Understanding MS
Understanding Multiple Sclerosis
Multiple sclerosis
MS is an autoimmune disease characterised by inflammation and damage to the central nervous system (CNS). Common MS symptoms include impairments to cognition, walking, and balance; bladder or bowel dysfunction; abnormal tiredness; or visual disturbances1. The symptoms of MS are caused by peripherally driven inflammation and neurodegeneration of the CNS2-5.
MS is characterised by four disease courses or phenotypes6,7:
- clinically isolated syndrome (CIS)
- relapsing-remitting MS (RRMS)
- secondary progressive MS (SPMS)
- primary-progressive MS (PPMS)
The course of the disease is indicated by evidence of progression, active disease and relapses, and the extent and nature of disability7. PPMS differs in important ways from RRMS and SPMS, discussed below, and can be considered apart from relapsing forms of the disease6.
The onset of MS is typically marked by CIS, which is the first episode of neurological symptoms caused by inflammation or demyelination in the CNS. CIS, which must persist for at least 24 hours, does not yet satisfy diagnostic criteria for MS as people who experience CIS may or may not develop MS8. RRMS, however can develop from CIS3,4,6.
Approximately 85% of people with MS are initially diagnosed with RRMS8. RRMS is characterised by clearly defined episodes of new or increasing neurologic symptoms (‘relapses’, ‘exacerbations’), followed by periods of partial or complete recovery (‘remissions’)6. RRMS can be characterised as ‘active’ (with relapses and/or evidence of new magnetic resonance imaging [MRI] activity over a period of time) or ‘not active’, and ‘worsening’ (a confirmed increase in disability following a relapse), or ‘not worsening’6.
SPMS follows an initial relapsing-remitting course. Some people with RRMS transition to a secondary progressive course, which shows progressive worsening of neurologic function (accumulation of disability) over time. SPMS can be characterised as ‘active’ (with relapses and/or evidence of new MRI activity during a period of time) or ‘not active’, and ‘with progression’ (evidence of disability accumulation over time, with or without relapses or new MRI activity), or ‘without progression’7.
A standardised definition of SPMS has not been developed. Assessments that consider other manifestations of MS disability are required. Clinical tools are being developed for establishing a standardised assessment based on patient-physician discussions of clinical history9.
Following 6–10 years from MS onset, approximately 25%–40% of people with RRMS have progressed to SPMS, with a median time to transition ranging from 10 to 23 years10–13
PPMS is characterised by worsening neurologic function from symptom onset, without early relapses or remissions. PPMS can be described as ‘active’ (with an occasional relapse and/or evidence of new MRI activity over time), or ‘not active’, and ‘with progression’ or ‘without progression’6.
PPMS differs in important ways from relapsing forms of MS (RRMS, SPMS):
- People with PPMS tend to have fewer brain lesions than people with RRMS or SPMS
- Brain lesions in people with PPMS may contain fewer inflammatory cells
- People with PPMS may exhibit more lesions in the spinal cord than in the brain
- The average age of onset is approximately 10 years later in PPMS than RRMS or SPMS
- People with PPMS commonly have more difficulty walking and remaining in the workforce than people with RRMS or SPMS
Approximately 15% of people with MS are diagnosed with PPMS8.
Overview of MS epidemiology
In 2020, approximately 2.8 million people worldwide had MS (Figure 1)14,15.
Figure 1. Number of people with multiple sclerosis per 100,000 worldwide, 2020 (Adapted14). MS, multiple sclerosis.
Onset of MS commonly occurs between the ages of 20–404. MS affects more women than men: 69% of people with MS are women, 31% are men14.
The prevalence of familial MS is approximately 11.8%16. Environmental and lifestyle risk factors include Epstein-Barr virus (EBV) infection in adolescence and early adulthood, tobacco exposure through active or passive smoking, low levels of vitamin D, a lack of sun exposure, and obesity during adolescence4,14.
Every 5 minutes, someone, somewhere in the world, is diagnosed with MS14
Unmet needs
There are common unmet needs in people living with MS, and for HCPs treating MS (Table 1)17-22.
