Thyroid cancer
Thyroid cancer is the most common endocrine malignancy worldwide, with rising incidence rates. This increase is attributed not only to improved awareness and diagnostic sensitivity but also to environmental factors and broader global changes that may contribute to disease occurrence.
What are the main subtypes of thyroid cancer?
Thyroid cancer is typically classified into four main subtypes:
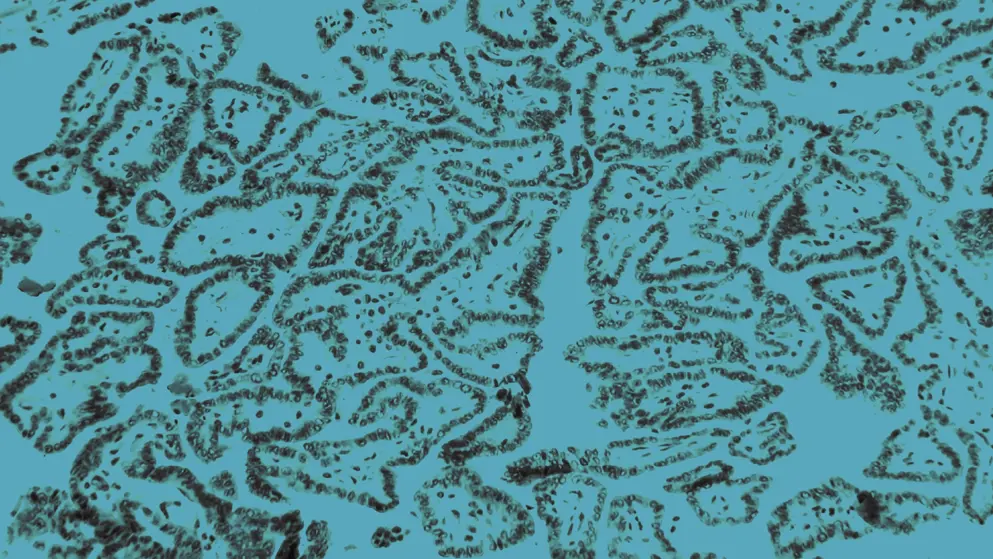
- Papillary thyroid cancer (PTC), the most common type, accounting for ~90% of all cases. It is highly treatable with a good prognosis
- Follicular thyroid cancer (FTC), the second most common type (~20% of cases). Most cases are mild and respond well to treatment, though ~20% may be more aggressive
- Medullary thyroid cancer (MTC), a rare subtype (1–5% of cases) with a poorer prognosis
- Anaplastic thyroid cancer, an extremely rare (~2% of cases) but highly aggressive subtype, responsible for approximately 50% of thyroid cancer–related deaths
What are the risk factors for thyroid cancer?
Risk factors for thyroid cancer include both modifiable and unmodifiable elements:
- Modifiable: Obesity, smoking, heavy alcohol consumption, physical inactivity, and exposure to radiation or environmental pollutants (e.g., heavy metals, endocrine-disruptors)
- Unmodifiable: Female sex, genetic predisposition (e.g., RET, BRAF, RAS mutations), and preexisting benign thyroid conditions, including hyperthyroidism and goiter
What are the symptoms of thyroid cancer?
Symptoms of thyroid cancer include hoarseness, numbness, and a visible lump in the neck. Sleep disturbances, fatigue, and emotional distress are common, with over 30% of patients reporting anxiety and depression.
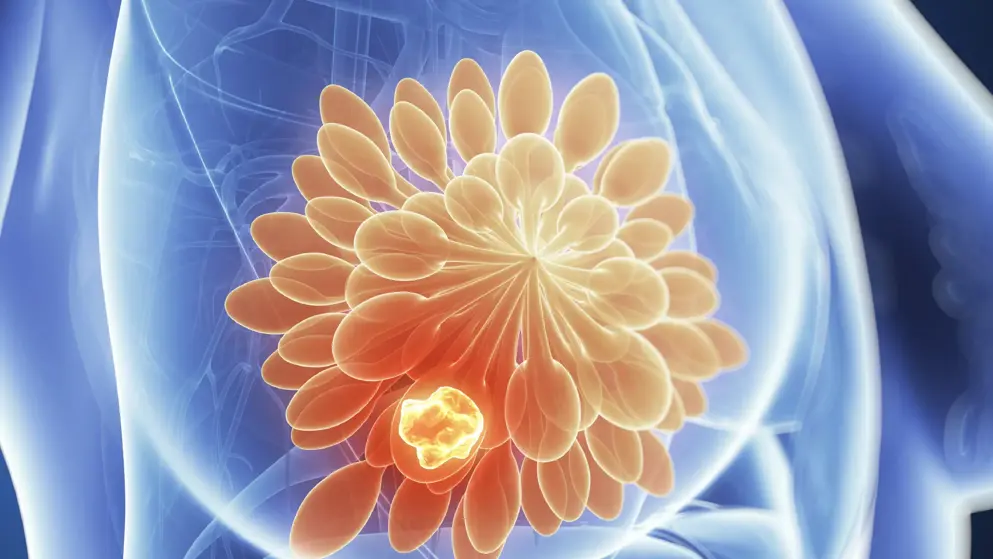
How is thyroid cancer diagnosed?
Approximately half of thyroid cancer cases are discovered incidentally during imaging for unrelated conditions. Diagnosis typically involves physical examination, ultrasound, and fine-needle aspiration biopsy. Molecular testing and advanced imaging techniques like PET/MRI help determine tumor type and extent.
Developed by EPG Health for Medthority, independently of any sponsor.
ASCO 2024 A high-level overview
From ASCO 2024, read Dr Ben Gallarda’s overview of ASCO’s commitment to palliative care, artificial intelligence, and coordination with organizations.
How can poor-quality clinical trials impact clinical decision-making?
Explore why a cautious approach is warranted when interpreting trial results.
Related news and insights
Related Guidelines
References
- NHS (2019). Available at: https://www.nhs.uk/conditions/thyroid-cancer/ (Accessed June 2021).
- Khan YS, Farhana A (2021). Thyroid gland. In: StatPearls [Internet]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK551659/ - :~:text=Thyroid%20cancer%3A%20Thyroid%20carcinomas%20arise,compression%2C%20displaces%20the%20adjacent%20structures. (Accessed June 2021).
- Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet. 2016;388:2783–2759.
- Shikha S, Tulla K, Maker AV, Burman KD, Prabhakar BS. Therapeutic advances in anaplastic thyroid cancer: a current perspective. Molecular Cancer. 2018;17:1–14.
- Moley JF. Medullary Thyroid Carcinoma: Management of Lymph Node Metastases. J Natl Compr Canc Netw. 2010;8:549–556.
- Taccaliti A, Silvetti F, Palmonella G, Boscaro M. Genetic Alterations in Medullary Thyroid Cancer: Diagnostic and Prognostic Markers. Curr Genomics. 2011;12:618–625.
- Zhou X, Zheng Z, Chen C, Zhao B, Cao H, Li T et al. Clinical characteristics and prognostic factors of Hurthle cell carcinoma: a population based study. BMC Cancer. 2020;20:1–9.
- Solomon JP, Benayed R, Hechtman JF, Ladanyi M. Identifying patients with NTRK fusion cancer. Ann Oncol. 2019;30:816–822.
- Viola D, Valerio L, Molinaro E, Agate L, Bottici V, Biagini A et al. Treatment of advanced thyroid cancer with targeted therapies: ten years of experience. Endocrine-Related Cancer. 2016;23:185–205.