Venous thromboembolism
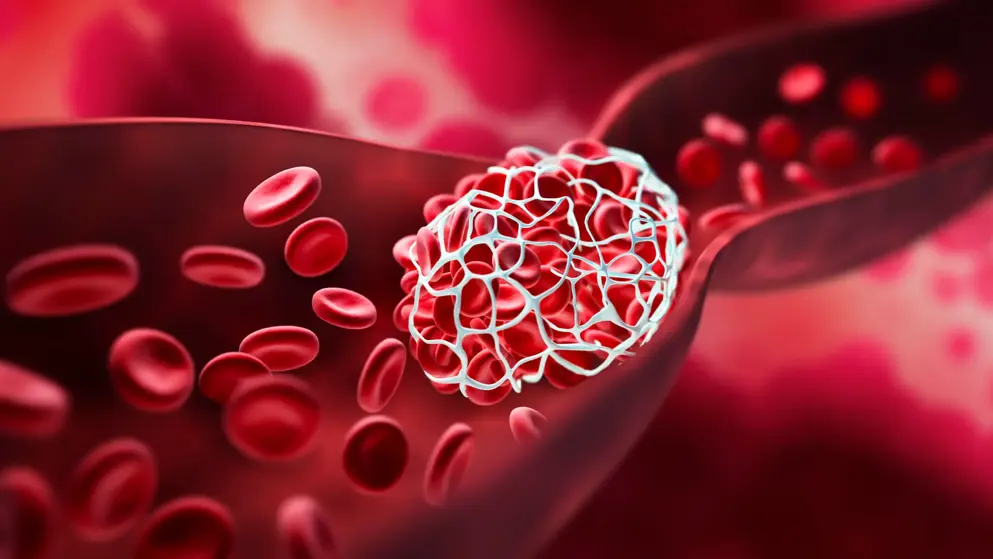
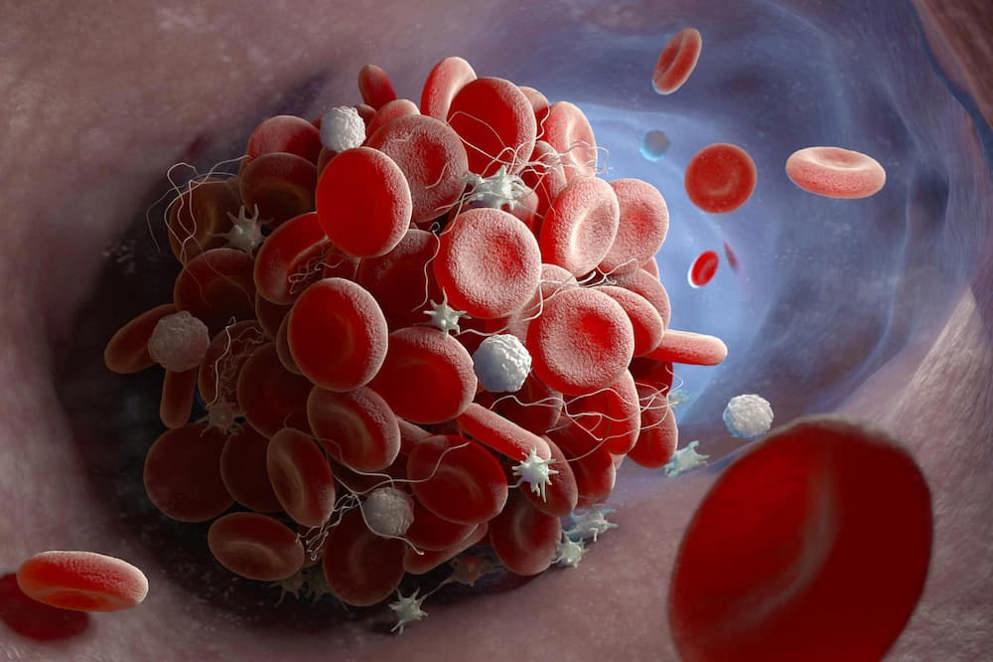
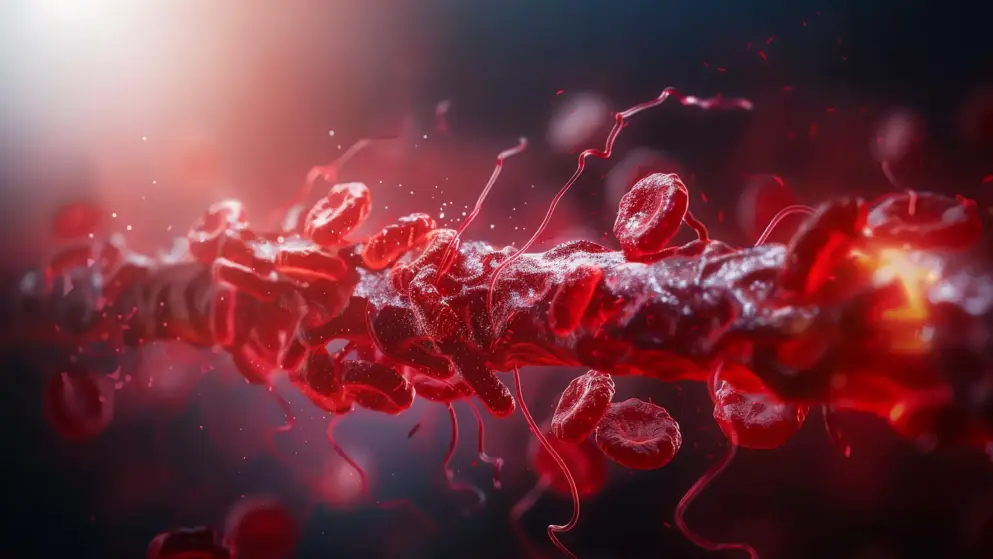
The term venous thromboembolism (VTE) encompasses deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT is the formation of a blood clot in a deep vein, most often in the legs, arms, and pelvis, though other vein involvement can occur. PE occurs when a blood clot, typically originating from a deep vein in the leg or pelvis, breaks loose, travels through the bloodstream, and lodges in the arteries of the lungs, obstructing blood flow.
What is the global prevalence of VTE?
VTE affects approximately 1 in 12 people over the course of their lifetime.
What are the risk factors for VTE?
There are numerous factors that may increase the risk of developing a blood clot. They include, but are not limited to, surgery, heart conditions, chronic conditions such as high blood pressure or diabetes, infections, multiple traumas, cancer, age, obesity, smoking, immobility, and a family history of VTE.
What are the most common symptoms of VTE?
The most common presentation of DVT includes leg pain or tenderness of the thigh or calf, edema, skin that feels warm to the touch, and reddish skin discoloration.
The most common presentation of PE includes sudden difficulty breathing, rapid breathing, chest pain, increased heart rate, light headedness, and coughing (with or without blood).
What treatment options are available for VTE?
