Nontraditional (non-Western pharmaceutical) treatments for chronic kidney disease
Nontraditional (non-Western pharmaceutical) treatments for chronic kidney disease
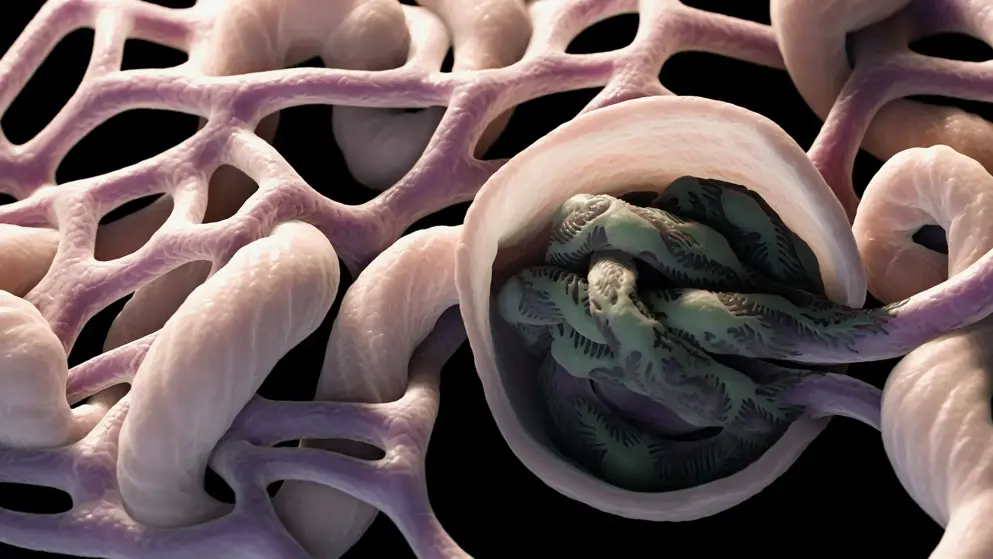
Nontraditional, non-Western medicines, often called complementary and alternative medicines (CAM), for chronic kidney disease (CKD) patients are, potentially, a huge low-cost therapy resource for poorer populations in the world. Use of CAM, particularly from plant sources, is common in poorer communities, but the scientific basis for their use is still under-researched and under-published. This review presents information on the treatment of kidney disease with CAM, particularly CKD and its closely associated cardiovascular disease (CVD), which might benefit vulnerable populations. The challenges of developing CAM therapies for resource-limited environments are also discussed, particularly with reference to targeting oxidative stress, a known cause of progressive diseases such as CKD and CVD. Oxidative stress is a mechanism often targeted by CAM, with good scientific basis. Dietary supplementation with antioxidants is one approach to reducing CKD incidence or morbidity. Antioxidant supplementation in populations with sufficient dietary antioxidant intake often report little benefit. In comparison, poorer populations that may have restricted nutritional dietary antioxidant intake may benefit from supplementation with antioxidants. Also needing consideration are the recorded instances of nephrotoxicity from CAM therapies, particularly related to nephrotoxic plant extracts, extract-drug reactions, and toxicity from contaminants within the extracts. As long as the possible toxicity of plant-derived CAM is considered, we argue that populations having marked deficiency in, or poor access to, dietary antioxidants, or high exposure to environmental oxidants, may benefit from these nontraditional medicines.
Read abstract on library site Access full article