Table 1. Unmet needs in people with MS and healthcare professionals (Adapted17-22). HCP, healthcare professional; MS, multiple sclerosis.
| Patient unmet needs | Healthcare professional unmet needs |
| Symptom Management | |
| · A cure for MS | · A cure for MS |
| · Invisible/‘hidden’ symptoms are not detected during neurological consultations · Invisible/‘hidden’ symptoms and mental health aspects of MS are difficult to communicate · HCPs do not always perceive patients holistically, or understand what is important to the patient ‘as a whole’ |
· Lack of treatments to manage progressive MS, or MS symptoms |
| · Practical needs relating to disease disability and quality of life | |
| Access to treatment | |
| · Lack of access to treatment and treatment support | · Inability to offer specific therapies due to local treatment stipulations, or high treatment costs · Need for more research into the impact of current therapies on quality-of-life outcomes · Perception that patients with MS prefer not to discuss risks of treatment · Time spent counselling and providing information is often not reimbursed |
| · Some HCPs are reluctant to prescribe particular therapies | |
| · Lack of awareness of specific therapies/latest therapeutic options | |
| · Dialogue on risk and benefits of treatment, not only the risks | |
| · More attention to personalised care needs | |
| Personalised care | |
| · Dissatisfaction with the limited time of consultations | · Professional training on personalised and holistic care · Time to communicate with patients and the multidisciplinary teams about the most appropriate treatment options |
| Education and information | |
| · Educational resources often lack MS information, with little consideration of specific disease states | · Professional education and understanding of the needs of patients · Information for patients needs to come from vetted and reliable sources |
Potential actions to help address some of these unmet needs in both people and HCPs could include17-22:
- Improve the quality of all interactions between HCPs and their patients
- Collaborate to form ‘joint’ local education, communication, and patient-engagement initiatives
- Motivate people to self-manage their MS
- Optimise consultation time
- Understand and optimally manage ‘hidden’ disease symptoms
- Improve benefit versus risk communication as related to MS therapies
- Provide accurate, clear information about MS in an accessible format
- Share new knowledge and information about MS with multidisciplinary team members, HCPs, and patients
Greater use of patient-centred educational resources before, during, and after consultations to improve understanding and communication of MS, is essential22
By bridging unmet needs, patients are better equipped to make informed decisions with HCPs, as part of a multidisciplinary, individualised disease management approach7,23,24.
Management of multiple sclerosis
Introduction
Multiple sclerosis (MS) is an immune-mediated disease, caused by peripherally driven inflammation and neurodegeneration of the central nervous system (CNS)2-5.
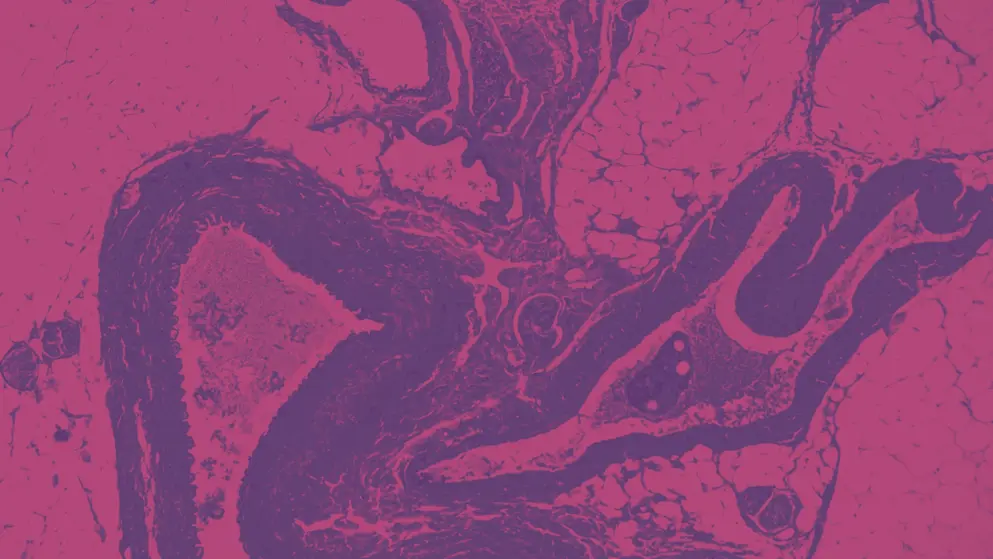
As MS progresses, lesions in the CNS and the brain indicate advancement from neuroinflammation to neurodegeneration, leading to irreversible neuroaxonal degeneration, demyelination, and cumulative disability, diminishing mobility, cognitive decline, and loss of independence2-5.
