Arrhythmia
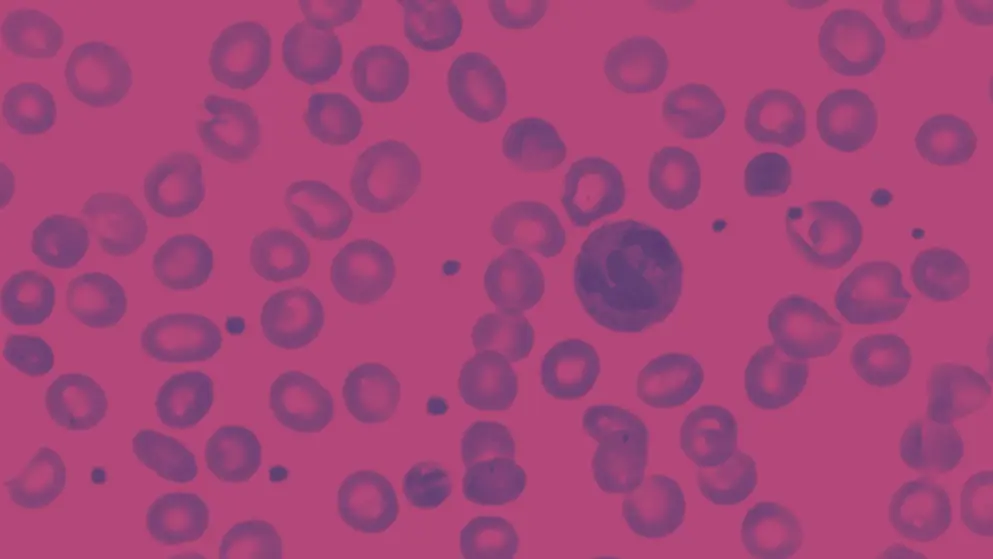
Arrhythmia refers to an irregular heartbeat caused by abnormal electrical impulses in the heart, leading to tachycardia, bradycardia, or erratic rhythms. Symptoms may include palpitations, dizziness, and fatigue. In some cases, arrhythmias can result in severe complications, such as stroke, blood clotting, heart failure, and sudden cardiac death. Common types include atrial fibrillation, atrial flutter, supraventricular tachycardia, ventricular fibrillation, and ventricular tachycardia.
What triggers arrhythmia?
Arrhythmias are often triggered by disruptions in the heart’s electrical conduction system. These may stem from structural heart disease, electrolyte imbalances, or autonomic nervous system instability. Common triggers include myocardial infarction, cardiomyopathy, thyroid disorders, stimulant use (e.g., caffeine, alcohol, certain drugs), and some medications. Sleep apnea and inherited channelopathies, such as long QT syndrome, are also recognized contributors.
What are the challenges in diagnosing arrhythmia?
Diagnosis is complicated by the often intermittent and non-specific nature of arrhythmia symptoms. Many arrhythmias are paroxysmal, making them hard to detect with a standard ECG. Patients may present with vague symptoms like fatigue, dizziness, or palpitations, which can overlap with other conditions. Silent arrhythmias, particularly asymptomatic atrial fibrillation, might remain undetected until complications such as stroke occur. Holter monitors, event recorders, and electrophysiologic studies can aid diagnosis but often require prolonged monitoring and patient cooperation. Comorbidities, including sleep apnea and thyroid disorders, may further obscure the clinical picture.
What treatment options are available for arrhythmia?
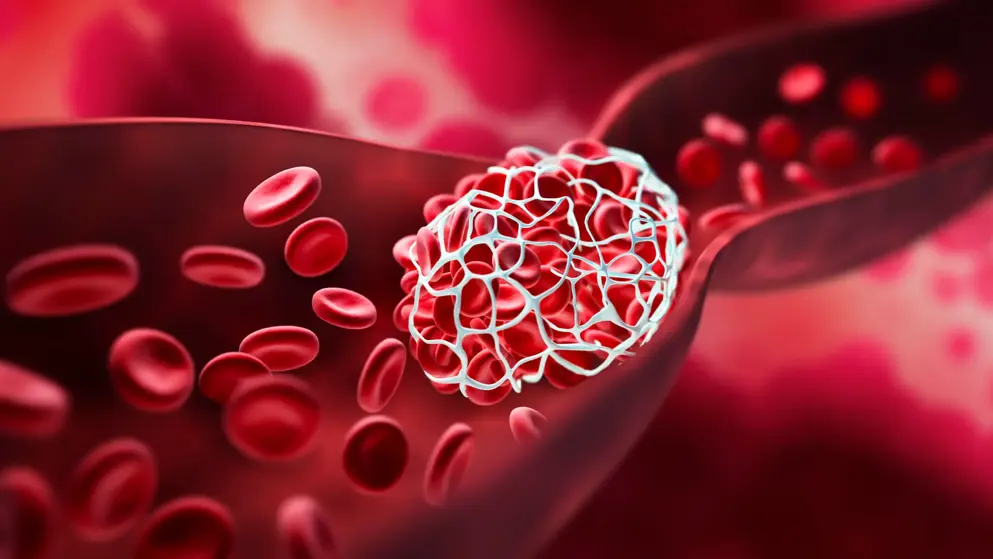
First-line management typically involves antiarrhythmic agents and anticoagulants. Additional options vary by arrhythmia type and include ischemic preconditioning, cardioversion, catheter ablation, implantable cardioverter-defibrillators, and cardiac resynchronization therapy.
Developed by EPG Health for Medthority, independently of any sponsor.
Browse older resources
Anticoagulation Therapy for Stroke Prevention
Explore the latest guidelines for the diagnosis and management of atrial fibrillation. Learn more about AF as a risk factor for stroke, AF screening, diagnosis and treatment.
Fluid Management Learning Zone
Welcome to the Fluid Management Learning Zone. In this Learning Zone we provide an overview of fluid management, including albumin for sepsis and septic shock, guidelines for fluid management in liver cirrhosis and fluid management in cardiac surgery.
Lipid Management in ASCVD Learning Zone
Atherosclerotic cardiovascular disease (ASCVD) is a major cause of morbidity and mortality despite advanced in lipid-lowering treatment and management.
Apple’s Afib history FDA qualified
Can it reliably estimate AFib burden, and what are its key limitations?
Can wearables reliably detect signs of atrial fibrillation? FDA says yes to Fitbit
FDA clearance for passive heart rhythm monitoring via smartwatches has the potential to increase passive detection of atrial fibrillation. But what concerns still exist about this new technology and how will it integrate into standard cardiology care?