Alpha-1 antitrypsin deficiency
Alpha-1 antitrypsin deficiency (AATD) is a genetic condition linked to serious lung and liver disease. Caused by mutations in the SERPINA1 gene, AATD leads to low or dysfunctional forms of alpha-1 antitrypsin (AAT), a key inhibitor of neutrophil elastase. Insufficient AAT allows unchecked inflammation, causing early-onset emphysema, chronic obstructive pulmonary disease (COPD), and progressive liver damage. Although common among people of European descent, AATD often remains undiagnosed until irreversible organ damage occurs.
Who is most at risk of AATD?
AATD affects all ethnicities but is most common in individuals of Northern European ancestry. The PiZZ genotype carries the highest risk, though other variants (e.g., PiSZ, PiMZ) may also lead to disease, especially when combined with environmental triggers like smoking or alcohol. Family history is a key risk factor, and screening is recommended for relatives of affected individuals.
What causes organ damage in AATD?
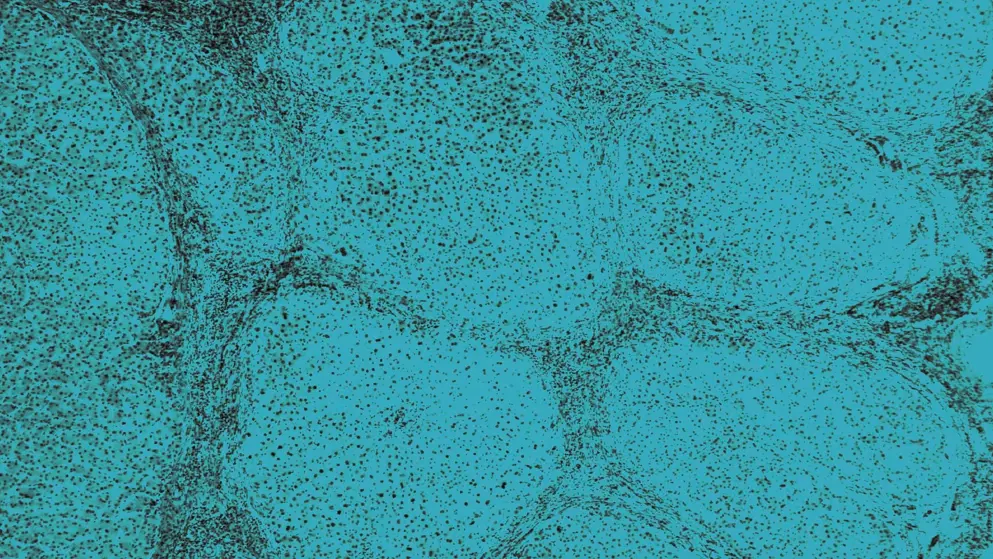
In AATD, mutations in the SERPINA1 gene result in low or misfolded AAT protein. In the lungs, this allows neutrophil elastase to damage alveolar tissue. In the liver, abnormal AAT accumulates in hepatocytes, causing cellular stress and fibrosis. Clinical presentation varies widely, even among individuals with the same genotype.
How does AATD impact quality of life?
Symptoms of AATD, such as breathlessness, fatigue, and recurrent infections, can significantly impact daily functioning. Liver–lung complications may lead to hospitalizations and long-term monitoring. Many patients experience delays in diagnosis, which can affect mental health.
What treatments are available for AATD?
Treatment for AATD depends on organ involvement and genotype. For lung disease, symptom relief includes smoking cessation, bronchodilators, and inhaled corticosteroids. These help improve symptoms and quality of life. Disease-modifying therapy with intravenous AAT may be considered for individuals with severe deficiency genotypes (e.g., PiZZ), though access varies by region and guideline. For liver involvement, regular monitoring is essential to detect progression, and transplantation may be needed in advanced cases. Genotype plays a key role in guiding therapy decisions, and ongoing research is exploring targeted approaches for hepatic disease.
Developed by EPG Health for Medthority, independently of any sponsor.
Listen and learn: AATD podcast series
Earn 1.5 CME credits by listening to this accredited podcast series.
- What is AATD and how does it impact the liver and the lung?
- AATD genotypes involved in liver disease
- Screening, diagnosis, and guideline recommendations for AATD management
- Treatment options for AATD-associated liver disease and current unmet needs