MS disease phenotypes comprise clinically isolated syndrome (CIS), relapsing remitting (RRMS), secondary progressive (SPMS), and primary progressive (PPMS)6,7. Approximately 85% of people with MS are diagnosed with RRMS8. As described in the previous section, PPMS differs from relapsing MS phenotypes (RRMS, SPMS) in important ways. Almost 15% of people with MS are diagnosed with PPMS6.
Follow the link to learn some of the important differences between PPMS and relapsing forms of MS
The development of relapsing forms of MS, excluding PPMS, is shown in Figure 225.
Figure 2. Evolution of relapsing forms of multiple sclerosis – RRMS, SPMS (Adapted26-30). CIS, clinically isolated syndrome; CNS, central nervous system; GM, grey matter; MRI, magnetic resonance imaging; MS, multiple sclerosis; RRMS, relapsing-remitting multiple sclerosis; SPMS, secondary progressive multiple sclerosis; WM, white matter.
Referral timing and pathways
People who report symptoms that might be MS-related should be referred to a neurologist as early as possible31. The aspirational goal for referral is 5 days31.
A patient ought to receive follow-up evaluations every 6 months and, minimally, once per year31. During these evaluations, people are assessed for treatment efficacy, MS progression, and if they are living a ‘brain-healthy’ lifestyle31. Healthcare professionals (HCPs) should also probe at follow-up for unmet patient needs32.
Early diagnosis
Even with improved diagnostic tools and criteria, diagnosis delays are common in people with MS (Figure 3)33. Psychiatric manifestations may mask early symptoms of MS and can be associated with delays in diagnosis34.
Figure 3. Delayed diagnosis of multiple sclerosis (Adapted33). MRI, magnetic resonance imaging.
Referral to a neurologist is advised at the earliest signs of MS symptoms31,33. Early diagnosis and intervention may slow the progression of MS, and benefit long-term patient outcomes.
Diagnoses that present similarly to MS include vasculitis, HIV infection, Lyme disease, thyroid dysfunction, and several nutritional deficiencies35. Typical findings consistent with a diagnosis of MS include T2 (and T1 post gadolinium) hyperintense periventricular lesions, known as Dawson fingers36. Spinal cord lesions are usually longitudinally oriented; their length does not extend beyond 1 or 2 spinal segments, and their width does not extend more than half the diameter of the cord36. The McDonald criteria states that the key requirements for MS diagnosis are dissemination in time, damage to the CNS at different dates, and dissemination in space, damage to different parts the CNS. It uses MRI evidence to test these criteria and suggest an MRI scan should be carried out where MS diagnosis could be a possibility37.
Conventional neuroimaging can miss or underestimate CNS damage. White matter can appear normal on a conventional MRI scan, while higher-resolution testing not available as part of routine clinical care, and/or immunohistochemical techniques, can identify widespread axonal damage indicating disease activity that may or may not be associated with clinical symptoms38. There is an unmet need for information and support at neurology clinics for people with MS, particularly at the time of diagnosis39.
While an early diagnosis is important, avoiding misdiagnosis, due to diverse clinical presentations of MS, and tests with high sensitivity, but limited specificity, should also be considered40.
Biomarkers
Dozens of biomarkers are currently being evaluated to improve diagnostic accuracy and to monitor disease activity that relates to MRI pathology41-43. In addition, many potential markers are being evaluated on their usefulness as prognostic for conversion from CIS to MS and for disability progression42.
Table 2 shows the classification and clinical uses of biomarkers for MS44.
| MS, multiple sclerosis. | |
| Biomarkers | Description |
| Predictive | Risk to Develop MS |
| Diagnostic | Fast Interpretation of Pathological State of MS |
| Prognosis | Outcome or Course of MS |
| Disease-Associated Activity | Demonstration of Current MS Condition as Inflammation, Demyelination, Cognitive Dysfunction, etc. |
| Response to Treatment | Predict Response to Therapy in MS Patients |
Serum neurofilament light chain (sNfL) is a component of neurofilament found in the neuronal cytoplasm. When an axon is damaged, cytoskeletal proteins, including neurofilaments, are released into the extracellular space and subsequently into the CSF and the blood45. It is important to note that changes in sNfL can highlight neurodegeneration, and is not specific to MS46.
