined with clinical parameters to generate an EPClin score. EPClin has good prognostic value for the prediction of BC recurrence 0–10 years after diagnosis and of late recurrence in a combined cohort from the ABCSG 6 and ABCSG 8 studies3,7.
A score of [I, B] (Table 2) according to biomarker LoE guidelines has been achieved from retrospective analyses of data from prospective trials regarding the prognostic value of Prosigna® and Endopredict®, in ER+ BC45,46. In addition, the prognostic value of MammaPrint® has been validated in the RASTER trial, a prospective but non-randomised, clinical trial47.
The Breast Cancer Index® (BCI) is a molecular score that incorporates the ratio of HOXB13:IL17BR levels and a proliferation-related five-gene module referred to as Molecular Grade Index3,7. In the Stockholm TAM data set, a heterogeneous cohort (in terms of BC risk) of 1,374 postmenopausal women treated with tamoxifen, BCI had prognostic value for recurrence beyond 5 years48. In the TransATAC study, BCI had prognostic value for late recurrence in women with no lymph node involvement3,7.
The OPTIMA Prelim Trial has recently shown that the use of molecular tests has an 86% probability of being cost-effective49.
Clinical validity has been shown for PAM50 and BCI, but clinical utility and the predictive benefit of extended ET have not yet been established3,7.
Risk assessment modelling
Predictive models have been validated to assess BC risk in populations and individuals. Individualised risk assessment is an essential part in the effective assessment of women at high risk of BC35,50.
Identifying women at high-risk before breast cancer develops enables this group to consider more frequent screening with mammography and breast magnetic resonance imaging, genetic testing, and chemoprevention
Assessing the risk of carrying a germline mutation
Germline mutations associated with familial BC have been identified in other genes, including TP53, PTEN, ATM, CHEK2, NBS1, RAD50, BRIP, and PALB2, and others are suspected3,8,35.
Several predictive models and scoring systems have been designed to assess the presence of a BRCA1 mutation or a BRCA2 mutation in a given individual based on family history35,50. These models are empirical models and the genetic risk prediction models35,50.
Empirical models estimate the probability that genetic testing will detect a BRCA1 or BRCA2 mutation. They do not make assumptions about the underlying genetic risks such as penetrance, mutation frequencies, and method of inheritance35,50.
Empirical models include the Couch model, Myriad II, and the Australian LAMBDA model.
Genetic risk prediction models make direct assumptions about the number of susceptibility genes involved, the allele frequencies in the general population, and the cancer risks that are conferred by these alleles. These models use pedigree analysis methods, which are based on information about the exact relationships among individuals within a family35,50.
The advantage of genetic risk prediction models is that they can compute cancer risks and mutation carrier probabilities regardless of the family structure and disease pattern. However, their accuracy depends on the accuracy of their underlying assumptions35,50.
Examples include BRCAPRO, the Yale University model, and the International Breast Cancer Intervention Study (IBIS) model.
Comparison of germline mutation risk prediction models
In one UK study, data from six genetics clinics were used to compare the most commonly used models in the UK: Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA), BRCAPRO, IBIS, the Myriad II, and the Manchester model51. Only BOADICEA accurately predicted the overall observed number of mutations that were detected51. BOADICEA also provided the best discrimination between mutation carriers and noncarriers, and was statistically significantly better than all of the other models, except BRCAPRO (area under the receiver operating characteristic curve [AUC]: BOADICEA = 0.77; BRCAPRO = 0.76; IBIS = 0.74; Manchester = 0.75; Myriad II = 0.72)51. An AUC of 0.5 identifies a model whose discriminatory accuracy is no better than random chance. An AUC of 1.0 identifies a model with perfect discriminatory accuracy. Realistically, an AUC of 0.7 or 0.8 is consistent with good discrimination.
Incorporation of risk factors into risk assessment models
Current EBC risk prediction models are based on combinations of risk factors. In general, their outputs include a BC risk estimate over a specific time and/or over the lifetime of the patient.
Several predictive models have been designed for this purpose (Table 3).
Table 3. Known risk factors and their incorporation into current risk models (Adapted35).
Gail model
The most widely used model for EBC risk assessment is the Gail model52–55, which has been validated in three large population-based database studies52–54. However, a systematic review reported that, although eight studies comprising almost 13,000 patients had shown that the Gail model is well calibrated, it has limited discriminatory accuracy56. This limitation could explain the poor individualised risk assessment of the Gail model when tested in higher risk populations35.
Claus model
The Claus model, developed using data from the Cancer and Steroid Hormone Study, uses family history to estimate risk in EBC. It incorporates a more comprehensive history than the Gail model and includes affected first- and second-degree relatives and the age at which cancers in those relatives were diagnosed. However, the Claus model has never been validated in an independent dataset35. A further limitation of the Claus model is that it does not include any nonhereditary risk factors, such as hormonal or reproductive factors35.
BRCAPRO model
In addition to assessing the likelihood of carrying a BRCA gene mutation, the computerised BRCAPRO model includes an extension software package that calculates overall BC risk. An advantage of this model is that it includes information on both affected and unaffected relatives. However, no nonhereditary risk factors have been included. This model may therefore underestimate BC risk in women who have nonhereditary risk factors35.
Jonker model
Jonker et al.57 published a genetic model to predict BC risk based on the family history of breast and ovarian cancers. In this model, familial clustering of breast and ovarian cancers is explained by three genes: BRCA1, BRCA2 and a hypothetical third gene called BRCAu. The hypothetical gene was modelled to explain familial clustering of BC that was not accounted for by the BRCA1 and BRCA2 genes. The original Jonker model does not include data on personal risk factors for BC.
The original Jonker model developed into the validated Claus extended model58. This model includes estimates of the risk of bilateral BC, and of having three or more affected relatives. A limitation of the extended model is its inability to estimate risk in women with complex family histories and its validation in individual families rather than in an independent series59.
IBIS model
The IBIS model60 attempts to integrate family history, proxy measures of endogenous oestrogen exposure, and benign breast disease. Unlike the Claus and BRCAPRO models, the IBIS model allows for the presence of multiple genes of differing penetrance. Like the Jonker model, IBIS’s algorithm includes the likelihood of BRCA1 and BRCA2 mutations while allowing for a lower penetrance of BRCAu.
Practical limitations of risk models
Adoption, small family size, and lack of information about family history reduce the usefulness of all predictive risk models for EBC. Given the reluctance of people to discuss their medical conditions, particularly those involving BC, generations of family medical history may be lost to present-day patients who are receiving care in the era of genetic testing35.
The foremost limitation of early breast cancer risk models is their reliance on known risk factors, despite data that show that up to 60% of breast cancers can arise in the absence of any known risk factors35
Another limitation is that current risk models include information only about first- or second-degree relatives of the person who is being assessed. This may underestimate BC risk if there are many third-degree or higher relatives with BC35.
Risk models for BC can be improved by incorporating population-specific risks, mutation prevalence, or tumour-specific characteristics. For example, BRCA1 mutations are associated with triple-negative grade 3 BC histology. The presence of this phenotype could allow for an increase in the estimated risk of carrying a BRCA1 mutation35.
While numerous risk models are available in the BC setting, they have not been widely implemented to guide screening decisions in routine clinical decision-making. This is partly due to lack of clarity on which risk model to use, limited accuracy of risk models, and the time needed to perform risk assessment and interpret results61.
Future developments in breast cancer risk assessment
Advances in breast imaging that focus on reproducible measures of breast density may permit mammographic density to be included in future risk assessment modeling35,62.
Genome-based research may add valuable data to BC risk prediction methods. One common variant in the CASP8 gene with a minor allele frequency greater than 5% is associated with BC risk63. As a result, investigation of a range of high-risk genes and single-nucleotide polymorphisms (SNPs) in several genes that are associated with low risk of BC have been conducted to add knowledge of cancer genetics29,64,65. However, because of the variable presence of some SNPs in the general population, large datasets are needed to identify, at genome-wide statistical significance levels, loci with small per-allele effect sizes35.
While BOADICEA and IBIS show similar performance in assessing for BC risk, improvements in the accuracy of predictions are possible with hybrid models that incorporate the polygenic risk component of BOADICEA and the non-family-history risk factors included in IBIS66.
Models that incorporate additional genetic and nongenetic risk factors and estimate risk of tumour subtypes may further improve BC risk prediction61.
Review
- Women at high-risk of breast cancer are those with strong family history of breast, ovarian or pancreatic cancer, diagnosis of breast cancer before the age of 50, diagnosis of triple-negative breast cancer before the age of 60, and personal history of ovarian cancer or second breast cancer4,8,35
- It is critical that accurate and individualised risk assessment is conducted by the patient’s multidisciplinary team to select women most likely to benefit from prevention strategies or treatment4
- Gene-expression profiles, such as MammaPrint®, Oncotype DX Recurrence Score®, Prosigna®, Endopredict® and Breast Cancer Index®, can complement clinicopathological assessment of breast cancer risk and recurrence4
- To date, no risk assessment model can perfectly discriminate between families that do and do not have mutations, or between women who will and will not develop breast cancer35
Risk stratification tools using clinicopathological features of the patient’s disease and its molecular profile are used to prevent overtreatment of low-risk patients and to plan early treatment or prevention strategies for those at high risk of cancer recurrence
Breast cancer stratification
Breast cancer (BC) can be stratified into different entities on the basis of clinical behaviour, histological features, and/or by biological properties. As current anticancer agents target biological mechanisms, detailed molecular stratification is a requirement for clinical management of breast BC3,4.
Assays for risk stratification focus on prediction of the response to existing treatment regimens. Gene-expression profiling shows that BCs can be stratified in so-called intrinsic subtypes (luminal A, luminal B, human epidermal growth factor receptor 2 [HER2]-enriched, basal-like and normal-like), which mostly corresponds to hormone receptor (HR) and HER2 status, and further stratifies luminal tumours on the basis of proliferation12–14.
Stratification is critical for selecting patients with BC who could benefit from adjuvant therapy3,4,7. This is especially important for patients with early breast cancer (EBC), who comprise the majority of patients, because of widespread uptake of screening mammography3,4,7.
Stratification could also be important for selecting patients for clinical trials. It could facilitate the discovery of novel drivers, the study of tumour evolution, and the identification of mechanisms of treatment resistance.
While only 6–10% of the women are diagnosed with de novo metastatic breast cancer (mBC), most women with mBC have been previously diagnosed with locally advanced disease and subsequently have cancer recurrence in the form of metastasis6. Approximately 30% of these patients will develop incurable cancer recurrence6–8.
Risk of cancer recurrence is high in patients with hormone receptor-positive (HR+) and oestrogen receptor-positive (ER+) BC. Relapse of BC may occur as late as >20 years after the initial diagnosis, particularly in patients with ER/progesterone receptor-positive (PR+) BC3.
The higher the risk of cancer recurrence, the more aggressive the therapy. Thus, stratification can prevent chemotherapeutic overtreatment in some patients at low risk of recurrence, or in those who are cured, and it can enable planning suitable treatments or prevention strategies in those at high risk of recurrence3,7.
A clinical decision-making tool has been proposed for the combined use of clinical and genomic tests for risk stratification of patients upon completion of 5 years of endocrine therapy (ET) without distant recurrence (Figure 7)7.
Figure 7. Decision-making aid for clinical and genomic testing (Adapted from Richman & Dowsett et al.7). BCI, Breast Cancer Index; CTS5, Clinical Treatment Score at 5 Years; PAM50, Prediction Analysis of Microarray 50; EPClin, EndoPredict®.
In Figure 7, the clinical treatment score at 5 years (CTS5) is calculated for all women upon completion of 5 years of adjuvant ET. For most women with a low CTS5 score, ET can be discontinued because extended therapy is unlikely to benefit them. For most women with a high risk of recurrence, extended ET up to 10 years is recommended if the toxicity profile is favourable. In both situations, genomic testing is unlikely to add further prognostic information and is not recommended. Women with an intermediate clinical risk and those at borderline low-intermediate or high-intermediate clinical risk should receive a genomic test to enable integrated clinical-genomic stratification of their risk of late recurrence. Following genomic testing, the following scenarios are possible: discontinuation of ET for patients with a low risk of recurrence or recommendation of extended ET for up to 10 years in patients with a high risk. Women who remain at an intermediate level of risk should discuss toxicities and personal preferences with their clinician.
