Chronic Kidney Disease Diagnosis and Management: A Review
Chronic Kidney Disease Diagnosis and Management: A Review
Importance: Chronic kidney disease (CKD) is the 16th leading cause of years of life lost worldwide. Appropriate screening, diagnosis, and management by primary care clinicians are necessary to prevent adverse CKD-associated outcomes, including cardiovascular disease, end-stage kidney disease, and death.
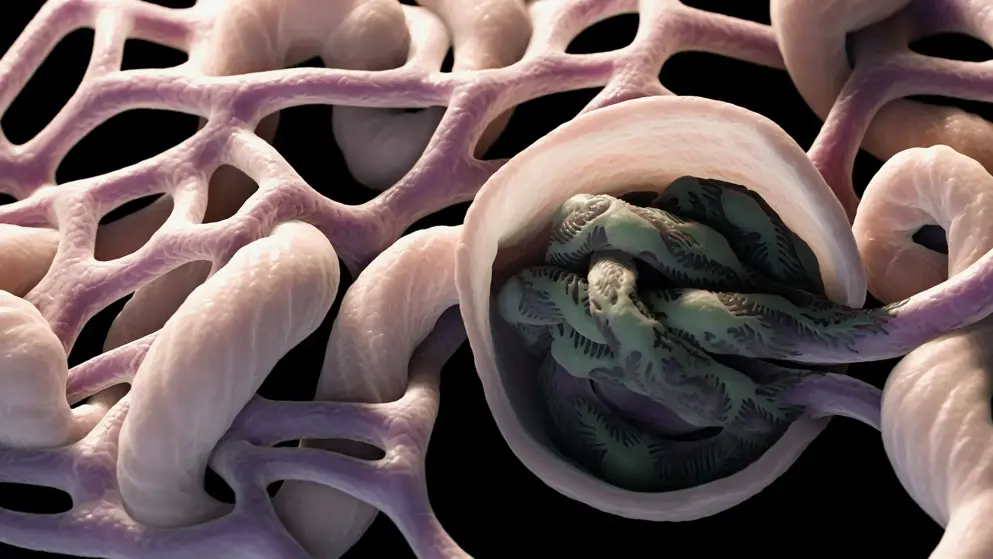
Observations: Defined as a persistent abnormality in kidney structure or function (eg, glomerular filtration rate [GFR] <60 mL/min/1.73 m2 or albuminuria ≥30 mg per 24 hours) for more than 3 months, CKD affects 8% to 16% of the population worldwide. In developed countries, CKD is most commonly attributed to diabetes and hypertension. However, less than 5% of patients with early CKD report awareness of their disease. Among individuals diagnosed as having CKD, staging and new risk assessment tools that incorporate GFR and albuminuria can help guide treatment, monitoring, and referral strategies. Optimal management of CKD includes cardiovascular risk reduction (eg, statins and blood pressure management), treatment of albuminuria (eg, angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers), avoidance of potential nephrotoxins (eg, nonsteroidal anti-inflammatory drugs), and adjustments to drug dosing (eg, many antibiotics and oral hypoglycemic agents). Patients also require monitoring for complications of CKD, such as hyperkalemia, metabolic acidosis, hyperphosphatemia, vitamin D deficiency, secondary hyperparathyroidism, and anemia. Those at high risk of CKD progression (eg, estimated GFR <30 mL/min/1.73 m2, albuminuria ≥300 mg per 24 hours, or rapid decline in estimated GFR) should be promptly referred to a nephrologist.
Conclusions and Relevance: Diagnosis, staging, and appropriate referral of CKD by primary care clinicians are important in reducing the burden of CKD worldwide.
Read abstract on library site Access full article