Dementia
Dementia refers to a group of clinical symptoms characterized by progressive cognitive and psychological decline that interferes with daily functioning. It encompasses multiple etiologies, with Alzheimer’s disease representing the most prevalent subtype (60–80% of cases).
How is dementia characterized?
Core clinical features may include impaired memory and visuospatial skills, executive dysfunction, speech impairment, and neuropsychiatric symptoms, such as apathy, agitation, or hallucinations.
Pathophysiological mechanisms vary by dementia type:
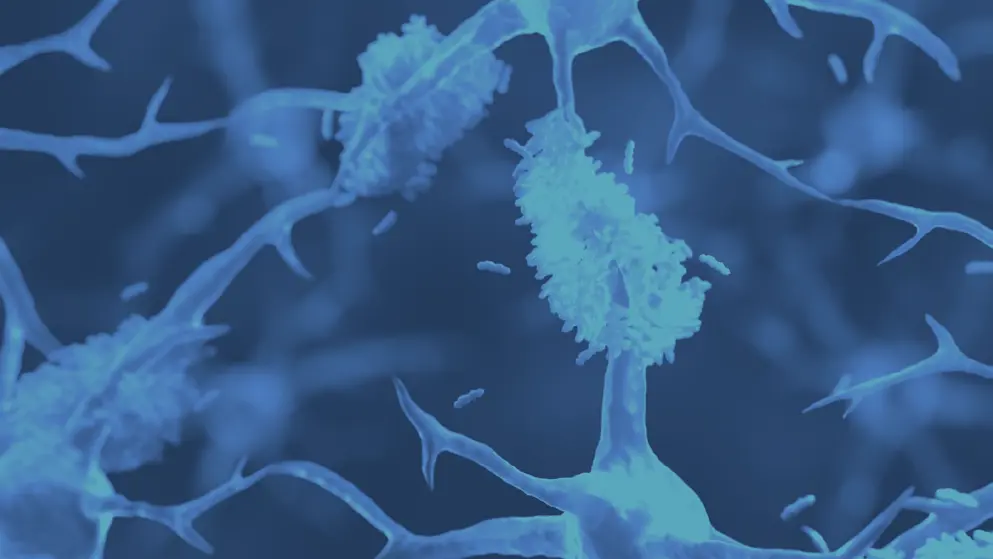
- Alzheimer’s is characterized by the accumulation of abnormal protein plaques and tangles in the brain
- Vascular dementia results from reduced brain blood flow due to small vessel blockages or microscopic bleeding
- Lewy body dementia is associated with accumulation of abnormal protein clumps, primarily composed of alpha-synuclein
- Frontotemporal dementia involves focal neurodegeneration of frontal and temporal lobes
What are the diagnostic criteria?
Neuroimaging is important in the diagnostic work-up of patients with dementia. Structural MRI is indicated to exclude treatable causes of cognitive impairment and assess patterns of atrophy, whereas functional imaging (FDG-PET) may assist subtype differentiation.
Diagnostic evaluation also includes detailed history, cognitive assessment, neurological examination, and laboratory studies. Biomarkers and neuropsychological testing may support differential diagnosis, particularly in specialized settings.
What are the treatment approaches?
There is no disease-modifying treatment for most forms of dementia. However, cholinesterase inhibitors (e.g., donepezil) and NMDA receptor antagonists (e.g., memantine) may offer symptomatic benefit in dementia.
What are the recommended strategies for dementia risk reduction?
Addressing modifiable risk factors across the life course is advised. Emerging evidence supports a multimodal approach to prevention. Around 40% of dementia cases worldwide may be preventable or delayed by addressing 12 modifiable risk factors.
Risk reduction strategies include management of factors such as hypertension, diabetes, obesity, hearing loss, depression, smoking, physical inactivity, and social isolation.
Developed by EPG Health for Medthority, independently of any sponsor.