Role of hormone receptors and biomarkers in breast cancer stratification
Oestrogen receptor
ER is arguably the most important prognostic biomarker in BC, because of the development of targeted therapy with tamoxifen or aromatase inhibitors.
The application of 5 years of adjuvant tamoxifen-based therapy in ER+ BC showed a 29% reduction of the risk for death from the disease36,67,68. In approximately 30–40% of patients with advanced ER+ BC, response to the treatment is likely to be positive. In approximately 20% of patients, stable disease could be achieved. Hormone therapy is generally free of toxicity, permitting long-lasting use69.
Progesterone receptor
In EBC, PR expression is associated with tumour grade, ER expression, Nottingham prognostic group and HER2- status70. Evidence shows a better prognosis in PR+ cancers70. The evaluation of PR expression does not appear to have a role in the ET choice in both locally advanced and mBC71.
PR is expressed in 60–70% of invasive ductal carcinomas. The correlation between ER and PR expression is high, but 10% of ER+ cancer can be PR-. In these patients, the risk of recurrence and mortality compared to ER+/PR+ cancer are higher69.
High expression of PR protein is more frequently observed in tumours with a better baseline prognosis (luminal A) than in tumours with a poor baseline prognosis (luminal B).
Ki-67
No significant relationship between proliferation index (Ki-67) and prognostic factors such as hormone receptors and HER2 has been found69. Furthermore, no significant correlation was observed between Ki-67 and disease-free survival (DFS) at 3 and 5 years or with overall survival (OS) at 5 years73. Therefore, the role of Ki-67 in patient stratification is limited.
Although Ki-67 may be used to discriminate higher risk groups in the context of ER+/PR+ BC, no consensus has been agreed on the cut-off69.
HER2
HER2+ is more frequently found in ER- tumours than in ER+ tumours. Only 12 % of ER+ BCs are positive for HER2 by amplification/overexpression of the gene74.
Tumours with HER2 amplification are associated with a less favourable prognosis when compared with tumours having similar morphological features, but lacking amplification of the gene or the overexpression of the protein69.
Although HER2 was originally proposed as a prognostic biomarker for BC, currently its usefulness lies in predicting response to anti-HER2 therapy in neoadjuvant and adjuvant settings69.
Amplification/overexpression of HER2 is a necessary condition for the administration of anti-HER2 therapies. Of the anti-HER2 treatments available, trastuzumab is the most studied.
HER2-low
Almost half of the currently defined HER2-negative BCs show some degree of HER2 immunohistochemistry (IHC) expression and have been recently renamed as HER2-low BC75. This is a recent designation defined as tumours with IHC staining of 1+, or 2+ without HER2 gene amplification76. These tumours are targets for antibody–drug conjugates (ADCs), one of which, trastuzumab deruxtecan (T-DXd), was approved by the FDA in August 2022 and the EMA in January 2023 for treatment of metastatic BC in patients with HER2-low cancers who have received one or two chemotherapies or developed recurrent disease during or within 6 months of completing chemotherapy77. This was based on results from the DESTINY-Breast04 clinical trial, where treatment with T-DXd resulted in significantly longer progression-free and overall survival than the physician’s choice of chemotherapy77,78.
Although hormone receptors and HER2 overexpression currently represent the main protagonists of targeted therapy for BC, chemotherapy (ChT) remains the standard of care for tumours lacking ER, PR and HER2 expression. Consequently, much effort in BC research involves study of targetable molecules with predictive purposes in triple negative tumours69.
Triple-negative breast cancer
A meta-analysis of triple-negative cancer (TNBC) defined seven clusters with different molecular profiling79:
- Basal-like 1 (BL1), basal-like 2 (BL2)
- Immunomodulatory (IM)
- Mesenchymal (M)
- Mesenchymal stem-like (MSL)
- Luminal androgen receptor (LAR)
- Unstable cluster (UNS)
BL1 tumours are characterised by genetic alteration of genes involved in cell-cycle regulation, including the higher rate of mutations of TP53, amplifications of MYC, CDK6 and CCNE1, and deletions of BRCA2, PTEN, MDM2 and RB180.
BL2 tumors are characterised by genetic alterations involving growth factor signaling pathways and metabolic pathway activity, including EGF, NGF, MET, Wnt/β-catenin and IGF1R81.
As a group, basal-like tumours can have high proliferative activity, as shown by high Ki-67 mRNA expression or nuclear Ki-67 immunohistochemical staining, high metabolic activity, and genetic instability72. Most BRCA-mutated BCs are part of the basal-like groups82.
IM tumors are characterised by mutation of genes involved in antigen processing and cytokine signaling, such as JAK/STAT, TNF and NFkB. The prevalent expression of genes related to cell motility and epithelial mesenchymal transition are the genetic clues of mesenchymal-like subtypes, including M and MSL subtypes83.
LAR subtype is characterised by the high expression of Androgen receptor (AR) with frequent mutations involving genes like PIK3CA, KMT2C, CDH1, NF1 and AKT180.
Emerging biomarkers
Programmed cell death receptor ligand 1 (PD-L1) is considered the most relevant predictive biomarkers of response to anti-PD1/PD-L1 immune checkpoint inhibitors. High levels of PD-L1 expression have been found in several types of cancers, and are generally associated with a poor prognosis. PD-L1 is overexpressed in a subset of basal-like and TNBCs, and its expression mainly occurs on tumour-infiltrating immune cells than on tumour cells84.
Vascular endothelial growth factor (VEGF) seems to be the most important angiogenetic factor in BC, promoting growth of blood vessels that support the neoplasm and metastatic dissemination. High levels of VEGF have been correlated to poor prognosis and TP53 mutation in BC. Consequently, immunohistochemical evaluation of VEGF expression may have a prognostic role in the near future69.
Microsatellite instability (MSI) is a phenotype defined by defects in mismatch repair proteins MLH1, PMS2, MSH2 and MSH6, leading to replication errors in segments of DNA characterised by short nucleotide repeat motifs known as microsatellites. MSI is an opportunity to select patients who may benefit from immune checkpoint inhibitors, especially among TNBC85.
AXL, deriving from the Greek “anexelekto”, meaning “uncontrolled”, is a gene located in the q13.2 locus of chromosome 19, and encodes a membrane-located receptor with tyrosine kinase activity, belonging to the TAM receptors family. AXL deregulation has been shown in several neoplasms, including breast carcinoma; therefore, it is a potential target for targeted therapy69.
ADAPTlate
ADAPTlate is a prospective, multicentre, interventional, two-arm, open, randomised, controlled adjuvant phase 3 trial, to investigate the additional benefit from 2 years of the CDK4/6 inhibitor abemaciclib combined with ET, compared with ET alone, in patients with high-risk HR+/HER2- EBC86.
The study seeks to improve adjuvant therapy for patients at high risk for late-disease recurrence who completed definite locoregional therapy, with or without (neo)adjuvant ChT, and are under adjuvant ET. This high-risk population does not benefit as much from standard ET and can go on to develop secondary ET resistance and late recurrences86.
Translational research aims to evaluate the potential mechanisms of resistance to ET and/or CDK4/6 targeted therapy. Exploratory tissue biomarker research will assess alterations in molecular markers and liquid biopsies, such as circulating tumour cells (CTC), circulating tumour DNA (ctDNA), and circulating tumour RNA (ctRNA), to study mutations and gene expression relevant for HR+/HER2- EBC86.
Recruitment is ongoing as of 2021. Eligible patients will be pre-/post- menopausal patients with histologically confirmed invasive HR+/HER2- EBC, 2–6 years after primary diagnosis, with either86:
- a known high clinical risk (clinical node staging / pathological assessment of the regional lymph nodes [c/pN] 2–3 or high clinical treatment score (CTS) score in pN 0–1 or non-pathological complete response (pCR) after neoadjuvant CT in cN 1 or G3 tumours or G3 and Ki-67 ≥40% in pN 0–1)
- a known high genomic risk (RS >25 in c/pN 0, RS >18 in c/pN 1 or high-risk Prosigna, EPclin, or Mammaprint in pN 0–1)
- an intermediate clinical, but unknown, genomic risk (luminal B-like (G3 or Ki-67 ≥40%) in c/pN 0–1 and either RS >25 in c/pN 0, or RS >18 in c/p N1 in screening)
The duration of treatment will be two years for abemaciclib + ET (premenopausal: aromatase inhibitor [AI] + gonadotropin-releasing hormone [GnRH]) followed by 3–6 years ET alone. Patients in control arm will receive 5–8 years of ET at the investigator’s choice86.
Review
- Knowledge of the molecular mechanisms underlying BC has led to the identification of different biomarkers12–14
- Based on their prognostic value, traditional biomarkers associated with BC, such as oestrogen receptor (ER), progesterone receptors (PR), or HER2, enable clinicians to stratify patients who could be eligible for adjuvant therapy, or at low or high-risk of cancer recurrence3,4,12–14
- Several emerging biomarkers may further improve prognostic stratification69,84,85
Further investigation is needed to determine if patients are stratified into clinically meaningful groups, and whether the resulting treatment changes ultimately improve clinical outcomes
Breast cancer treatment landscape
Treatment of breast cancer (BC) in specialised breast units or centres, defined as specialised institutions or departments that care for a high volume of BC patients, improves disease-free survival (DFS) and overall survival (OS), daily functioning, and quality of life (QoL)3,4.
Treatment in these units/centres is provided by a multidisciplinary team (MDT) specialised in BC. MDTs provide “consistent, continuous, co-ordinated, and cost-effective care to the patient,”87 and there is evidence to suggest that decisions made by an MDT are more likely to align with evidence-based guidelines89–91. Introduction of multidisciplinary care has been shown to significantly improve outcomes such as mortality92.
BC MDTs consist of medical oncologists, breast surgeons, radiation oncologists, breast radiologists, breast pathologists and breast nurses. A breast nurse, or a similarly trained and specialised health care practitioner, usually acts as a “patient navigator.” Patients ought to be actively involved in all management decisions3,4.
- Treatment options for early breast cancer
- CDK4/6 inhibitors: an adjuvant treatment option?
- Review
- Treatment options for advanced breast cancer
- Hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer
- CDK4/6 inhibitors as a treatment option in advanced breast cancer
- Triple-negative breast cancer (TNBC)
- Review
Treatment options for early breast cancer
Treatment of EBC is complex and involves multiple options. These include local modalities (surgery, radiotherapy (RT)], systemic anticancer treatments (chemotherapy [ChT], endocrine therapy [ET], molecularly targeted therapies) and supportive measures, delivered in diverse sequences3.
Prognostic and predictive biomarkers such as oestrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), Ki-67, and approved genomic signatures can help determine suitable treatments (Figure 8)3.
Figure 8. Early breast cancer treatment algorithm (Adapted4). BCS, breast-conserving surgery; ChT, chemotherapy; ET, endocrine therapy; HER2, human epidermal growth factor receptor 2; RT, radiotherapy; TNBC, triple-negative breast cancer. To view levels of evidence and grades of recommendation, see Table 2.
Surgery
Table 4 provides an overview of current local surgical treatments for EBC3.
Table 4. An overview of current local surgical treatments for early breast cancer (Adapted3).
| Local treatment | Recommendation |
| Breast-conserving surgery (BCS) | · BCS is the preferred local treatment for many patients with EBC, with the use of oncoplastic techniques, to maintain good cosmetic outcomes in certain patients, when needed. |
| Mastectomy | · Besides simple mastectomy and skin-sparing mastectomy (SSM) that preserves the skin envelope, nipple-sparing mastectomy (NSM) has been increasingly used in the last decade · Breast reconstruction should be available and proposed to all women requiring mastectomy |
| Risk-reducing mastectomy | · Risk-reducing surgery (with prophylactic bilateral mastectomy and reconstruction) may be offered to women at very high risk, such as BRCA1 or BRCA2 mutation carriers. or those who have had previous chest RT at young age |
| Sentinel lymph node biopsy (SLNB) | · SLNB, rather than full nodal clearance, is the standard-of-care for axillary staging in early, clinically node-negative BC |
| Radiotherapy (RT) | · Postoperative RT is recommended after BCS · Boost RT is advised to reduce the risk of in-breast relapse in patients at higher risk of local recurrence |
| Accelerated partial-breast RT after BCS (APBI) | · APBI is an acceptable treatment in patients at low risk for local recurrence |
| Post-mastectomy RT (PMRT) | · PMRT is recommended for high-risk patients |
Adjuvant systemic treatment
The decision on adjuvant/neoadjuvant systemic treatment is based on the predicted patient sensitivity to particular treatment types, the benefit from their use, and the patient’s risk of relapse (Figure 9)4. Relapse relies on the patient’s tumour burden and tumour biology.
