Coagulopathy and bleeding disorders
Coagulopathy presents a complex clinical challenge, encompassing both bleeding and thrombotic disorders that disrupt the body’s clotting mechanisms. Despite advances in diagnosis and treatment, generating scientific evidence to advance care for patients with coagulopathies remains challenging because of their low prevalence and heterogeneity of affected populations, including varied patient demographics and symptom severities.
Globally, inherited bleeding disorders may affect over 7.5 million individuals worldwide, with von Willebrand disease being the most common overall. Acquired conditions like cancer-associated thrombosis (CAT) are known to be a major cause of morbidity and mortality. Rapid recognition and targeted management improve outcomes.
What are the types of coagulopathy?
Coagulopathies are broadly classified as:
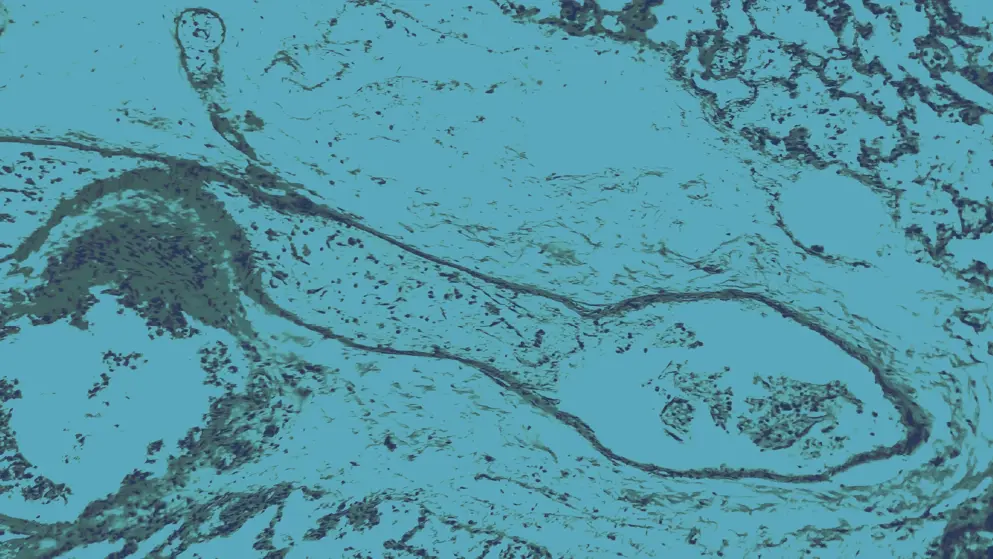
- Bleeding disorders: Inherited (e.g., hemophilia A/B, von Willebrand disease) and acquired (e.g., liver disease, vitamin K deficiency, disseminated intravascular coagulation [DIC], arteriovenous malformations)
- Thrombotic disorders: Inherited (e.g., factor V Leiden, prothrombin gene mutation) and acquired (e.g., antiphospholipid syndrome, DIC, CAT, infection, atherosclerosis)
How are coagulation disorders diagnosed?
Coagulopathies are diagnosed based on clinical presentation and risk factors. Initial tests assess blood clotting ability and fibrinogen function and include:
- Platelet count: Screens for thrombocytopenia
- Coagulation screens: E.g., prothrombin time, partial prothromboplastin time, and fibrinogen tests, which assess clotting factor deficiencies and pathway defects
- Specialist assays: Factor levels, von Willebrand factor, Clauss fibrinogen, viscoelastic tests such as rotational thromboelastometry (ROTEM) and thromboelastography (TEG)
Genetic testing for inherited disorders is under investigation to enable early diagnosis and targeted therapy.
What treatments are available for coagulation disorders?
Management of coagulopathies is tailored to the underlying disorder:
- Bleeding: Factor replacements, desmopressin, vitamin K supplements, oral contraceptives, antifibrinolytics
- Thrombosis: Anticoagulants (heparin, direct oral anticoagulants), surgery to remove clots, and stent insertion
The benefits and risks of each agent should be assessed using clinical judgment in order to individualize therapy based on the treatment risk, patient history, age, renal function, and concomitant medications.
Developed by EPG Health for Medthority, independently of any sponsor.