- In people with RMS, sNfL levels are correlated with neuroinflammatory and neurodegenerative activity41,45,47
- Baseline sNfL levels are associated with T2 lesion volume, and Gd+ lesions as early as the first demyelinating event48
- Higher concentrations of sNfL in people with CIS and RMS are related to higher MRI lesion load and higher disability scores49
Glial fibrillary acidic protein (GFAP) is an astrocyte-specific skeletal protein that is encoded by the GFAP gene in humans. GFAP is released into CSF and blood upon activation or glial cell damage50.
GFAP is a candidate serum biomarker to assess disease severity in progressive forms of MS, particularly in combination with NfL51,52.
In the EXPAND HET trial, GFAP was retrospectively analysed as an exploratory biomarker53,54:
- High baseline GFAP levels were significantly associated with high Expanded Disability Status Scale (EDSS), low Symbol Digit Modalities Test (SDMT) score, presence of Gd+ lesions, and a high T2 lesion volume at baseline
- Siponimod reduced GFAP levels from baseline to EOS by 1.2%, compared to 9.2% increase in placebo group
Progress is being made to identify diagnostic or prognostic biomarkers for MS. Advances in biomarker identification and validation could improve treatments, reduce relapses and delay disease progression44.
Early intervention
Early intervention can maximise the chances of altering the course of MS before the disease progresses further, even if the disease minimally impacts the patient’s functioning33,55-57.
Delayed treatment of MS is associated with worsening disease course and poorer response to treatments31
Starting treatment early (<2 years after diagnosis) is associated with a 40% reduction in risk of progression in people who had a first event of MS, or clinically isolated syndrome (CIS)25.
Early initiation of high-efficacy therapies (HETs) can be accompanied by other appropriate steps to help preserve brain tissue and optimise brain health early in the disease course, including exercise, meditation, music therapy, social engagement, smoking cessation, weight loss, and control of comorbidities33,58,59. These steps may improve the chances of altering the MS course before further relapses or disability progression occur33.
In a cohort analysis of 592 people from the UK with MS who were prescribed pharmacological treatment, long-term outcomes were more favourable with early intensive therapy versus starting on first-line moderate-efficacy treatment60.
There is increasing evidence that initiating HET early in MS may more effectively manage MS, and therefore may be a good choice to prevent irreversible progression, especially in people with forms of RRMS at risk of early and rapid advancement of disability43,55,56,61-63.
In addition, analytical models have shown that early treatment of MS is cost-effective for the health care provider and society, as well as slowing MS progression64.
Immunoglobulins in MS
Immunoglobulins (Igs), also termed antibodies, function as part of the healthy immune system to destroy bacteria and viruses (Figure 4)65.
In MS, however, excessive amounts of IgG and IgM antibodies in the CSF, as measured using an oligoclonal band (OCB) assay, are associated with inflammation and active lesions66-68. Often used as a marker of inflammation in the diagnosis of MS43, the presence of oligoclonal IgG bands in the CSF are seen in up to 95% of people with MS66.
Immune-modulating HETs target the immune system to reduce the autoimmune reaction in MS69. The question of the impact of these medications, in particular B-cell depleting treatments, on the ability of people with MS to elicit a suitable immune response to infections and post-vaccination is relevant in the time of the COVID pandemic70. Evidence continues to emerge on the impact of B-cell depleting anti-CD20 therapies on IgG and IgM serum levels, with data indicating varying levels of reduction over time for the available treatments70,71.
Figure 4. Immunoglobulins (Adapted65). Ig, immunoglobulin.
Holistic patient care
The optimal holistic patient care plan is management by specialists and HCPs with expertise in treating people with MS72.
MS specialists, primarily neurologists and MS nurses, will be most familiar with symptoms and MS progression, and are best positioned to manage the treatment options for people72, which may include pharmacological and/or non-pharmacological treatments.