Figure 9. Adjuvant systemic treatment choices for early breast cancer by marker expression and intrinsic phenotype (Adapted4). ChT, chemotherapy; ER, oestrogen receptor; ET, endocrine therapy; HER2, human epidermal growth factor receptor2; N0, node-negative; PR, progesterone receptor; TNBC, triple-negative breast cancer. To view levels of evidence and grades of recommendation, see Table 2.
The decision on adjuvant systemic treatment also incorporates the predicted short- and long-term toxicities of treatment, the patient’s age, general health status, comorbidities and preferences4.
Decision-making tools such as PREDICT Plus®, NPI® and Adjuvant! Online® can help predict recurrence risk and potential benefit from systemic treatments (Table 5)4
Table 5. Summary of biomarkers for treatment decision making (Adapted4).
ChT, chemotherapy; ER, oestrogen receptor; ET, endocrine therapy; GoR, grade of recommendation; HER2, human epidermal growth factor receptor 2; IHC, immunohistochemistry; ISH, in situ hybridisation; LoE, level of evidence; PR, progesterone receptor; RT-PCR, reverse transcription polymerase chain reaction. To view levels of evidence and grades of recommendation, see Table 2.
Genomic tests are not recommended for patients with clinicopathological low-risk tumours (pT1a, pT1b, G1, ER high, pN0) or patients with comorbid health conditions who are not candidates for adjuvant ChT3.
Premenopausal and postmenopausal women
For premenopausal women, tamoxifen for 5–10 years is a standard of care. For postmenopausal women, aromatase inhibitors (AIs) and tamoxifen are considered standard treatments3.
Chemotherapy
Chemotherapy (ChT) is advised for most patients with most triple-negative, HER2+ BC and those with high-risk luminal-like HER2- tumours. Sequential anthracycline/taxane-based regimen is the standard for most patients with EBC. In some lower risk patients, 4 cycles of anthracycline- or taxane-based ChT or cyclophosphamide/methotrexate/5-fluorouracil (CMF) may be used3.
Taxanes can improve the efficacy of ChT, independently of age, nodal status, tumour size or grade, steroid receptor expression or tamoxifen use. Taxanes allow for the use of a lower total dose of anthracyclines through the use of sequential regimens3.
Anti-HER2 therapy
Trastuzumab combined with ChT in patients with HER2 overexpression/amplification roughly halves recurrence and mortality risk, compared with ChT alone, signifying a 10% improvement in long-term DFS and 9% increase in 10-year OS. One year of adjuvant trastuzumab remains a standard for the vast majority of HER2+ EBC (Figure 10).
Figure 10. HER2-positive breast cancer treatment (Adapted4).
ChT, chemotherapy; EMA, European Medicines Agency; ER, oestrogen receptor; ESMO-MCBS, ESMO-Magnitude of Clinical Benefit Scale; HER2, human epidermal growth factor receptor 2; N-positive, node-positive; pCR, pathological complete response; T-DM1, trastuzumab emtansine. To view levels of evidence and grades of recommendation, see Table 2.
Personalised medicine
ER, PR and HER2 status are routinely used as prognostic/predictive factors to select patients for targeted ET or anti-HER2 treatment3.
More recently, surrogate intrinsic tumour phenotypes, based on biomarker expression, have been used for personalised treatment. Urokinase plasminogen activator-plasminogen activator inhibitor 1 (uPA-PAI1), a biomarker of tumour invasiveness, has been validated in prospective clinical trials as a prognostic marker for both node-negative and node-positive BC and can be used in treatment decision-making for EBC93.
Molecular signatures for ER+ BC such as MammaPrint®, Oncotype DX®, EndoPredict®, Prosigna® and Breast Cancer Index® may help with adjuvant ChT decision making, together with clinicopathological features, in challenging cases of BC, such as luminal B-like/HER2- or node-negative/nodes 1–3+ BC3.
PARP inhibitors in early breast cancer
The OlympiA study was the first randomised, double-blind, phase 3 study, to investigate the use of the poly (ADP-ribose) polymerase (PARP) inhibitor olaparib as adjuvant therapy following adjuvant or neoadjuvant ChT in patients with gBRCA mutations and HER2− (TNBC or HR+) high-risk EBC94. Results from the OlympiA study showed that adjuvant treatment with olaparib, after completion of neoadjuvant or adjuvant ChT, significantly improved invasive disease-free survival (iDFS) and distant disease-free survival (DDFS)94. Notably, these results have now been incorporated into the June 2021 American Society of Clinical Oncology (ASCO) rapid guidelines recommendation update. Specifically, guidelines now recommend offering 1 year of adjuvant olaparib to patients with high-risk early-stage HER2− BC and germline BRCA mutations after completion of (neo)adjuvant chemotherapy and local treatment95.
In March 2022, olaparib received FDA approval for adjuvant treatment of adult patients with deleterious or suspected deleterious germline BRCA-mutated (gBRCAm) HER2−, high-risk EBC after treatment with neoadjuvant or adjuvant chemotherapy. The approval stipulates that patients must be selected for therapy using an FDA-approved companion diagnostic for olaparib96.
CDK4/6 inhibitors in early breast cancer
Following the success of cyclin-dependent kinases 4 and 6 inhibitors (CDK4/6 inhibitors) in the advanced breast cancer (ABC) setting for HR+/HER2- BC, and evidence in EBC from the phase 2 NeoPalAna trial (palbociclib plus anastrozole), several phase 2/3 clinical trials have assessed CDK4/6 inhibitor efficacy in combination with ET in the adjuvant setting97,98. These trials include monarchE for abemaciclib99, PALLAS and PENELOPE B for palbociclib100,101, and NATALEE and Ear-LEE-1 for ribociclib102-103.
The monarchE trial showed that adding abemaciclib to standard-of-care adjuvant ET, including ovarian function suppression for premenopausal women, reduced the risk of cancer recurrence99. This was the first clinical trial to establish a role for CDK4/6 inhibition in the adjuvant treatment of EBC.
The outcome of the monarchE trial led to approval by the US Food and Drug Administration and the European Medicines Agency for the use of abemaciclib in combination with ET as adjuvant treatment of adult patients with HR+/HER2−, node-positive, early breast cancer (EBC) at high risk of recurrence104,105
Learn more about clinical trials for CDK4/6 inhibitors in early and advanced breast cancer
Neither the PALLAS study nor the PENELOPE B trial demonstrated a statistically significant improvement in iDFS with palbociclib + ET, compared with ET alone, therefore failing to meet their primary endpoints100,106,107. By contrast, at a pre-planned interim analysis in March 2023, it was announced that the NATALEE trial had met its primary endpoint, achieving a statistically significant improvement in iDFS in people with HR+/HER2– EBC treated with ribociclib + ET when compared with ET alone108. Further results from the NATALEE clinical trial are expected to be released in late 2023.
Review
- Treatment of BC in specialised breast units or centres, provided by specialist multidisciplinary teams, improves patient breast cancer outcomes3,4
- The treatment landscape for early BC is complex and comprises local modalities, systemic anticancer and supportive measures3
- Prognostic and predictive biomarkers such as ER, PR, human epidermal growth factor receptor2, and Ki-67 and approved genomic signatures, can help determine suitable personalised therapies for targeted endocrine therapy or anti-human epidermal growth factor receptor2 treatments3
- Breast-conserving surgery is the preferred local treatment for many patients with early breast cancer3
- Oncoplastic techniques are used when needed, and breast reconstruction should be available and proposed to all women requiring mastectomy3
- Chemotherapy is recommended in most triple-negative, human epidermal growth factor receptor 2+ breast cancers, and in high-risk luminal-like human epidermal growth factor receptor 2- Sequential anthracycline/taxane-based regimen is standard-of-care for most patients with early breast cancer3,4
- The PARP inhibitor olaparib is approved for adjuvant treatment of deleterious or suspected deleterious germline BRCA-mutated (gBRCAm) HER2−, high-risk EBC after treatment with neoadjuvant or adjuvant chemotherapy
- The CDK4/6 inhibitor abemaciclib in combination with ET is now an option for adjuvant treatment of patients with HR+/HER2−, node-positive early breast cancer at high risk of recurrence
The final decision on adjuvant systemic treatment is based on the patient’s expected sensitivity to specific treatment types, treatment benefits and toxicities, and the patient’s risk of relapse (comprising the patient’s tumour burden and tumour biology), age, overall health status, comorbidities and personal preferences3
Treatment options for advanced breast cancer
Advanced breast cancer (ABC) comprises both inoperable locally advanced breast cancer (LABC) and metastatic breast cancer (mBC)4.
Treatment of ABC is complex. Involvement of all appropriate specialties in a multidisciplinary team (MDT), not restricted to medical, radiation and surgical oncologists, imaging experts, pathologists, gynaecologists, psycho-oncologists, social workers, nurses and palliative care specialists, is essential4.
Following a thorough assessment and confirmation of mBC, the potential treatment goals of care are discussed with the patient and family. Treatment should be personalised for the individual patient4.
mBC remains largely incurable; however, as survival is improving in some patients with ABC, consideration of survivorship issues is part of routine care. Sensitive healthcare professionals are ready to change and adapt treatment strategies to disease status, treatment of adverse effects and quality of life, patients’ priorities and life plans4.
With some patients achieving long-term relapse-free survival, discussion is now ongoing as to whether a subset of patients may be curable with a more aggressive MDT approach and curable intent109.
In the absence of a cure, the goal of treatment must be to extend life and delay disease progression, while ensuring that patients continue to have the best quality of life for as long as possible110.
Patient involvement in their care has been associated with positive patient outcomes111
Treatment choice for ABC should take at least these factors into consideration4:
- Hormone receptor (HR), human epidermal growth factor receptor 2 (HER2), and germline BRCA status
- Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) in hormone receptor-positive (HR+) and programmed death-ligand-1 (PD-L1) in triple-negative breast cancer (TNBC), if targeted therapies are accessible
- Previous therapies and their toxicities
- Disease-free interval (DFI)
- Tumour burden (defined as number and site of metastases)
- Age of the patient
- Performance status (PS)
- Comorbidities (including organ dysfunctions)
- Menopausal status (for ET)
- Need for rapid disease/symptom control
- Socio-economic and psychological factors
- Available therapies in the patient’s country
- Patient’s preference
Most cases of mBC are treated using systemic therapy, which includes endocrine therapy (ET), chemotherapy (ChT) and various targeted therapies, such as the oral cyclin dependent kinase 4/6 inhibitors (CDK4/6 inhibitors), abemaciclib, palbociclib and ribociclib3,112. These may be used as single agents or in combination with one another.
Current targets of systemic therapies include a range of key pathways, such as112:
- oestrogen receptor (ER) signalling
- HER2 signalling
- phosphoinositide 3-kinase (PI3K)/protein kinase B (AKT)/mammalian target of rapamycin (mTOR) signalling
HR and HER2 status of the cancer is a particularly important consideration when selecting a treatment strategy4.
Hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer
ET is considered a mainstay of HR+/HER2- mBC treatment, and is internationally recommended as a first-line systemic treatment for this disease subtype3,113. This is in preference to chemotherapy (ChT), which is usually reserved for those with rapidly progressing visceral disease3,114.
