Oncology
Our specialist oncology resources cover the latest guidelines and scientific updates to support your clinical practice, from assessing patient risk of disease recurrence to identifying unmet needs.
Medical conditions
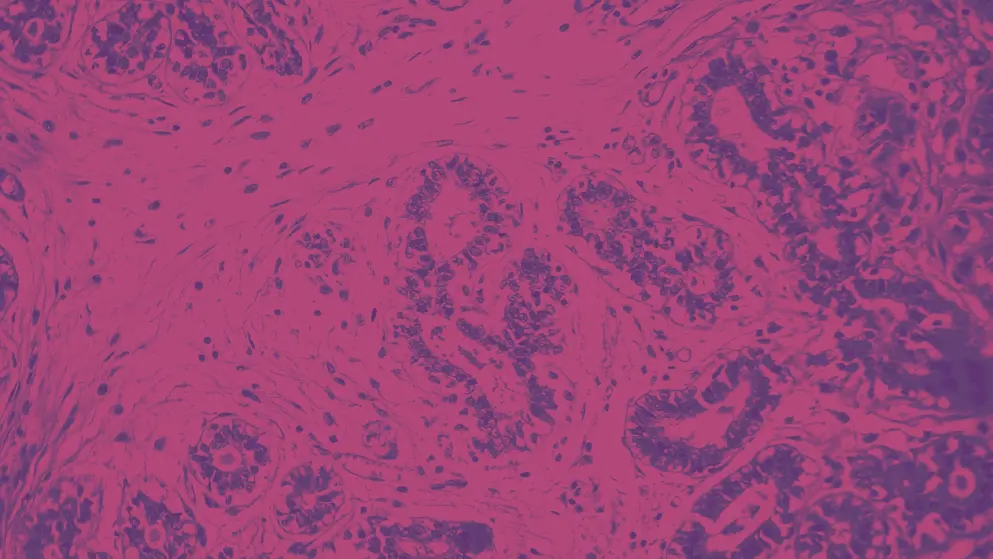
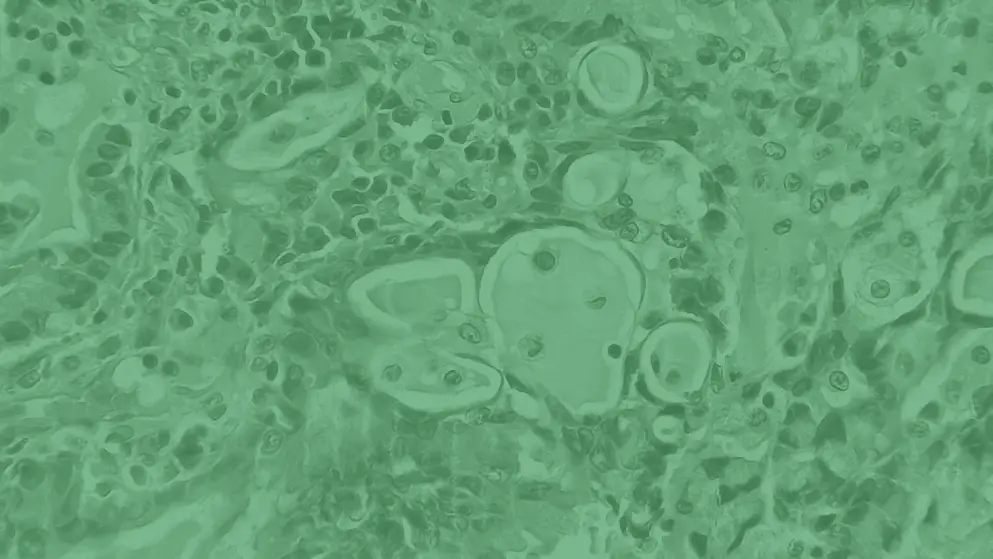
Bladder cancer
Expert congress highlights and recent advances
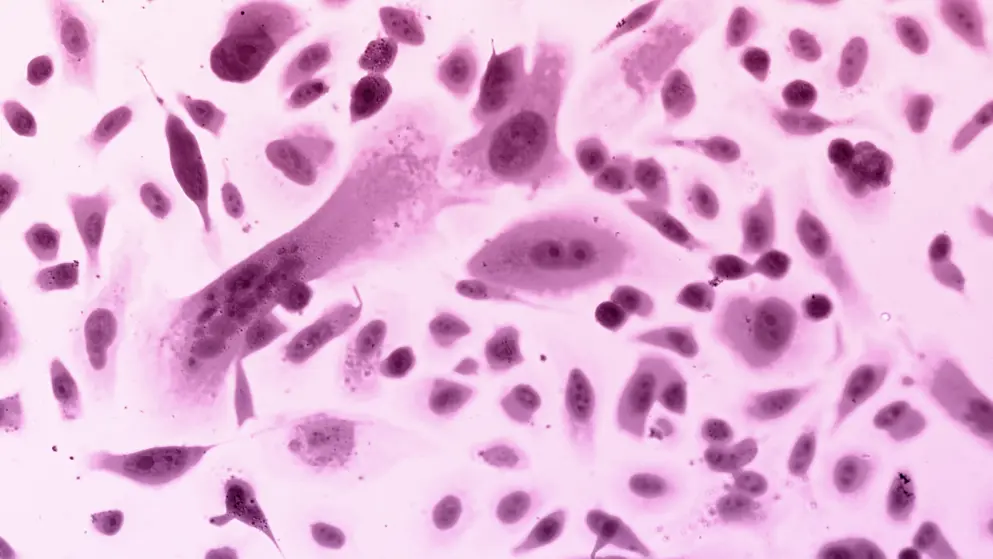
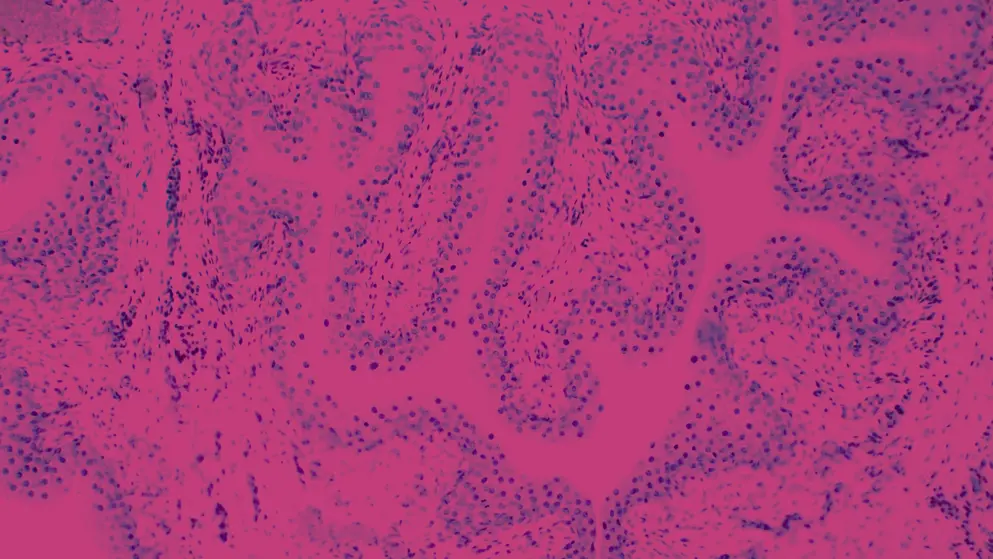
Breast cancer
Expert podcast and congress highlights
Colorectal cancer
Disease information and treatment guidelines
Leukemia
Latest news, insights, and guideline updates
Lymphoma
Earn CME credit, plus expert congress highlights
Multiple myeloma
Latest news, insights, and guideline updates
Lung cancer
Latest insights and spotlight articles
Ovarian cancer
Latest news, insights, and guideline updates
Prostate Cancer Nexus
Congress coverage and expert podcasts
Thyroid cancer
Latest news, insights, and guideline updates
DGHO 2025: Desmoid tumor updates
Watch expert insights on updates in desmoid tumor care, from Deutsche Gesellschaft für Hämatologie und Medizinische Onkologie (DGHO) 2025.
Browse older resources
Breast Cancer 2023 Wrapped
End of 2023 review of major advancements in HER2+ breast cancer with content from recently held SABCS and other major oncology congresses
ESMO Breast Cancer 2022 – Congress Highlights
Follow all the latest developments with daily highlights from the European Society of Medical Oncology Breast Cancer Congress in Berlin, Germany, 3–5 May 2022.
Future breast cancer care: ESMO Breast Cancer 2024
Congress coverage of ESMO Breast Cancer 2024, featuring the latest advances in research, treatment updates, expert interviews, and key takeaways.
PARP Inhibitor Selection in Ovarian Cancer Learning Zone
Up to date on the latest treatments for advanced ovarian cancer? Get expert insights and case studies on PARP inhibitors in ovarian cancer.
Molecular Diagnostics for RET Inhibition in NSCLC and Thyroid Cancers
Discover assorted resources and expert opinions on molecular diagnostics for RET inhibition in non-small cell lung cancer (NSCLC) and thyroid cancers.
Symposium Overview
The 44th Annual San Antonio Breast Cancer Symposium (SABCS) 2021 was its first hybrid meeting.
St. Gallen International Breast Cancer Conference 2023 - Day 1
Highlights and key developments from the 2023 St. Gallen International Breast Cancer Conference, 15-18 March in Vienna