Other stakeholders who may play a critical role in supporting patient needs include psychologists, physiotherapists, case workers, social workers, and community support groups72.
Together, these MS care units can provide seamless and efficient care across the continuum of MS72. This communication and trust between HCPs and people with MS, can help identify invisible symptoms and ultimately improve quality of life73.
Education for people with MS is critical for adherence with care plans, and is associated with improved satisfaction and better adherence to treatment22. In some people with MS, however, education alone may be insufficient to improve outcomes. For example, physician referral to an exercise program is twice as effective as simply providing written information from Physical Activity Guidelines to adults with MS74.
References
- Gross HJ, Watson C. Characteristics, burden of illness, and physical functioning of patients with relapsing-remitting and secondary progressive multiple sclerosis: A cross-sectional US survey. Neuropsychiatric Disease and Treatment. 2017;13:1349-1357.
- Baecher-Allan C, Kaskow BJ, Weiner HL. Multiple Sclerosis: Mechanisms and Immunotherapy. Neuron. 2018;97:742-768.
- Dendrou CA, Fugger L, Friese MA. Immunopathology of multiple sclerosis. Nature Reviews Immunology. 2015;15:545-558.
- Filippi M, Bar-Or A, Piehl F, Preziosa P, Solari A, Vukusic S, et al. Multiple sclerosis. Nature Reviews Disease Primers. 2018;4(1):1-27.
- Hemmer B, Kerschensteiner M, Korn T. Role of the innate and adaptive immune responses in the course of multiple sclerosis. The Lancet Neurology. 2015;14:406-419.
- Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sørensen PS, Thompson AJ, et al. Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology. 2014;83:278-286.
- NICE. Multiple sclerosis in adults: management. https://www.nice.org.uk/guidance/ng220. Accessed 23 October 2022.
- National Multiple Sclerosis Society. Types of MS. https://www.nationalmssociety.org/What-is-MS/Types-of-MS. Accessed 23 October 2022.
- Cree BAC, Arnold DL, Chataway J, Chitnis T, Fox RJ, Pozo Ramajo A, et al. Secondary Progressive Multiple Sclerosis. New Insights. 2021;97(8):378-388.
- Koch M, Kingwell E, Rieckmann P, Tremlett H, Adams D, Craig D, et al. The natural history of secondary progressive multiple sclerosis. Journal of Neurology, Neurosurgery and Psychiatry. 2010;81(9):1039-1043.
- Rovaris M, Confavreux C, Furlan R, Kappos L, Comi G, Filippi M. Secondary progressive multiple sclerosis: Current knowledge and future challenges. Lancet Neurology. 2006;5:343-354.
- Scalfari A, Neuhaus A, Daumer M, Muraro PA, Ebers GC. Onset of secondary progressive phase and long-term evolution of multiple sclerosis. Journal of Neurology, Neurosurgery and Psychiatry. 2014;85(1):67-75.
- Tremlett H, Zhao Y, Devonshire V. Natural history of secondary-progressive multiple sclerosis. Multiple Sclerosis. 2008;14(3):314-324.
- MS International Federation. Atlas of MS background. http://www.msif.org/about-us/advocacy/atlas/atlas-of-ms/. Accessed 23 October 2022.
- Kister I, Bacon TE, Chamot E, Salter AR, Cutter GR, Kalina JT, et al. Natural history of multiple sclerosis symptoms. International Journal of MS Care. 2013;15(3):146-158.
- Ehtesham N, Rafie MZ, Mosallaei M. The global prevalence of familial multiple sclerosis: an updated systematic review and meta-analysis. BMC Neurology. 2021;21(1):246.
- Borreani C, Bianchi E, Pietrolongo E, Rossi M, Cilia S, Giuntoli M, et al. Unmet needs of people with severe multiple sclerosis and their carers: Qualitative findings for a home-based intervention. PLoS One. 2014;9(10):e109679-e109679.
- Davies F, Wood F, Brain KE, Edwards M, Jones R, Wallbank R, et al. The transition to secondary progressive multiple sclerosis: An exploratory qualitative study of health professionals' experiences. International Journal of MS Care. 2016;18(5):257-264.