A range of differentETs is currently available for the treatment of HR+ mBC (Table 6). Ensuring that patients receive the treatment best suited to their individual needs requires careful consideration of the following factors3,114:
- Menopausal status
- Comorbidities
- Prior adjuvant therapy
- Drug availability
- Patient preference
- Drug safety profile
Table 6. Summary of endocrine therapies available to treat hormone receptor-positive metastatic breast cancer (Adapted84).
| ER, oestrogen receptor; NSAI, non-steroidal aromatase inhibitor; SAI, steroidal aromatase inhibitor. | ||
| Endocrine therapy | Patient group | Mode of action |
| Tamoxifen | Pre-/postmenopausal women | Binds to the ligand binding domain of ER, competing with oestrogen |
| Aromatase inhibitors · Exemestane (SAI) · Anastrozole, letrozole (NSAI) |
Mostly postmenopausal women | Inhibit aromatase, an enzyme involved in conversion of androgens to oestrogen |
| Goserelin | Premenopausal women | A luteinising hormone releasing hormone analogue that causes ovarian suppression |
| Fulvestrant | Mostly postmenopausal women | Binds to ER resulting in ER degradation and loss or ER protein expression |
| Cyclin dependent kinase 4/6 (CDK4/6) inhibitors | Pre-/postmenopausal women | Binds the ATPase pocket of CDK4 and CDK6, thereby inhibiting cell cycle progression |
Continuation of ET is an option following disease progression on first-line ET, provided the patient derived some benefit from their initial therapy, and unless they are experiencing symptoms of the underlying disease or the disease is progressing rapidly114.
Failure of three lines of ET usually necessitates the use of ChT, although continuation of ET may be considered reasonable if disease progression remains slow and the patient is asymptomatic113,114.
Premenopausal and postmenopausal women
In postmenopausal women, an aromatase inhibitor (AI) such as anastrozole or letrozole may be used as a form of endocrine monotherapy in the first line of treatment. Similarly, tamoxifen, a selective oestrogen receptor modulator (SERM), or fulvestrant, a selective oestrogen receptor degrader (SERD), may initially be used to treat this group of patients112.
In premenopausal women, treatment options mirror those available to postmenopausal women, but additional treatment with ovarian suppression drugs such as leuprolide or goserelin, or ovarian ablation are required in order to reduce oestrogen levels4,6. These patients may also be treated with a selective oestrogen receptor modulator (SERM)3,115.
CDK4/6 inhibitors as a treatment option in advanced breast cancer
Three oral CDK4/6 inhibitors, abemaciclib, palbociclib and ribociclib, are available for the treatment of HR+/HER2- mBC following the success of a series of trials investigating their safety and efficacy116. All three CDK4/6 inhibitors are indicated in patients with local ABC104,117,118.
The CDK4/6 inhibitors are now widely recommended for use in first-line treatment in combination with either an AI or fulvestrant. This recommendation applies to postmenopausal women, and to premenopausal women in combination with an luteinising hormone-releasing hormone (LHRH) agonist4.
Abemaciclib is also approved by the US Food and Drug Administration (FDA) as a monotherapy in HR+/HER2- mBC, in adults who progressed following ET and ChT. Regimens that include CDK4/6 inhibitors may also be used as second-line treatment in cases where they have not been used as first-line treatment and have shown promising results in the later line setting112,114.
It is not known if CDK4/6 inhibitors should be preferably administered in the first- or second-line ABC setting. However, the majority of panellists preferred giving a CDK4/6 inhibitor in the first-line setting for most patients4.
No data currently support the use of a combination of CDK4/6 inhibitor and ET as maintenance therapy following ChT. Maintenance therapy, in this case, is delivered with ET alone4.
Using artificial intelligence to predict CDK4/6 treatment response in advanced breast cancer
Although treatment with CDK4/6 inhibitors is supported by evidence in ER+/HER2− BC, side effects and financial considerations have contributed to limited administration. In addition, predictive biomarkers for CDK4/6-targeted therapies are currently lacking, despite ongoing research in the field119.
A retrospective analysis was recently conducted that examined CDK4/6 inhibitor response using a database of over 1,000 genomes from patients with BC (171 of whom were treated with palbociclib and ribociclib). The analysis incorporated genomics, molecular biology and machine learning algorithms. The results indicated that the genomic signature of CDK4/6 inhibitors, comprising nine biomarkers, improved the predictive stratification of patients with advanced ER+/HER2− BC. This is promising research that may help clinicians identify patients most likely to benefit from CDK4/6 inhibitor treatment119.
Endocrine resistance
Endocrine resistance is common among HR+ mBC patients receiving ET and results in disease progression120.
Dysregulation of the phosphatidylinositol-3-kinase (PI3K)/AKT/mammalian target of rapamycin (mTOR) pathway frequently occurs in BC, and hyperactivation of the PI3K pathway is associated with acquired resistance to endocrine therapy120,121. mTOR, which comprises two multi-protein complexes, is a downstream effector of the PI3K/AKT pathway122.
Everolimus restricts the growth of tumour cells via inhibition of mTOR complex 1 and is often given in combination with exemestane as second- or later-line treatment in postmenopausal patients who have developed resistance to non-steroidal AIs122.
In addition, a second molecule targeting a different part of the PI3K/AKT/mTOR pathway, alpelisib, was recently approved by the US Food and Drug Administration (FDA)3,123. This PI3Kα-specific inhibitor can be given in combination with fulvestrant to postmenopausal patients who have undergone unsuccessful treatment with an AI and have HR+/HER2-, PI3Kα mutated mBC3,124.
The HER2- status of these patients means that among those with a germline BRCA1/2 mutation, poly-ADP ribose polymerase (PARP) inhibitors may also prove an effective treatment option112.
A recent retrospective study evaluated the distribution and incidence of de novo PIK3CA mutations in HR+/HER2- metastatic breast cancer, enrolling patients on endocrine therapy being treated with CDK4/6 inhibitors, whose initial formalin-fixed paraffin-embedded tissue samples were available. Results indicate that a worse clinical outcome is associated with HR+/HER2- metastatic breast cancer patients who exhibit the presence of de novo PI3K mutation. This is despite the use of CDK4/6 inhibitors. This study concludes that clinicians should consider assessing the presence of de novo PIK3CA mutation, upfront125.
Hormone receptor-positive, human epidermal growth factor receptor 2-positive metastatic breast cancer
It has been estimated that overexpression or gene amplification of HER2 occurs in 20–30% of BC cases4,85. Of these, around half are also HR+4,126. Overexpression of HER2 promotes tumour cell proliferation and is associated with significantly shortened disease-free survival and overall survival in patients with BC4,127. HER2 signalling pathways, therefore, represent an important treatment target in patients with HER2+ cancers. The addition of multiple anti-HER2 targeted therapies to oncologists’ treatment arsenal has resulted in significant improvements to patient outcomes in this group, even in the advanced setting. However, despite the benefits of HER2-targeted therapies, de novo and acquired resistance to these therapies is very common4,128.
Currently available HER2-targeted therapies include trastuzumab, pertuzumab, lapatinib, ado-trastuzumab emtansine (T-DM1) and T-DXd. Standard first-line therapy in patients with HER2+ mBC is trastuzumab and pertuzumab taken in combination with a taxane3,114,129. This is generally followed by trastuzumab emtansine in the second line of treatment3,114,129. If the disease continues to progress, a new ChT or ET with continued HER2 blockade can be used, even if previous HER2-targeted therapy has failed to prevent disease progression4,6.
Hormone receptor-negative, human epidermal growth factor receptor 2-positive metastatic breast cancer
HR−/HER2+ mBC is the least common of the four subtypes130. Treatment options for patients with this type of breast cancer are very similar to those available to patients with the HR+/HER2+ subtype, starting with dual blockade or HER2 in combination with ChT. However, later-line therapy usually comprises a ChT, rather than ET, in combination with an HER2-targeted agent6.
Triple-negative breast cancer (TNBC)
Metastatic TNBC has the worst prognosis of the four BC subtypes, lacking the molecular targets of both endocrine and HER2-targeted therapies14,131. For this reason, chemotherapeutic approaches are widely recommended for the treatment of this group of patients. Monotherapy in the form of an anthracycline, a taxane, capecitabine or eribulin is common in both first- and later-line treatment4,6.
PARP inhibitors may also be used to treat patients with this disease subtype, provided they have a germline BRCA1/2 mutation4,94,131,132.
Sacituzumab govitecan is an ADC that targets Trop-2 for the selective delivery of SN-38, the active metabolite of irinotecan. It is approved by the EMA and FDA for the treatment of adult patients with unresectable locally advanced or metastatic TNBC who have received at least two prior therapies, at least one of them for advanced disease133,134.
The immune checkpoint inhibitor pembrolizumab is approved by the EMA and FDA for the treatment of high-risk early-stage TNBC as neoadjuvant therapy in combination with chemotherapy and as a single agent for adjuvant therapy. Pembrolizumab, in combination with chemotherapy, is also approved for treatment of locally recurrent unresectable or metastatic TNBC in adults whose tumours express programmed death ligand 1 (PD-L1) with a combined positive score (CPS) of ≥10 and who have not received prior chemotherapy for metastatic disease135,136.
Erβ is another potential treatment target for TNBC and a phase 2 trial for oestradiol is currently in progress24,137.
Review
- Treatment of ABC is complex, and involves all suitable specialties in a multidisciplinary team4
- Treatment should be personalised for each patient. As survival is improving in some patients, integrating survivorship issues into optimal care is essential4
- Treatment choice for ABC should consider a range of complex, interacting factors, including hormone receptor, human epidermal growth factor receptor 2 status, and germline BRCA status, phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha in hormone receptor-positive and programmed death-ligand-1 in TNBC, disease-free interval, comorbidities, and patient preferences4
- Most patients with mBC are treated with systemic therapy, comprising ET, ChT, or targeted therapies4,112
- Continuation of ET is an option following disease progression on first-line ET4,109
- In premenopausal women, treatment options are the same as those available to postmenopausal women, but further treatment with ovarian suppression drugs may be required in this group4,6,112
- Everolimus with exemestane as second- or later-line treatment in postmenopausal patients is recommended in patients who develop endocrine resistance3,122
- HER2 signalling pathways are an important treatment target in patients with HER2+ cancers3,126,128
- For TNBC, chemotherapeutic approaches are advised4,131,132
CDK4/6 inhibitor overview
Many breast cancers (BCs) are diagnosed at an early stage. These tumours are mostly hormone receptor-positive (HR+) and human epidermal growth factor receptor 2 negative (HER2-) and are sensitive to endocrine therapies (ETs). However, approximately 20% of patients have cancer recurrence, usually as incurable metastatic disease, despite such treatment138. Ongoing efforts to improve survival in this subgroup include the development of new endocrine agents or extended duration of ET.
HR+/HER2- BC cells often overexpress cyclin D, which activates cell cycle progression through cyclin-dependent kinases 4 and 6 (CDK4/6). Therefore, HR+/HER2- BC cells are sensitive to CDK4/6 inhibitors, such as oral abemaciclib, palbociclib and ribociclib138.
The combination of CDK4/6 inhibitors with endocrine therapy (ET) has been used successfully in the treatment of HR+/HER2- advanced breast cancer (ABC), showing significantly longer progression-free survival (PFS) and overall survival(OS)131,132,138–147.
Watch this video from our roundtable discussion with leading BC experts on the most interesting data related to CDK4/6 inhibitors for managing BC.
In this section, we focus on the role of CDK4 and CDK6 in the regulation of the cell cycle, BC pathogenesis, and the mode of action for these CDK4/6 inhibitors in BC.
CDK4/6 pathway
CDK4/6 and cell proliferation
The mammalian cell cycle is a tightly regulated, ordered process that is active through four distinct phases termed G1, S, G2 and M (Figure 11)148.
Figure 11. The classical model of the mammalian cell cycle (Adapted148). CDK 1,2,4 or 6, cyclin dependent kinase 1,2,4 or 6; G1, gap 1 phase; G2, gap 2 phase; M, mitosis; S, DNA synthesis.
Between each phase is a controlled checkpoint that is regulated by cyclins and cyclin-dependent kinases (CDKs)148. Cyclin-dependent kinases (CDKs) belong to a family of serine/threonine protein kinases that interact with specific cyclins to promote cell cycle progression (as well as other functions). Cyclins are a diverse family of proteins divided into four classes (A, B, D and E) with multiple members within each class, such as cyclin D1, D2 and D3.
