AL amyloidosis
Systemic amyloid light-chain (AL) amyloidosis, also known as primary amyloidosis, is a potentially life-threatening rare plasma cell disorder caused by abnormal immunoglobulin light-chain proteins produced by plasma cells in the bone marrow. These proteins misfold and form amyloid fibrils that are deposited in various organs and tissues, causing significant damage.
How prevalent is AL amyloidosis?
An estimated 74,000 people were diagnosed with AL amyloidosis worldwide over the 20 years leading up to 2018, with an average increase of approximately 1,111 cases every 5 years.
What are the common symptoms of AL amyloidosis?
At diagnosis, non-specific symptoms may include fatigue, weight loss, and swelling. As the disease progresses, significant damage can occur to the heart, kidneys, and nervous system, resulting in symptoms such as peripheral neuropathy, shortness of breath, and arrhythmia.
Why is it important to diagnose AL amyloidosis early?
Delayed diagnosis of AL amyloidosis is associated with progressive organ damage and reduced survival, with approximately 25% of patients dying within 6 months of diagnosis, primarily due to advanced cardiac involvement by the time the disease is identified.
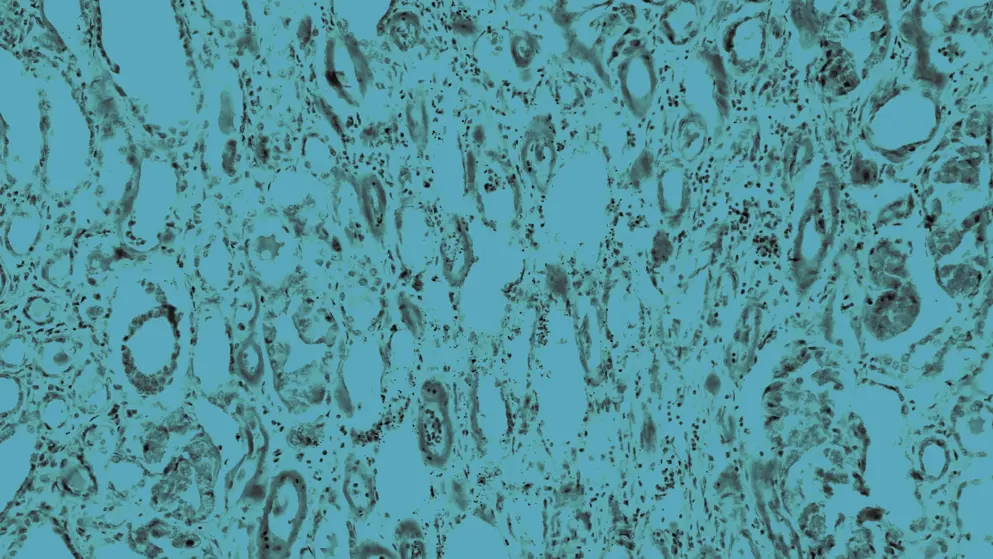
How is AL amyloidosis diagnosed?
Diagnosing AL amyloidosis involves a combination of lab tests, imaging, and biopsies to confirm amyloid deposits and determine their type. Comprehensive testing is essential for accurate identification. Specialized diagnostic techniques, including serum and urine protein electrophoresis, immunofixation, and tissue biopsies (e.g., fat pad, bone marrow biopsy), are crucial. Resource limitations may complicate the diagnostic process.
What are the treatments for AL amyloidosis?
Treatment for AL amyloidosis requires a personalized, multidisciplinary approach aimed at reducing abnormal light chains and managing organ damage. Management strategies may include:
- Chemotherapy
- Autologous stem cell transplantation for eligible patients
- Targeted therapies, such as monoclonal antibodies and proteasome inhibitors
Supportive care may include heart medications and kidney support.
Developed by EPG Health for Medthority, independently of any sponsor.
AL amyloidosis interactive patient journey
Make your own clinical decisions for managing a patient with AL amyloidosis in this interactive patient journey, guided by additional management tips provided by Dr. Shaji Kumar every step of the way.
Related news and insights
Guidelines
References
- Merlini G, Dispenzieri A, Sanchorawala V, Schönland SO, Palladini G, Hawkins PN, et al. Systemic immunoglobulin light chain amyloidosis. Nat Rev Dis Prim. 2018;4(1):38.
- Palladini G, Milani P, Merlini G. Management of AL amyloidosis in 2020. Blood. 2020;136(23):2620–2627.
- Shi J, Guan J, Jiang B, Brenner DA, Del Monte F, Ward JE, et al. Amyloidogenic light chains induce cardiomyocyte contractile dysfunction and apoptosis via a non-canonical p38α MAPK pathway. Pro Nat Acad Sci. 2010;107(9):4188–4193.
- D'Souza A, Osman K, Chase CC, Borham A, Bruno M. The hematologist's role in amyloidosis management: disease awareness, diagnostic workup, and practice patterns. Blood. 2020;136:28–29.
- Palladini G, Merlini G. How I treat AL amyloidosis. Blood. 2022;139(19):2918–2930.
- Merlini G, Seldin DC, Gertz MA. Amyloidosis: pathogenesis and new therapeutic options. J Clin Oncol. 2011;29(14):1924.
- Kastritis E, Leleu X, Arnulf B, Zamagni E, Cibeira MT, Kwok F, et al. Bortezomib, melphalan, and dexamethasone for light-chain amyloidosis. J Clin Oncol. 2020;38(28):3252–3260.
- Dispenzieri A, Kastritis E, Wechalekar AD, Schönland SO, Kim K, Sanchorawala V, et al. A randomized phase 3 study of ixazomib-dexamethasone versus physician’s choice in relapsed or refractory AL amyloidosis. Leukemia. 2022;36(1):225–235.
- Kastritis E, Palladini G, Minnema MC, Wechalekar AD, Jaccard A, Lee HC, et al. Daratumumab-based treatment for immunoglobulin light-chain amyloidosis. New Eng J Med. 2021;385(1):46–58.