- Lonergan R, Kinsella K, Fitzpatrick P, Duggan M, Jordan S, Bradley D, et al. Unmet needs of multiple sclerosis patients in the community. Multiple Sclerosis and Related Disorders. 2015;4(2):144-150.
- Mehr SR, Zimmerman MP. Reviewing the unmet needs of patients with multiple sclerosis. American Health and Drug Benefits. 2015;8(8):426-431.
- Ponzio M, Tacchino A, Vaccaro C, Traversa S, Brichetto G, Battaglia MA, et al. Unmet needs influence health-related quality of life in people with multiple sclerosis. Multiple sclerosis and related disorders. 2020;38:101877-101877.
- Rieckmann P, Centonze D, Elovaara I, Giovannoni G, Havrdová E, Kesselring J, et al. Unmet needs, burden of treatment, and patient engagement in multiple sclerosis: A combined perspective from the MS in the 21st Century Steering Group. Multiple Sclerosis and Related Disorders. 2018;19:153-160.
- Rae-Grant A, Day GS, Marrie RA, Rabinstein A, Cree BAC, Gronseth GS, et al. Comprehensive systematic review summary: Disease-modifying therapies for adults with multiple sclerosis. Neurology. 2018;90(17):789-800.
- Rae-Grant A, Day GS, Marrie RA, Rabinstein A, Cree BAC, Gronseth GS, et al. Practice guideline recommendations summary: Disease-modifying therapies for adults with multiple sclerosis. Neurology. 2018;90:777-788.
- Ziemssen T, Derfuss T, de Stefano N, Giovannoni G, Palavra F, Tomic D, et al. Optimizing treatment success in multiple sclerosis. Journal of Neurology. 2016;263:1053-1065.
- Bar-Or A. The immunology of multiple sclerosis. Seminars in Neurology. 2008;28:29-45.
- Cree BAC, Hollenbach JA, Bove R, Kirkish G, Sacco S, Caverzasi E, et al. Silent progression in disease activity–free relapsing multiple sclerosis. Annals of Neurology. 2019;85(5):653-666.
- Kutzelnigg A, Lucchinetti CF, Stadelmann C, Brück W, Rauschka H, Bergmann M, et al. Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain. 2005;128(11):2705-2712.
- Larochelle C, Uphaus T, Prat A, Zipp F. Secondary Progression in Multiple Sclerosis: Neuronal Exhaustion or Distinct Pathology? Trends in Neurosciences. 2016;39:325-339.
- Mahad DH, Trapp BD, Lassmann H. Pathological mechanisms in progressive multiple sclerosis. The Lancet Neurology. 2015;14:183-193.
- Hobart J, Bowen A, Pepper G, Crofts H, Eberhard L, Berger T, et al. International consensus on quality standards for brain health-focused care in multiple sclerosis. Multiple Sclerosis Journal. 2019;25(13):1809-1818.
- Lorefice L, Fenu G, Frau J, Coghe G, Marrosu MG, Cocco E. The impact of visible and invisible symptoms on employment status, work and social functioning in Multiple Sclerosis. Work. 2018;60(2):263-270.
- Giovannoni G, Butzkueven H, Dhib-Jalbut S, Hobart J, Kobelt G, Pepper G, et al. Brain health: time matters in multiple sclerosis. Multiple Sclerosis and Related Disorders. 2016;9:S5-S48.
- Byatt N, Rothschild AJ, Riskind P, Ionete C, Hunt AT. Relationships Between Multiple Sclerosis and Depression. Journal of Neuropsychiatry and Clinical Neurosciences. 2011;23(2):198-200.
- Shull C, Hoyle B, Iannotta C, Fletcher E, Curan M, Cipollone V. A current understanding of multiple sclerosis. JAAPA : official journal of the American Academy of Physician Assistants. 2020;33(2):19-23.
- Siva A. Common Clinical and Imaging Conditions Misdiagnosed as Multiple Sclerosis: A Current Approach to the Differential Diagnosis of Multiple Sclerosis. Neurol Clin. 2018;36:69-117.
- MS Trust. McDonald Criteria. https://mstrust.org.uk/a-z/mcdonald-criteria. Accessed 24 October 2022.
- Marriott JJ. Safety and Efficacy of Fingolimod in Treatment-Naïve Multiple Sclerosis Patients. Journal of Central Nervous System Disease. 2011;3:JCNSD.S5120-JCNSD.S5120.