The role of CDK4/6 in the cell cycle
During the G1 phase of the cell cycle, cells must overcome the restriction point, which is a checkpoint that, once passed, commits a cell to the S phase and another cycle of cell division148. Progression through G1 and the restriction point requires synthesis of cyclin D and the formation of a cyclin D:CDK4/6 complex148. A key function of the cyclin D:CDK4/6 complex is to overcome the inhibitory function of the retinoblastoma (RB) protein that binds and sequesters the transcription factor E2F148.
Cyclin D:CDK4/6 complexes phosphorylate RB reducing its ability to bind E2F and enabling E2F to drive the transcription of genes required for the S phase of the cell cycle (Figure 12)149,150. These include cyclin E, which binds CDK2 and promotes progress through the S phase and genes involved in DNA replication.
CyclinD:CDK4 has been shown to directly promote other pathways involved in cell proliferation, migration and the DNA damage response, while CDK6 may play a kinase-independent role in angiogenesis149,151.
Figure 12. The role of cyclin D:CDK4/6 in breast cell proliferation (Adapted149). CDK, cyclin-dependent kinase; E2; oestrogen; E2F, E2 factor; ER, oestrogen receptor; HER, human epidermal growth factor receptor; P, phosphorylation; RB, retinoblastoma protein.
Role of CDK4/6 in breast cancer pathogenesis
Escape of senescence and progression through the cell cycle is essential for cancer development and progression. A number of strategies are utilised by BC cells to achieve this, many resulting in an increase in cyclin D-dependent activity149.
Amplification of CDK4 and cyclin D1 has been observed in 15–25% of BCs, while overexpression of cyclin D1 has been reported in over half of all BCs149. Interestingly, amplification of cyclin D1 and CDK4 genes differs between BC subtypes. Cyclin D1 amplification was seen in 29%, 58% and 38% of luminal A, luminal B and HER2 subtypes, respectively149. Meanwhile, CDK4 amplification was seen in 14%, 25% and 24% of luminal A, luminal B and HER2 subtypes, respectively149. However, reduced expression/mutation/loss of Rb protein is more common in the basal subtype where changes in cyclin D and CDK4 were less common149.
Upstream signalling is also capable of driving increased cyclin D:CDK4/6 activity. Oestrogen activation of ER upregulates cyclin D1 levels culminating in increased activation of CDK4/6 and cell proliferation149. Mitogenic signalling pathways can also promote cyclin D1:CDK4/6 signalling.
Interestingly, cyclin D1 can independently activate ER suggesting a possible mechanism for ER+ cells becoming resistant to hormone therapy and the oestrogen-independence of some ER+ cancers149.
CDK4/6 inhibition
For many years, it was believed that the cyclins and CDKs would be essential to cellular proliferation and normal embryonic development. However, this changed with the discovery that knockout mice lacking individual cyclins or CDKs were viable and double knockouts of CDK4/6 and triple knockouts of cyclin D1, D2 and D3 develop normally until mid-late gestation149. Further, BC cells that become oestrogen-independent and resistant to hormone therapy are still reliant on cyclin D:CDK4/6 signalling to drive proliferation149,152.
With these insights and the likelihood that CDK4/6 may be dispensable for some normal cell function, in addition to existing knowledge on inhibiting kinase activity, CDK4/6 became an increasingly interesting target for drug discovery149.
Many of the initial attempts at CDK inhibition resulted in poor activity and an undesirable adverse event profile. These first generation of CDK inhibitors, including flavopiridol and UCN-01, were essentially pan-CDK inhibitors149,151. Following the poor outcomes associated with pan-CDK inhibition, second generation CDK-specific inhibitors were developed.
While CDK2 was an initial target for many groups looking to develop inhibitors, the focus shifted to inhibition of CDK4/6. In recent years, the first CDK inhibitors targeting CDK4/6, have reached the market (Figure 13)151.
Figure 13. Chemical structures of CDK4/6 inhibitors used to treat HR+/HER2- metastatic breast cancer (Adapted105,118,153,154).
Abemaciclib, palbociclib and ribociclib are all CDK4/6 inhibitors that differ structurally, abemaciclib more so than palbociclib and ribociclib.
Ribociclib and abemaciclib show stronger activity towards CDK4 than CDK6 in in vitro studies whereas palbociclib has similar activity against both kinases155. Abemaciclib is the most potent of the three inhibitors and shows modest activity against a range of other CDKs, including CDK9155. It seems unlikely that this has a significant in vivo effect, given the similar specificity for Rb+ tumour cells versus Rb− tumour cells seen with all the CDK4/6 inhibitors156. However, some differences in adverse events between abemaciclib and palbociclib or ribociclib, utility of abemaciclib as a monotherapy, and the possible future utility of abemaciclib following progression on palbociclib may be explained by this difference in specificity155,157,158. For instance, neutropenia is a similarly common adverse event for both palbociclib and ribociclib; however, it is less common in patients who received abemaciclib. This has ultimately led to differences in dosing between the three CDK4/6 inhibitors, with palbociclib and ribociclib dosed once daily in cycles of three weeks ON and 1 week OFF, whereas abemaciclib can be dosed continuously, twice daily104,105,117,118,154.
Another difference that is worth noting is central nervous system bioavailability, with a higher efflux noted for palbociclib compared with abemaciclib and ribociclib, indicating that the latter two may be better suited to patients with central nervous system involvement156.
CDK4/6 inhibitors mode of action
The role of CDK4/6 in cell proliferation has been extensively studied and it was assumed that inhibition of CDK4/6 would simply prevent cell cycle progression. However, the mechanism of action of CDK4/6 inhibitors may be more complicated than this, involving additional non-cell cycle related effects, including quiescence and senescence, and alterations to metabolism and the immune system156.
Cell cycle inhibition
The classical mechanism of action of CDK4/6 inhibitors is through the inhibition of the cell cycle. Inhibition of CDK4/6 prevents phosphorylation and inactivation of the Rb protein resulting in continued inhibition of the E2F transcription factor149,156. This prevents the transcription of cyclin E and cyclin A which normally promote G1-S progression.
Quiescence versus senescence
The response of tumour cells to CDK4/6 inhibition does not seem to be uniform. Depending on the cell type and transforming event, some Rb-positive cells undergo quiescence while others become senescent. The advantage of creating senescent cells is that they will not return to the cell cycle following removal of the inhibitory signal and are generally resistant to proliferative signals156. Achieving senescence requires cells to transition from quiescence and is termed geroconversion or senescence after growth arrest (SAGA).
CDK4 inhibitor-induced SAGA in breast cancer cells involves the downregulation of mouse double minute 2 homolog 2 (MDM2), redistribution of the chromatin remodeller ATRX and repression of HRAS transcription159,160.
Metabolism and immune system
In vitro experiments have shown CDK4/6 inhibitors, often in combination with other therapies, are capable of manipulating metabolic pathways and driving cells towards apoptosis or senescence. However, these changes are likely to be context-dependent and more research is required to fully understand this mechanism156.
Finally, CDK4/6 inhibition can affect maturation of sentinel cells of the immune system and expansion of regulatory T-cells156. This increase in immune activity is thought to be at least partly related to reduced E2F transcriptional activity161.
In this clip, we asked Dr Laura Spring from the Massachusetts General Hospital Cancer Centre and Harvard Medical School, to tell us when she uses CDK4/6 inhibitors, and for which breast cancer patient groups.
CDK4/6 inhibitor safety and tolerability
CDK4/6 inhibitors are well tolerated, with any side-effects and adverse events resolving with dose modification and supportive care (table 7)162. Haematological toxicities, primarily neutropenia, are the most common side-effect observed with all three inhibitors162. Cytopenias occurring due to CDK4/6 inhibitor treatment are considered an on-target effect due to the role CDK6 plays in the proliferation of haematological precursors162.
Table 7. Adverse event frequency of CDK4/6 inhibitors in phase 3 trials (%) (Adapted162)
| ALT, alanine transaminase; AST, aspartate transaminase | ||||||
| Adverse Event | Palbociclib (%) | Ribociclib (%) | Abemaciclib (%) | |||
| Any grade | Grade 3-4 | Any grade | Grade 3-4 | Any grade | Grade 3-4 | |
| Neutropenia | 80 | 66 | 75 | 60 | 41 | 22 |
| Anaemia | 24 | 5 | 18 | 1 | 28 | 6 |
| Thrombocytopenia | 16 | 1 | 29 | 1 | 10 | 2 |
| Nausea | 35 | <1 | 52 | 2 | 39 | <1 |
| Vomiting | 16 | 1 | 29 | 4 | 28 | 1 |
| Abdominal Pain | 0 | 0 | 11 | 1 | 35 | 1 |
| Diarrhoea | 26 | 1 | 35 | 1 | 81 | 9 |
| Decreased appetite | 15 | 1 | 19 | 2 | 27 | 1 |
| Fatigue | 37 | 2 | 37 | 2 | 46 | 3 |
| AST increase | 52 | 3 | 44 | 7 | 37 | 4 |
| ALT increase | 43 | 2 | 46 | 10 | 48 | 6 |
| Infection | 60 | 7 | 50 | 4 | 39 | 5 |
A frequently reported serious adverse reaction to CDK4/6 inhibitor therapy is venous thromboembolism (VTE)163. The incidence of VTE reported in MONARCH 2 and 3 (4.8% and 6.1%), MONALESSA-3 (4.8%), and PALOMA-1, 2 and 3 (1.6%) has led to warnings about increased VTE risk140,147,164,165. However, as many of these clinical trials excluded patients with pre-existing cardiovascular conditions, the results regarding VTE risk were not an accurate depiction of overall VTE risk among the general real-world population.
This is demonstrated in results from a real-world clinical practice study assessing the rate of VTE following abemaciclib, which differs significantly from the rates seen among the highly selected clinical trial populations. In a multicentre observational cohort study of 364 patients with mBC, 7.4% developed thromboembolic complications over a median treatment duration of 5.5 months, with the median time to thrombosis only 2.8 months after initiating abemaciclib therapy166.
Additionally, it was reported that development of VTE while on abemaciclib therapy was associated with a twofold increase in mortality risk and a much lower overall survival166.
These findings are of particular importance because abemaciclib is the only approved CDK 4/6 inhibitor for use in early breast cancer166.
Similarly, in real-world populations of people treated with palbociclib, the VTE incidence is 6–10%, significantly higher than the 1.6% reported in the clinical trials163,167.
Given the considerable rates of VTE observed in both the clinical trial and the real-world settings, low-risk thromboprophylaxis could be an important consideration for certain patient subgroups receiving abemaciclib166. However, further investigation to quantify the risk and benefits of such an intervention is still required.
Review
- Cyclin-dependent kinases (CDKs) comprise a family of serine/threonine protein kinases that interact with specific cyclins to promote cell cycle progression148
- HR+/HER2− BC cells often overexpress cyclin D, which activates cell cycle progression through cyclin-dependent kinases 4 and 6 (CDK4/6)
- HR+/HER2− BC cells are sensitive to CDK4/6 inhibitors, such as oral abemaciclib, palbociclib and ribociclib138
- CDK4/6 inhibitors are well tolerated, with any side-effects and adverse events resolving with dose modification and supportive care162
- Haematological toxicities, primarily neutropenia, are the most common side-effect observed with all three inhibitors162
- The most frequently reported serious adverse event of CDK4/6 inhibitor therapy is VTE163
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for Clinicians. 2021;71(3):209-249.
- Global Health Estimates : Deaths by Cause, Age, Sex, by Country and by Region, 2000-2019. 2020. Available at: https://gco.iarc.fr/today/data/factsheets/populations/900-world-fact-sheets.pdf.
- Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Annals of Oncology. 2020;31(12):1623-1649.
- Cardoso F, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rubio IT, et al. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2019;30(8):1194-1220.
- Lehmann BD, Jovanović B, Chen X, Estrada MV, Johnson KN, Shyr Y, et al. Refinement of triple-negative breast cancer molecular subtypes: Implications for neoadjuvant chemotherapy selection. PLoS ONE. 2016;11(6):e0157368-e0157368.