VTE is often preventable; therefore, a proactive approach using risk assessment is advised. When VTE does occur, anticoagulants are used to prevent clots from continuing to form. Thrombolytic therapy may be used in people with PE accompanied by hemodynamic instability or in cases of severe DVT. Surgical thrombectomy may be required in complex cases.
Developed by EPG Health for Medthority, independently of any sponsor.
Browse older resources
ASCO: Treatment selection in Ph+ ALL
Join experts Elias Jabbour, Hagop Kantarjian and Nicholas Short at this symposium, where they discuss the frontline treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL).
Cancer-Associated Thrombosis
Cancer‐associated thrombosis (CAT) is a frequent, potentially life‐threatening event that complicates cancer management. New treatments, including DOACs, are now recommended for CAT
Fluid Management Learning Zone
Welcome to the Fluid Management Learning Zone. In this Learning Zone we provide an overview of fluid management, including albumin for sepsis and septic shock, guidelines for fluid management in liver cirrhosis and fluid management in cardiac surgery.
Venous Thromboembolism (VTE) Learning Zone
Venous thromboembolism (VTE) includes deep vein thrombosis (DVT) and pulmonary embolism (PE), and is associated with long-term complications, disability and significant mortality.
Bleeding risk after DOAC initiation
From ISTH 2024, read results from a study investigating time to bleeding after DOAC initiation for venous thromboembolism and atrial fibrillation.