- Mortensen GL, Rasmussen PV. The impact of quality of life on treatment preferences in multiple sclerosis patients. Patient Preference and Adherence. 2017;11:1789-1796.
- Brownlee WJ, Solomon AJ. Misdiagnosis of multiple sclerosis: Time for action. Multiple Sclerosis Journal. 2021;27(6):805-806.
- Kapoor R, Smith KE, Allegretta M, Arnold DL, Carroll W, Comabella M, et al. Serum neurofilament light as a biomarker in progressive multiple sclerosis. Neurology. 2020;95(10):436-444.
- Toscano S, Patti F. CSF biomarkers in multiple sclerosis: beyond neuroinflammation. Neuroimmunology and Neuroinflammation. 2020;2020(1):14-41.
- Ziemssen T, Akgün K, Brück W. Molecular biomarkers in multiple sclerosis. Journal of Neuroinflammation. 2019;16:1-11.
- Mathur D, Mishra BK, Rout S, Lopez-Iranzo FJ, Lopez-Rodas G, Vallamkondu J, et al. Potential Biomarkers Associated with Multiple Sclerosis Pathology. International Journal of Molecular Sciences. 2021;22(19):10323.
- Disanto G, Barro C, Benkert P, Naegelin Y, Schädelin S, Giardiello A, et al. Serum Neurofilament light: A biomarker of neuronal damage in multiple sclerosis. Annals of Neurology. 2017;81(6):857-870.
- Ferreira-Atuesta C, Reyes S, Giovanonni G, Gnanapavan S. The Evolution of Neurofilament Light Chain in Multiple Sclerosis. Frontiers in Neuroscience. 2021;15:383-383.
- Kuhle J, Kropshofer H, Haering DA, Kundu U, Meinert R, Barro C, et al. Blood neurofilament light chain as a biomarker of MS disease activity and treatment response. Neurology. 2019;92(10):E1007-E1015.
- Jakimovski D, Kuhle J, Ramanathan M, Barro C, Tomic D, Hagemeier J, et al. Serum neurofilament light chain levels associations with gray matter pathology: a 5-year longitudinal study. Annals of Clinical and Translational Neurology. 2019;6(9):1757-1770.
- Dalla Costa G, Martinelli V, Sangalli F, Moiola L, Colombo B, Radaelli M, et al. Prognostic value of serum neurofilaments in patients with clinically isolated syndromes. Neurology. 2019;92(7):E733-E741.
- Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541(7638):481-487.
- Abdelhak A, Huss A, Kassubek J, Tumani H, Otto M. Serum GFAP as a biomarker for disease severity in multiple sclerosis. Scientific Reports. 2018;8(1):14798-14798.
- Högel H, Rissanen E, Vuorimaa A, Airas L. Positron emission tomography imaging in evaluation of MS pathology in vivo. Multiple Sclerosis Journal. 2018;24(11):1399-1412.
- Kappos L, Bar-Or A, Cree BAC, Fox RJ, Giovannoni G, Gold R, et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): a double-blind, randomised, phase 3 study. The Lancet. 2018;391(10127):1263-1273.
- Kuhle J, Kropshofer H, Maceski AM, Dahlke F, Hach T, Tomic D, et al. Plasma Glial Fibrillary Acidic Protein Correlates with Characteristics of Advanced Disease and Treatment Response in Secondary Progressive Multiple Sclerosis. Presented at the AAN Annual Meeting 2020, 26 April. Available at: https://issuu.com/americanacademyofneurology/docs/aan_science2020_book.
- Gartner J, Hauser S, Bar-Or A, Montalban X, Cohen J, Cross AH, et al. Benefit-risk of ofatumumab in treatment-naïve early relapsing multiple sclerosis patients. Multiple Sclerosis Journal. 2020;26:210-210.
- He A, Merkel B, Brown JWL, Zhovits Ryerson L, Kister I, Malpas CB, et al. Timing of high-efficacy therapy for multiple sclerosis: a retrospective observational cohort study. The Lancet Neurology. 2020;19(4):307-316.