- Waks AG, Winer EP. Breast Cancer Treatment: A Review. JAMA - Journal of the American Medical Association. 2019;321(3):288-300.
- Richman J, Dowsett M. Beyond 5 years: enduring risk of recurrence in oestrogen receptor-positive breast cancer. Nature Reviews Clinical Oncology. 2019;16(5):296-311.
- Dowsett M, Turner N. Estimating risk of recurrence for early breast cancer: Integrating clinical and genomic risk. Journal of Clinical Oncology. 2019;37(9):689-692.
- Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years. New England Journal of Medicine. 2017;377(19):1836-1846.
- Dowsett M, Sestak I, Buus R, Lopez-Knowles E, Mallon E, Howell A, et al. Estrogen receptor expression in 21-Gene recurrence score predicts increased late recurrence for estrogen-positive/HER2-Negative breast cancer. Clinical Cancer Research. 2015;21(12):2763-2770.
- Alexandre M, Maran-Gonzalez A, Viala M, Firmin N, D’hondt V, Gutowski M, et al. Decision of adjuvant systemic treatment in HR+ HER2-early invasive breast cancer: Which biomarkers could help? Cancer Management and Research. 2019;11:10353-10373.
- Makki J. Diversity of breast carcinoma: Histological subtypes and clinical relevance. Clinical Medicine Insights: Pathology. 2015;8(1):23-31.
- Tungsukruthai S, Petpiroon N, Chanvorachote P. Molecular mechanisms of breast cancer metastasis and potential anti-metastatic compounds. Anticancer Research. 2018;38(5):2607-2618.
- Cardoso F, Spence D, Mertz S, Corneliussen-James D, Sabelko K, Gralow J, et al. Global analysis of advanced/metastatic breast cancer: Decade report (2005-2015). Breast. 2018;39:131-138.
- Santa-Maria CA, Park SJ, Jain S, Gradishar WJ. Breast cancer and immunology: Biomarker and therapeutic developments. Expert Review of Anticancer Therapy. 2015;15(10):1215-1222.
- Ding Y, Ding K, Yu K, Zou D, Yang H, He X, et al. Prognosis and endocrine therapy selection for patients with low hormone receptor-positive breast cancer following neoadjuvant chemotherapy: A retrospective study of 570 patients in China. Oncology Letters. 2019;18(6):6690-6696.
- Shah R, Rosso K, David Nathanson S. Pathogenesis, prevention, diagnosis and treatment of breast cancer. World Journal of Clinical Oncology. 2014;5(3):283-298.
- Anderson E. The role of oestrogen and progesterone receptors in human mammary development and tumorigenesis. Breast Cancer Research. 2002;4(5):197-201.
- Brisken C. Hormonal control of alveolar development and its implications for breast carcinogenesis. Journal of Mammary Gland Biology and Neoplasia. 2002;7:39-48.
- Rosen JM. Hormone receptor patterning plays a critical role in normal lobuloalveolar development and breast cancer progression. Breast Disease. 2003;18:3-9.
- Yu KD, Cai YW, Wu SY, Shui RH, Shao ZM. Estrogen receptor-low breast cancer: Biology chaos and treatment paradox. Cancer Commun (Lond). 2021;41(10):968-980.
- Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. Journal of Clinical Oncology. 2020;38(12):1346-1366.
- Saha Roy S, Vadlamudi RK. Role of estrogen receptor signaling in breast cancer metastasis. International Journal of Breast Cancer. 2012;2012:65498-65498.
- Treeck O, Schüler-Toprak S, Ortmann O. Estrogen Actions in Triple-Negative Breast Cancer. Cells. 2020;9(11):2358.
- Daniel AR, Hagan CR, Lange CA. Progesterone receptor action: Defining a role in breast cancer. Expert Review of Endocrinology and Metabolism. 2011;6(3):359-369.
- Grimm SL, Hartig SM, Edwards DP. Progesterone Receptor Signaling Mechanisms. Journal of Molecular Biology. 2016;428(19):3831-3849.
- Elster N, Collins DM, Toomey S, Crown J, Eustace AJ, Hennessy BT. HER2-family signalling mechanisms, clinical implications and targeting in breast cancer. Breast Cancer Research and Treatment. 2015;149(1):5-15.
- Gagliato DdM, Jardim DLF, Marchesi MSP, Hortobagyi GN. Mechanisms of resistance and sensitivity to anti-HER2 therapies in HER2+ breast cancer. Oncotarget. 2016;7:64431-64446.
- Morris GJ, Naidu S, Topham AK, Guiles F, Xu Y, McCue P, et al. Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients: A single-institution compilation compared with the national cancer institute's surveillance, epidemiology, and end results database. Cancer. 2007;110(4):876-884.
- Rastelli F, Biancanelli S, Falzetta A, Martignetti A, Casi C, Bascioni R, et al. Triple-negative breast cancer: Current state of the art. Tumori. 2010;96(6):875-888.
- Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, et al. The triple negative paradox: Primary tumor chemosensitivity of breast cancer subtypes. Clinical Cancer Research. 2007;13(8):2329-2334.
- Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, et al. Triple-negative breast cancer: Clinical features and patterns of recurrence. Clinical Cancer Research. 2007;13(15):4429-4434.
- Gao R, Davis A, McDonald TO, Sei E, Shi X, Wang Y, et al. Punctuated copy number evolution and clonal stasis in triple-negative breast cancer. Nature Genetics. 2016;48(10):1119-1130.
- Lee A, Djamgoz MBA. Triple negative breast cancer: Emerging therapeutic modalities and novel combination therapies. Cancer Treatment Reviews. 2018;62:110-122.
- Amir E, Freedman OC, Seruga B, Evans DG. Assessing women at high risk of breast cancer: A review of risk assessment models. Journal of the National Cancer Institute. 2010;102(10):680-691
- Bradley R, Burrett J, Clarke M, Davies C, Duane F, Evans V, et al. Aromatase inhibitors versus tamoxifen in early breast cancer: Patient-level meta-analysis of the randomised trials. The Lancet. 2015;386(10001):1341-1352.
- Mamounas EP, Tang G, Paik S, Baehner FL, Liu Q, Jeong JH, et al. 21-Gene Recurrence Score for prognosis and prediction of taxane benefit after adjuvant chemotherapy plus endocrine therapy: results from NSABP B-28/NRG Oncology. Breast Cancer Research and Treatment. 2018;168(1):69-77.
- Cardoso F, van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, et al. 70-Gene Signature as an Aid to Treatment Decisions in Early-Stage Breast Cancer. New England Journal of Medicine. 2016;375(8):717-729.
- Nitz U, Gluz O, Christgen M, Kates RE, Clemens M, Malter W, et al. Reducing chemotherapy use in clinically high-risk, genomically low-risk pN0 and pN1 early breast cancer patients: five-year data from the prospective, randomised phase 3 West German Study Group (WSG) PlanB trial. Breast Cancer Research and Treatment. 2017;165(3):573-583.
- Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. New England Journal of Medicine. 2018;379(2):111-121.
- Petkov VI, Miller DP, Howlader N, Gliner N, Howe W, Schussler N, et al. Breast-cancer-specific mortality in patients treated based on the 21-gene assay: A SEER population-based study. npj Breast Cancer. 2016;2(1):16017-16017.
- Esserman LJ, Yau C, Thompson CK, Van 't Veer LJ, Borowsky AD, Hoadley KA, et al. Use of molecular tools to identify patients with indolent breast cancers with ultralow risk over 2 decades. JAMA Oncology. 2017;3(11):1503-1510.
- Fallah P, Mulla NK, Aloyz R, Aleynikova O, Florea A, Pelmus M, et al. Can high Ki67 predict distant recurrence in early-stage breast cancer with low Oncotype Dx score? Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 149P.2021.
- Dykewicz CA. Summary of the Guidelines for Preventing Opportunistic Infections among Hematopoietic Stem Cell Transplant Recipients. Clinical Infectious Diseases. 2001;33(2):139-144.
- Wazir U, Mokbel K. Emerging gene-based prognostic tools in early breast cancer: First steps to personalised medicine. World Journal of Clinical Oncology. 2014;5(5):795-799.
- Harbeck N, Sotlar K, Wuerstlein R, Doisneau-Sixou S. Molecular and protein markers for clinical decision making in breast cancer: Today and tomorrow. Cancer Treatment Reviews. 2014;40(3):434-444.
- Drukker CA, Bueno-De-Mesquita JM, Retèl VP, Van Harten WH, Van Tinteren H, Wesseling J, et al. A prospective evaluation of a breast cancer prognosis signature in the observational RASTER study. International Journal of Cancer. 2013;133(4):929-936.
- Zhang Y, Schnabel CA, Schroeder BE, Jerevall PL, Jankowitz RC, Fornander T, et al. Breast cancer index identifies early-stage estrogen receptor-positive breast cancer patients at risk for early- and late-distant recurrence. Clinical Cancer Research. 2013;19(15):4196-4205.
- Hall PS, Smith A, Hulme C, Vargas-Palacios A, Makris A, Hughes-Davies L, et al. Value of Information Analysis of Multiparameter Tests for Chemotherapy in Early Breast Cancer: The OPTIMA Prelim Trial. Value in Health. 2017;20(10):1311-1318.
- Paluch-Shimon S, Cardoso F, Sessa C, Balmana J, Cardoso MJ, Gilbert F, et al. Prevention and screening in BRCA mutation carriers and other breast/ovarian hereditary cancer syndromes: ESMO clinical practice guidelines for cancer prevention and screening. Annals of Oncology. 2016;27(5):v103-v110.
- Antoniou AC, Hardy R, Walker L, Evans DG, Shenton A, Eeles R, et al. Predicting the likelihood of carrying a BRCA1 or BRCA2 mutation: Validation of BOADICEA, BRCAPRO, IBIS, Myriad and the Manchester scoring system using data from UK genetics clinics. Journal of Medical Genetics. 2008;45(7):425-431.
- Atkins CD. Re: Validation of the gail et al. Model for predicting individual breast cancer risk. Journal of the National Cancer Institute. 1994;86(17):1350-1350.
- Bondy ML, Lustbader ED, Halabi S, Ross E, Vogel VG. Validation of a breast cancer risk assessment model in women with a positive family history. Journal of the National Cancer Institute. 1994;86(8):620-625.
- Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, et al. Validation studies for models projecting the risk of invasive and total breast cancer incidence. Journal of the National Cancer Institute. 1999;91(18):1541-1548.
- Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. Journal of the National Cancer Institute. 1989;81(24):1879-1886.
- Cummings SR, Tice JA, Bauer S, Browner WS, Cuzick J, Ziv E, et al. Prevention of breast cancer in postmenopausal women: Approaches to estimating and reducing risk. Journal of the National Cancer Institute. 2009;101(6):384-398.
- Jonker MA, Jacobi CE, Hoogendoorn WE, Nagelkerke NJD, De Bock GH, Van Houwelingen JC. Modeling Familial Clustered Breast Cancer Using Published Data. Cancer Epidemiology Biomarkers and Prevention. 2003;12(12):1479-1485.
- Van Asperen CJ, Jonker MA, Jacobi CE, Van Diemen-Homan JEM, Bakker E, Breuning MH, et al. Risk Estimation for Healthy Women from Breast Cancer Families: New Insights and New Strategies. Cancer Epidemiology Biomarkers and Prevention. 2004;13(1):87-93.
- Antoniou AC, Pharoah PPD, Smith P, Easton DF. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. British Journal of Cancer. 2004;91(8):1580-1590.
- Tyrer J, Duffy SW, Cuzick J. A breast cancer prediction model incorporating familial and personal risk factors. Statistics in Medicine. 2004;23(7):1111-1130.
- McCarthy AM, Guan Z, Welch M, Griffin ME, Sippo DA, Deng Z, et al. Performance of Breast Cancer Risk-Assessment Models in a Large Mammography Cohort. Journal of the National Cancer Institute. 2020;112(5):489-497.
- Vilmun BM, Vejborg I, Lynge E, Lillholm M, Nielsen M, Nielsen MB, et al. Impact of adding breast density to breast cancer risk models: A systematic review. European Journal of Radiology. 2020;127:109019-109019.
