Polycystic kidney disease
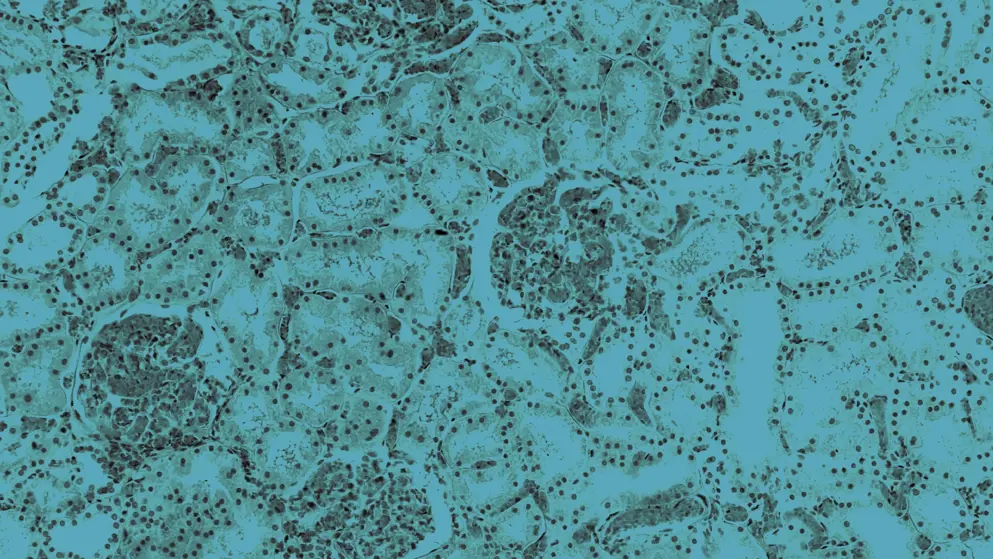
Polycystic kidney disease (PKD) remains a major cause of kidney failure and significantly impacts patient quality of life. There are two main forms:
- Autosomal dominant PKD (ADPKD) affects around 1 in 1,000 people, accounts for 90% of cases, usually presents in adulthood, and progresses slowly
- Autosomal recessive PKD (ARPKD) is rare (1 in 25,000), presents in infancy or early childhood, and is more severe with a rapidly progressive course
In both forms, cyst growth compresses surrounding tissue, driving inflammation and fibrosis. Patients experience back or side pain, hematuria, hypertension, and recurrent urinary tract infections.
How is PKD diagnosed?
PKD is diagnosed using age-specific imaging criteria. Ultrasound offers a reliable, accessible first step, while magnetic resonance imaging (MRI) detects smaller cysts and tracks disease progression. Genetic testing supports diagnosis when imaging is inconclusive or atypical.
What are the most common extrarenal manifestations of PKD?
Common extrarenal manifestations of PKD include liver cysts, intracranial aneurysms, mitral valve prolapse, and cysts in the pancreas, seminal vesicles, and arachnoid membrane.
What factors influence disease severity and progression in PKD?
Poor prognostic factors in ADPKD include:
- Sex – ADPKD tends to be more severe in males
- Genotype – truncating PKD1 variants are linked to faster progression
- Early clinical features – diagnosis before age 30, hematuria before age 30, hypertension before age 35 years
- Metabolic and vascular factors – hyperlipidemia, high body mass index, high urine sodium excretion, lower kidney blood flow, lower serum high-density lipoprotein cholesterol
- Large total kidney volume
Several factors are linked to more severe disease and earlier dialysis in ARPKD:
- Oligohydramnios
- Anhydramnios
- Enlarged kidneys
- Kidney cysts visible on prenatal imaging
- Presence of two truncating (null) PKHD1 variants
Developed by EPG Health for Medthority, independently of any sponsor.