Fluid overload as a therapeutic target for the preservative management of chronic kidney disease
Fluid overload as a therapeutic target for the preservative management of chronic kidney disease
Purpose of review: There is growing clinical evidence of adverse effects of fluid overload on kidney outcomes in patients with cardiovascular disease who are not yet receiving kidney replacement therapy. In this review, we discuss the patient populations most at risk for fluid overload, the pathophysiology associated with fluid overload, and finally treatment options.
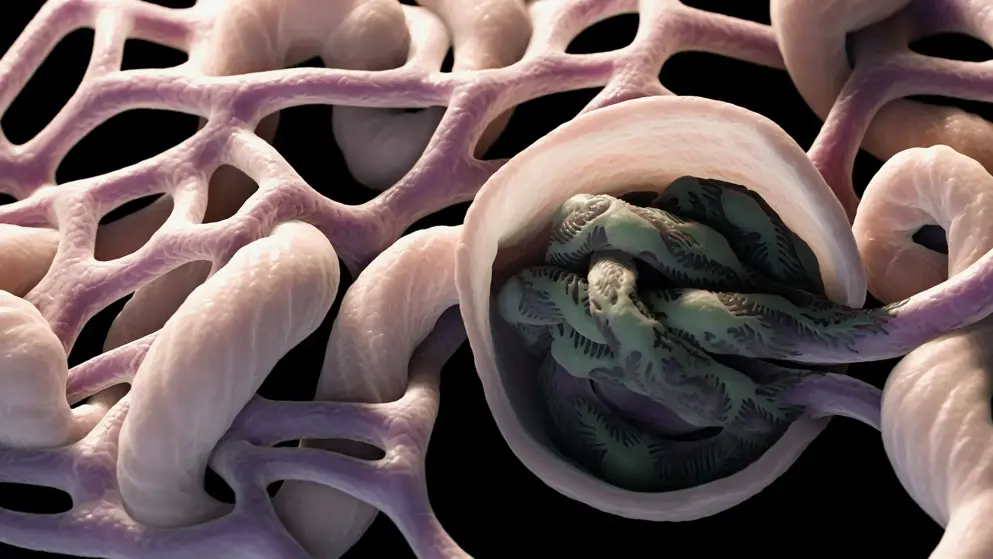
Recent findings: The severity of fluid overload is an independent risk factor for both an increased risk of rapidly declining kidney function and increased risk for the need of kidney replacement therapy. High venous pressure within the kidney secondarily causes a decrease in kidney perfusion, which in turn signals salt retention and the resulting increase in plasma volume completes a vicious cycle propagating ongoing kidney injury. Fluid overload has also been identified as a risk factor for the combined outcome of all-cause mortality and cardiovascular morbidity. This increased risk in some studies has been identified as more important than hypertension in predicting both the increased risk of kidney disease progression and morbidity and mortality from cardiovascular disease. Once fluid status is accurately assessed, a combination of salt restriction and effective diuretic therapy is the first-line therapy to manage this complication. In those patients who require additional therapy, use of a V2 receptor antagonists can be considered. Finally, some patients may benefit from peritoneal dialysis to bring about volume removal even if they do not yet require dialysis for uremic complications.
Summary: Excess fluid or fluid overload appears to enhance chronic kidney disease progression and its treatment and resolution is a potential disease-modifying intervention.
Read abstract on library site Access full article
Featured Learning Zones
You may be interested in...
The 2023 update of the German Society of Neurology’s guideline on Parkinson’s disease (PD) provides detailed recommendations on the use of transcranial brain parenchyma sonography (TCS) for early and differential diagnosis. This update addresses previously unspecified diagnostic criteria and investigator qualifications, offering a robust framework based on a systematic literature review.