- Cox A, Dunning AM, Garcia-Closas M, Balasubramanian S, Reed MWR, Pooley KA, et al. A common coding variant in CASP8 is associated with breast cancer risk. Nature Genetics. 2007;39(3):352-358.
- Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, et al. SEER Cancer Statistics Review. 2015. Available at: https://seer.cancer.gov/csr/1975_2017/ http://seer.cancer.gov/csr/1975_2005/.
- Statistics S. Cancer Statistics Review, 1975–2015. 2017. Available at: https://seer.cancer.gov/archive/csr/1975_2016/%0Ahttps://seer.cancer.gov/csr/1975_2018/%0Ahttps://seer.cancer.gov/archive/csr/1975_2016/.
- Terry MB, Liao Y, Whittemore AS, Leoce N, Buchsbaum R, Zeinomar N, et al. 10-year performance of four models of breast cancer risk: a validation study. Lancet Oncology. 2019;20(4):504-517.
- Davies C, Godwin J, Gray R, Clarke M, Cutter D, Darby S, et al. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: Patient-level meta-analysis of randomised trials. The Lancet. 2011;378(9793):771-784.
- Abe O, Abe R, Enomoto K, Kikuchi K, Koyama H, Masuda H, et al. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. Lancet. 2005;365(9472):1687-1717.
- Ronchi A, Pagliuca F, Zito Marino F, Accardo M, Cozzolino I, Franco R. Current and potential immunohistochemical biomarkers for prognosis and therapeutic stratification of breast carcinoma. Seminars in Cancer Biology. 2021;72:114-122.
- Purdie CA, Quinlan P, Jordan LB, Ashfield A, Ogston S, Dewar JA, et al. Progesterone receptor expression is an independent prognostic variable in early breast cancer: A population-based study. British Journal of Cancer. 2014;110(3):565-572.
- Yeung C, Hilton J, Clemons M, Mazzarello S, Hutton B, Haggar F, et al. Estrogen, progesterone, and HER2/neu receptor discordance between primary and metastatic breast tumours—a review. Cancer and Metastasis Reviews. 2016;35(3):427-437.
- Mohsin SK, Weiss H, Havighurst T, Clark GM, Berardo M, Roanh LD, et al. Progesterone receptor by immunohistochemistry and clinical outcome in breast cancer: A validation study. Modern Pathology. 2004;17(12):1545-1554.
- Kamranzadeh H, Ardekani RM, Kasaeian A, Sadighi S, Maghsudi S, Jahanzad I, et al. Association between Ki-67 expression and clinicopathological features in prognosis of breast cancer: A retrospective cohort study. Journal of Research in Medical Sciences. 2019;24(1):30-30.
- Anderson WF, Rosenberg PS, Katki HA. Tracking and evaluating molecular tumor markers with cancer registry data: HER2 and breast cancer. Journal of the National Cancer Institute. 2014;106(5).
- Corti C, Giugliano F, Nicolò E, Tarantino P, Criscitiello C, Curigliano G. HER2-Low Breast Cancer: a New Subtype? Current Treatment Options in Oncology. 2023;24(5):468-478.
- Gampenrieder SP, Rinnerthaler G, Tinchon C, Petzer A, Balic M, Heibl S, et al. Landscape of HER2-low metastatic breast cancer (MBC): results from the Austrian AGMT_MBC-Registry. Breast Cancer Res. 2021;23(1):112.
- Sakai H, Tsurutani J, Ozaki Y, Ishiguro H, Nozawa K, Watanabe K, et al. Multicentre, randomised, double-blind, placebo-controlled phase II study of prophylactic olanzapine for patients with metastatic breast cancer receiving T-DXd treatment: protocol for the ERICA study (WJOG14320B). BMJ Open. 2023;13(4):e070304.
- Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N Engl J Med. 2022;387(1):9-20.
- Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. Journal of Clinical Investigation. 2011;121(7):2750-2767.
- Bareche Y, Venet D, Ignatiadis M, Aftimos P, Piccart M, Rothe F, et al. Unravelling triple-negative breast cancer molecular heterogeneity using an integrative multiomic analysis. Annals of Oncology. 2018;29(4):895-902.
- Burstein MD, Tsimelzon A, Poage GM, Covington KR, Contreras A, Fuqua SAW, et al. Comprehensive genomic analysis identifies novel subtypes and targets of triple-negative breast cancer. Clinical Cancer Research. 2015;21(7):1688-1698.
- Stefansson OA, Jonasson JG, Johannsson OT, Olafsdottir K, Steinarsdottir M, Valgeirsdottir S, et al. Correction: Genomic profiling of breast tumours in relation to BRCA abnormalities and phenotypes. Breast Cancer Research. 2009;11(5):R47-R47.
- Karaayvaz M, Cristea S, Gillespie SM, Patel AP, Mylvaganam R, Luo CC, et al. Unravelling subclonal heterogeneity and aggressive disease states in TNBC through single-cell RNA-seq. Nature Communications. 2018;9(1):3588-3588.
- Johnston SJ, Cheung K-L. Endocrine Therapy for Breast Cancer: A Model of Hormonal Manipulation. Oncology and Therapy. 2018;6(2):141-156.
- Segovia-Mendoza M, González-González ME, Barrera D, Díaz L, García-Becerra R. Efficacy and mechanism of action of the tyrosine kinase inhibitors gefitinib, lapatinib and neratinib in the treatment of her2-positive breast cancer: Preclinical and clinical evidence. American Journal of Cancer Research. 2015;5:2531-2561.
- Gluz O, Scheffen I, Degenhardt T, Marschner NW, Christgen M, Kreipe HH, et al. ADAPTlate: A randomized, controlled, open-label, phase III trial on adjuvant dynamic marker—Adjusted personalized therapy comparing abemaciclib combined with standard adjuvant endocrine therapy versus standard adjuvant endocrine therapy in (clinical or ge. Presented at the American Society of Clinical Oncology (ASCO) congress 2021, 4–8 June 2021, Virtual. TPS598.2021.
- Fleissig A, Jenkins V, Catt S, Fallowfield L. Multidisciplinary teams in cancer care: are they effective in the UK? Lancet Oncology. 2006;7(11):935-943.
- Sainsbury R, Haward R, Round C, Rider L, Johnston C. Influence of clinician workload and patterns of treatment on survival from breast cancer. The Lancet. 1995;345(8960):1265-1270.
- Chang JH, Vines E, Bertsch H, Fraker DL, Czerniecki BJ, Rosato EF, et al. The impact of a multidisciplinary breast cancer center on recommendations for patient management: The university of Pennsylvania experience. Cancer. 2001;91(7):1231-1237.
- Vinod SK, Sidhom MA, Delaney GP. Do multidisciplinary meetings follow guideline-based care? Journal of Oncology Practice. 2010;6(6):276-281.
- Saini KS, Taylor C, Ramirez AJ, Palmieri C, Gunnarsson U, Schmoll HJ, et al. Role of the multidisciplinary team in breast cancer management: results from a large international survey involving 39 countries. Annals of Oncology. 2012;23(4):853-859.
- Kesson EM, Allardice GM, George WD, Burns HJG, Morrison DS. Effects of multidisciplinary team working on breast cancer survival: Retrospective, comparative, interventional cohort study of 13 722 women. BMJ (Online). 2012;344(7856).
- Harbeck N, Kates RE, Look MP, Meijer-van Gelder ME, Klijn JGM, Krüger A, et al. Enhanced benefit from adjuvant chemotherapy in breast cancer patients classified high-risk according to urokinase-type plasminogen activator (uPA) and plasminogen activator inhibitor type 1 (n = 3424). Cancer Research. 2002;62(16):4617-4622.
- Tutt A, Garber JE, Kaufman B, Viale G, Fumagalli D, Rastogi P, et al. OlympiA: A phase III, multicenter, randomized, placebo-controlled trial of adjuvant olaparib after (neo)adjuvant chemotherapy in patients with germline BRCA1/2 mutations and high-risk HER2-negative early breast cancer. Presented at the American Society of Clinical Oncology (ASCO) congress 2021, 4–8 June 2021, Virtual. LBA1.2021.
- Tung NM, Zakalik D, Somerfield MR. Adjuvant PARP Inhibitors in Patients With High-Risk Early-Stage HER2-Negative Breast Cancer and Germline BRCA Mutations: ASCO Hereditary Breast Cancer Guideline Rapid Recommendation Update. J Clin Oncol. 2021;39(26):2959-2961.
- FDA. FDA approves olaparib plus bevacizumab as maintenance treatment for ovarian, fallopian tube, or primary peritoneal cancers. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-olaparib-plus-bevacizumab-maintenance-treatment-ovarian-fallopian-tube-or-primary.
- Mohammed AA, Rashied H, Elsayed FM. CDK4/6 inhibitors in advanced breast cancer, what is beyond? Oncology Reviews. 2019;13(2):125-133.
- Ma CX, Gao F, Luo J, Northfelt DW, Goetz M, Forero A, et al. NeoPalAna: Neoadjuvant palbociclib, a cyclin-dependent kinase 4/6 inhibitor, and anastrozole for clinical stage 2 or 3 estrogen receptor–positive breast cancer. Clinical Cancer Research. 2017;23(15):4055-4065.
- Johnston SRD, Harbeck N, Hegg R, Toi M, Martin M, Shao ZM, et al. Abemaciclib Combined With Endocrine Therapy for the Adjuvant Treatment of HR+, HER2-, Node-Positive, High-Risk, Early Breast Cancer (monarchE). J Clin Oncol. 2020;38(34):3987-3998.
- Mayer EL, Dueck AC, Martin M, Rubovszky G, Burstein HJ, Bellet-Ezquerra M, et al. Palbociclib with adjuvant endocrine therapy in early breast cancer (PALLAS): interim analysis of a multicentre, open-label, randomised, phase 3 study. The Lancet Oncology. 2021;22(2):212-222.
- A study of palbociclib in addition to standard endocrine treatment in hormone receptor positive HER2 normal patients with residual disease after neoadjuvant chemotherapy and surgery (PENELOPE-B). 2016. Available at: https://clinicaltrials.gov/ct2/show/NCT01864746.
- Adjuvant Ribociclib With Endocrine Therapy in Hormone Receptor+/HER2- High Risk Early Breast Cancer. 2017. Available at: https://clinicaltrials.gov/show/NCT03078751.
- Slamon DJ, Fasching PA, Patel R, Verma S, Hurvitz SA, Chia SKL, et al. NATALEE: Phase III study of ribociclib (RIBO) + endocrine therapy (ET) as adjuvant treatment in hormone receptor–positive (HR+), human epidermal growth factor receptor 2–negative (HER2–) early breast cancer (EBC). Journal of Clinical Oncology. 2019;37(15_suppl):TPS597-TPS597.
- Abemaciclib, Verzenios® SmPC. 2022. Available at: https://www.medicines.org.uk/emc/product/9532/smpc.
- Abemaciclib, VERZENIO® | Highlights of Prescribing Information. 2023. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/208716s006s007s008lbl.pdf. Accessed 2023.
- Gnant M, Singer CF, Rinnerthaler G, Pfeiler G, Egle D, Balic M, et al. Position paper on CDK4/6 inhibitors in early breast cancer. memo - Magazine of European Medical Oncology. 2023.
- Loibl S, Marme F, Martin M, Untch M, Bonnefoi H, Kim SB, et al. Palbociclib for Residual High-Risk Invasive HR-Positive and HER2-Negative Early Breast Cancer-The Penelope-B Trial. J Clin Oncol. 2021;39(14):1518-1530.
- Novartis Kisqali® Phase III NATALEE trial meets primary endpoint at interim analysis demonstrating clinically meaningful benefit in broad population of patients with early breast cancer [press release]. Available at: https://www.novartis.com/news/media-releases/novartis-kisqali-phase-iii-natalee-trial-meets-primary-endpoint-interim-analysis-demonstrating-clinically-meaningful-benefit-broad-population-patients-early-breast-cancer. Accessed May 2023.
- Hattori M, Iwata H. Advances in treatment and care in metastatic breast cancer (MBC): Are there MBC patients who are curable? Chinese Clinical Oncology. 2018;7(3).