- Turner B, Cree BAC, Kappos L, Montalban X, Papeix C, Wolinsky JS, et al. Ocrelizumab efficacy in subgroups of patients with relapsing multiple sclerosis. Journal of Neurology. 2019;266(5):1182-1193.
- Senders A, Wahbeh H, Spain R, Shinto L. Mind-body medicine for multiple sclerosis: A systematic review. Autoimmune Dis. 2012;1.
- Strober LB, Becker A, Randolph JJ. Role of positive lifestyle activities on mood, cognition, well-being, and disease characteristics in multiple sclerosis. Applied Neuropsychology:Adult. 2018;25(4):304-311.
- Harding K, Williams O, Willis M, Hrastelj J, Rimmer A, Joseph F, et al. Clinical Outcomes of Escalation vs Early Intensive Disease-Modifying Therapy in Patients with Multiple Sclerosis. JAMA Neurology. 2019;76(5):536-541.
- Fyfe I. Progressive and aggressive MS — new frontiers emerge. Nature Research 2021. 2018(December):2018-2018.
- Grandmaison F, Yeung M, Morrow S, Lee L, Emond F, Ward B, et al. Sequencing of high-efficacy disease-modifying therapies in multiple sclerosis: Perspectives and approaches. Neural Regeneration Research. 2018;13:1871-1874.
- Stankiewicz JM, Weiner HL. An argument for broad use of high efficacy treatments in early multiple sclerosis. Neurology(R) neuroimmunology & neuroinflammation. 2020;7:636-636.
- Tinelli M, Pugliatti M, Antonovici A, Hausmann B, Hellwig K, Quoidbach V, et al. Averting multiple sclerosis long-term societal and healthcare costs: The Value of Treatment (VoT) project. Multiple Sclerosis and Related Disorders. 2021;54.
- MSD Manual. Molecular Components of the Immune System https://www.msdmanuals.com/en-gb/professional/immunology-allergic-disorders/biology-of-the-immune-system/molecular-components-of-the-immune-system. Accessed 24 October 2022.
- Dobson R, Ramagopalan S, Davis A, Giovannoni G. Cerebrospinal fluid oligoclonal bands in multiple sclerosis and clinically isolated syndromes: A meta-analysis of prevalence, prognosis and effect of latitude. Journal of Neurology, Neurosurgery and Psychiatry. 2013;84(8):909-914.
- Gilden D, Devlin M, Wroblewska Z. A technique for the elution of cell‐surface antibody from human brain tissue. Annals of Neurology. 1978;3(5):403-405.
- Lucchinetti C, Brück W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. Heterogeneity of multiple sclerosis lesions: Implications for the pathogenesis of demyelination. Annals of Neurology. 2000;47(6):707-717.
- Reder AT, Centonze D, Naylor ML, Nagpal A, Rajbhandari R, Altincatal A, et al. COVID-19 in Patients with Multiple Sclerosis: Associations with Disease-Modifying Therapies. CNS Drugs. 2021;35(3):317-330.
- Flores-Gonzalez RE, Hernandez J, Tornes L, Rammohan K, Delgado S. Development of SARS-CoV-2 IgM and IgG antibodies in a relapsing multiple sclerosis patient on ofatumumab. Multiple Sclerosis and Related Disorders. 2021;49:102777-102777.
- Lee DSW, Rojas OL, Gommerman JL. B cell depletion therapies in autoimmune disease: advances and mechanistic insights. Nature Reviews Drug Discovery 2020 20:3. 2020;20(3):179-199.
- Soelberg Sorensen P, Giovannoni G, Montalban X, Thalheim C, Zaratin P, Comi G. The Multiple Sclerosis Care Unit. Multiple Sclerosis Journal. 2019;25(5):627-636.
- Lakin L, Davis BE, Binns CC, Currie KM, Rensel MR. Comprehensive Approach to Management of Multiple Sclerosis: Addressing Invisible Symptoms—A Narrative Review. Neurology and Therapy. 2021;10(1):75-98.
- Canning KL, Hicks AL. Physician referral improves adherence to the physical activity guidelines for adults with MS: A randomized controlled trial. Multiple Sclerosis and Related Disorders. 2020;37.
This content has been developed independently by Medthority who previously received educational funding from Novartis Pharma AG in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