- O'Shaughnessy J. Extending Survival with Chemotherapy in Metastatic Breast Cancer. The Oncologist. 2005;10(S3):20-29.
- Kashaf MS, McGill E. Does shared decision making in cancer treatment improve quality of life? A systematic literature review. Medical Decision Making. 2015;35(8):1037-1048.
- Savard M-F, Khan O, Hunt KK, Verma S. Redrawing the lines: The next generation of treatment in metastatic breast cancer. American Society of Clinical Oncology Educational Book. 2019(39):e8-e21.
- Twelves C, Cheeseman S, Sopwith W, Thompson M, Riaz M, Ahat-Donker N, et al. Systemic treatment of hormone receptor positive, human epidermal growth factor 2 negative metastatic breast cancer: Retrospective analysis from Leeds Cancer Centre. BMC Cancer. 2020;20(1):53-53.
- Matutino A, Joy AA, Brezden-Masley C, Chia S, Verma S. Hormone receptor-positive, HER2-negative metastatic breast cancer: Redrawing the lines. Current Oncology. 2018;25:S131-S141.
- NCCN. Breast cancer - Metastatic: NCCN Guidelines for Patients. https://www.nccn.org/patients/guidelines/content/PDF/stage_iv_breast-patient.pdf. Accessed 11 May.
- Ballinger TJ, Meier JB, Jansen VM. Current landscape of targeted therapies for hormone-receptor positive, HER2 negative metastatic breast cancer. Frontiers in Oncology. 2018;8:308-308.
- Palbociclib, IBRANCE® SmPC. 2020. Available at: https://www.ema.europa.eu/en/documents/product-information/ibrance-epar-product-information_en.pdf.
- Ribociclib, KISQALI® SmPC. 2020. Available at: https://www.ema.europa.eu/en/documents/product-information/kisqali-epar-product-information_en.pdf.
- Zawadzki P, Woźna A, Sztromwasser P, Majer-Burman W, Stępień R, Pacewicz K, et al. Personalized medicine in advanced breast cancer: AI-driven genomic test for CDK4/6 treatment response prediction. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 1134P.2021.
- Presti D, Quaquarini E. The PI3K/AKT/mTOR and CDK4/6 pathways in endocrine resistant HR+/HER2- metastatic breast cancer: Biological mechanisms and new treatments. Cancers. 2019;11(9).
- Vinayak S, Carlson RW. mTOR inhibitors in the treatment of breast cancer. ONCOLOGY (United States). 2013;27(1).
- O'Shaughnessy J, Thaddeus Beck J, Royce M. Everolimus-based combination therapies for HR+, HER2− metastatic breast cancer. Cancer Treatment Reviews. 2018;69:204-214.
- Alpelisib, PIQRAY® | Highlights of Prescribing Information. 2020. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212526s000lbl.pdf. Accessed 14 May 2020.
- Vernieri C, Corti F, Nichetti F, Ligorio F, Manglaviti S, Zattarin E, et al. Everolimus versus alpelisib in advanced hormone receptor-positive HER2-negative breast cancer: Targeting different nodes of the PI3K/AKT/mTORC1 pathway with different clinical implications. Breast Cancer Research. 2020;22:33-33.
- Pavithran K, Jayamohanan H, Jose WM, Soman S, Vijaykumar DK, Ariyannur PS. PI3K mutation is associated with reduced sensitivity to CDK4/6 inhibitors in metastatic breast cancer. Presented at European Society for Medical Oncology (ESMO) Congress 2021, 16–21 September 2021. Virtual. 256P.2021.
- Schedin TB, Borges VF, Shagisultanova E. Overcoming Therapeutic Resistance of Triple Positive Breast Cancer with CDK4/6 Inhibition. International Journal of Breast Cancer. 2018;2018.
- Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of Chemotherapy plus a Monoclonal Antibody against HER2 for Metastatic Breast Cancer That Overexpresses HER2. New England Journal of Medicine. 2001;344(11):783-792.
- Pernas S, Tolaney SM. HER2-positive breast cancer: new therapeutic frontiers and overcoming resistance. Therapeutic Advances in Medical Oncology. 2019;11.
- Managing advanced breast cancer - NICE Pathways. 2020. Available at: https://pathways.nice.org.uk/pathways/advanced-breast-cancer#content=view-node%3Anodes-hrpos-and-her2pos&path=view%3A/pathways/advanced-breast-cancer/managing-advanced-breast-cancer.xml.
- Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LA, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5).
- Azim HA, Ghosn M, Oualla K, Kassem L. Personalized treatment in metastatic triple‐negative breast cancer: The outlook in 2020. The Breast Journal. 2020;26(1):69-80.
- Li CH, Karantza V, Aktan G, Lala M. Current treatment landscape for patients with locally recurrent inoperable or metastatic triple-negative breast cancer: A systematic literature review. Breast Cancer Research. 2019;21(1):143-143.
- Sacituzumab govitecan, Trodelvy® | SmPC. 2021. Available at: https://www.ema.europa.eu/en/documents/product-information/trodelvy-epar-product-information_en.pdf. Accessed April 2023.
- Sacitzumab govitecan highlights of prescribing information. 2023. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/761115s035lbl.pdf. Accessed 25 May 2023.
- Pembrolizumab highlights of presribing. 2021. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/125514s089s114lbl.pdf. Accessed 25 May 2023.
- Pembrolizumab product information. 2023. Available at: https://www.ema.europa.eu/en/documents/product-information/keytruda-epar-product-information_en.pdf. Accessed 25 May 2023.
- NCT03941730. Estradiol in Treating Patients With ER Beta Positive, Triple Negative Locally Advanced or Metastatic Breast Cancer. 2022. Available at: https://clinicaltrials.gov/ct2/show/NCT03941730. Accessed May 2023.
- Curigliano G. CDK4/6 inhibitors for HR+HER2− early stage breast cancer — when to escalate treatment? Nature Reviews Clinical Oncology. 2021;18(2):67-68.
- Dickler MN, Tolaney SM, Rugo HS, Cortes J, Dieras V, Patt D, et al. MONARCH 1, a phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, n patients with refractory HR+/HER2- metastatic breast cancer. Clinical Cancer Research. 2017;23(17):5218-5224.
- Sledge GW, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2-advanced breast cancer who had progressed while receiving endocrine therapy. Journal of Clinical Oncology. 2017;35(25):2875-2884.
- Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im S-A, et al. Overall Survival with Ribociclib plus Fulvestrant in Advanced Breast Cancer. New England Journal of Medicine. 2020;382(6):514-524.
- Tripathy D, Im SA, Colleoni M, Franke F, Bardia A, Harbeck N, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. The Lancet Oncology. 2018;19(7):904-915.
- Xu QQ, Pan B, Wang CJ, Zhou YD, Mao F, Lin Y, et al. HER2 amplification level is not a prognostic factor for HER2-positive breast cancer with trastuzumab-based adjuvant treatment: A systematic review and meta-analysis. Oncotarget. 2016;7(39):63571-63582.
- Im S-A, Lu Y-S, Bardia A, Harbeck N, Colleoni M, Franke F, et al. Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. New England Journal of Medicine. 2019;381(4):307-316.
- Sledge GW, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. The Effect of Abemaciclib Plus Fulvestrant on Overall Survival in Hormone Receptor-Positive, ERBB2-Negative Breast Cancer That Progressed on Endocrine Therapy - MONARCH 2: A Randomized Clinical Trial. JAMA Oncology. 2020;6(1):116-124.
- Goetz MP, Toi M, Campone M, Trédan O, Bourayou N, Sohn J, et al. MONARCH 3: Abemaciclib as initial therapy for advanced breast cancer. Journal of Clinical Oncology. 2017;35(32):3638-3646.
- Johnston S, Martin M, Di Leo A, Im SA, Awada A, Forrester T, et al. MONARCH 3 final PFS: a randomized study of abemaciclib as initial therapy for advanced breast cancer. npj Breast Cancer. 2019;5(1):1-8.
- Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: A changing paradigm. Nature Reviews Cancer. 2009;9:153-166.
- Finn RS, Aleshin A, Slamon DJ. Targeting the cyclin-dependent kinases (CDK) 4/6 in estrogen receptor-positive breast cancers. Breast Cancer Research. 2016;18(1).
- Rugo HS, Finn RS, Diéras V, Ettl J, Lipatov O, Joy AA, et al. Palbociclib plus letrozole as first-line therapy in estrogen receptor-positive/human epidermal growth factor receptor 2-negative advanced breast cancer with extended follow-up. Breast Cancer Research and Treatment. 2019;174(3):719-729.
- Murphy CG, Dickler MN. The role of CDK4/6 inhibition in breast cancer. The Oncologist. 2015;20(5):483-490.
- Iwata H. Clinical development of CDK4/6 inhibitor for breast cancer. Breast Cancer. 2018;25(4):402-406.
- Xu H, Yu S, Liu Q, Yuan X, Mani S, Pestell RG, et al. Recent advances of highly selective CDK4/6 inhibitors in breast cancer. Journal of Hematology and Oncology. 2017;10(1):97-97.
- Palbociclib, IBRANCE® | Highlights of Prescribing Information. 2019. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212436lbl.pdf. Accessed 2020.
- Marra A, Curigliano G. Are all cyclin-dependent kinases 4/6 inhibitors created equal? npj Breast Cancer. 2019;5(1).
- Klein ME, Kovatcheva M, Davis LE, Tap WD, Koff A. CDK4/6 Inhibitors: The Mechanism of Action May Not Be as Simple as Once Thought. Cancer Cell. 2018;34:9-20.
- Wander SA, Zangardi M, Niemierko A, Kambadakone A, Kim LSL, Xi J, et al. A multicenter analysis of abemaciclib after progression on palbociclib in patients (pts) with hormone receptor-positive (HR+)/HER2- metastatic breast cancer (MBC). Journal of Clinical Oncology. 2019;37(15_suppl):1057-1057.
- Mariotti V, Khong HT, Soliman HH, Costa RL, Fisher S, Boulware D, et al. Efficacy of abemaciclib (abema) after palbociclib (palbo) in patients (pts) with metastatic breast cancer (MBC). Journal of Clinical Oncology. 2019;37(15_suppl):e12521-e12521.
- Kovatcheva M, Liao W, Klein ME, Robine N, Geiger H, Crago AM, et al. ATRX is a regulator of therapy induced senescence in human cells. Nature Communications. 2017;8(1).
- Kovatcheva M, Liu DD, Dickson MA, Klein ME, O'Connor R, Wilder FO, et al. MDM2 turnover and expression of ATRX determine the choice between quiescence and senescence in response to CDK4 inhibition. Oncotarget. 2015;6(10):8226-8243.
- Goel S, Decristo MJ, Watt AC, Brinjones H, Sceneay J, Li BB, et al. CDK4/6 inhibition triggers anti-tumour immunity. Nature. 2017;548(7668):471-475.
- Spring LM, Wander SA, Andre F, Moy B, Turner NC, Bardia A. Cyclin-dependent kinase 4 and 6 inhibitors for hormone receptor-positive breast cancer: past, present, and future. The Lancet. 2020;395(10226):817-827.
- West MT, Smith CE, Kaempf A, Kohs TCL, Amirsoltani R, Ribkoff J, et al. CDK 4/6 inhibitors are associated with a high incidence of thrombotic events in women with breast cancer in real-world practice. Eur J Haematol. 2021;106(5):634-642.
- Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Annals of Oncology. 2018;29(7):1541-1547.
- Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. The Lancet Oncology. 2016;17(4):425-439.
- Watson NW, Wander SA, Shatzel JJ, Al-Samkari H. Venous and arterial thrombosis associated with abemaciclib therapy for metastatic breast cancer. Cancer. 2022;128(17):3224-3232.
- Yan MM, Wu SS, Qi YP, Li ZR, Zhang Q, Zhao H, et al. Association between cyclin-dependent kinase 4/6 inhibitors and venous thromboembolism: analysis of F.A.E.R.S. data. Expert Opin Drug Saf. 2022;21(2):277-283.
of interest
are looking at
saved
next event
This content has been developed independently by Medthority who previously received educational funding from Eli Lilly in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
