Innovations in cancer therapy: antibody-drug conjugates
Article by Sharmini Rajanayagam BSc (Hons), PhD; Senior Medical Writer at EPG Health
Anti-HER2 therapy
The monoclonal antibody trastuzumab was among the first targeted cancer therapies and the first human epidermal growth factor receptor 2 (HER2) inhibitor approved for the treatment of breast cancer1,2. The development of trastuzumab was considered a breakthrough in the treatment of HER2+ breast cancers, as it was associated with significantly improved survival outcomes for a breast cancer subtype with a bleak outlook1,2. The downside, though, is that trastuzumab is effective only in patients whose tumours overexpress HER2 at high levels, sufficient to register an immunohistochemistry (IHC) score of at least 3+ or IHC score of 2+ with gene amplification of ≥2 copies on fluorescence in situ hybridisation (FISH)1,3. This excludes about 60% of patients whose tumours express HER2 at levels below this threshold4.
For the purpose of determining eligibility for anti-HER2 therapy, HER2+ status was defined as an IHC score of 3+ or IHC 2+ with gene amplification of ≥2 copies on FISH3,5. IHC scores of 1+ or 2+ were not considered clinically relevant, given that they are typically unresponsive to anti-HER2 therapy, and tumours with these scores were relegated to HER2− status3. Clearly, breast cancers deemed HER2− by current guidelines are not necessarily devoid of these receptors. Indeed, more than half of metastatic HER2− breast cancers do express HER2 but at levels that evade standard anti-HER2 therapy4.
The current notion of HER2 status as binary, either positive or negative, is now undergoing a paradigm shift with the recognition of a third option – ‘HER2-low’ – found to be a viable treatment target of a new class of drugs1,5. HER2-low encompasses tumours with IHC scores of 1+ and 2+ without gene amplification, which are unresponsive to standard anti-HER2 therapy but recently found to be sensitive to the antibody-drug conjugates (ADCs) trastuzumab deruxtecan (T-DXd) and trastuzumab duocarmazine4–6.
Antibody-drug conjugates
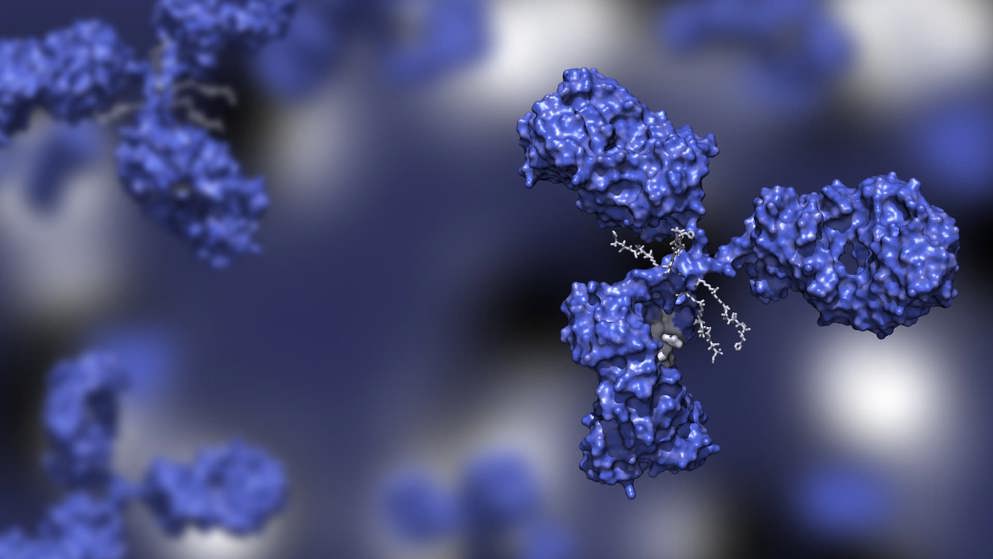
ADCs are a recent innovation in cancer therapy and provide a unique means of fine-tuning the delivery of cytotoxic agents to tumour cells7–9. ADCs consist of a monoclonal antibody, such as trastuzumab, bound to a chemotherapy drug via cleavable linker peptides (Figure 1).
Figure 1. Antibody-drug conjugate. Image adapted under CC BY-SA 4.0
The antibody binds to the target antigen on the tumour cell and is then internalised in the cell where the linker proteins are cleaved to release a cytotoxic payload7–9. In this way, ADCs are capable of selectively delivering cytotoxic agents to specific cancer cell targets while minimising exposure to non-cancer cells7–9. An additional key feature of T-DXd and trastuzumab duocarmazine is their ability to exert a so-called ‘bystander’ effect on neighbouring tumour cells, regardless of whether they express HER210. Preclinical studies have shown that T-DXd has anti-tumour activity in a variety of tumour types, including those expressing low levels of HER211.
The ability of T-DXd and trastuzumab duocarmazine to selectively deliver potent cytotoxic payloads to HER2+ tumour cells, together with their unique bystander effect, broadens the reach of these agents to patients with HER2-low tumours, who are ineligible for standard anti-HER2 therapy
Trastuzumab deruxtecan
T-DXd is an ADC that consists of trastuzumab bound to the topoisomerase 1 inhibitor deruxtecan, an exatecan derivative. It was designed to deliver the potent topoisomerase 1 inhibitor to HER2-expressing cells4,10. The linker peptides are stable in plasma but cleaved by lysosomal cathepsins, which are upregulated in cancer cells11. Once released in the tumour cell, the topoisomerase 1 inhibitor, designed to be cell permeable, can exert its bystander effect to eliminate surrounding tumour cells, whether they express HER2 or not10.
In mid-2022, the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) approved the use of T-DXd for treatment of HER2+ metastatic breast cancer12,13. Approval was based on the results of the DESTINY-Breast03 trial, which compared T-DXd with trastuzumab emtansine (T-DM1), an earlier version of an ADC combining trastuzumab with the cytotoxic anti-microtubule agent DM114. DESTINY-Breast03 showed that the risk of disease progression was significantly lower in patients with HER2+ metastatic breast cancer who received T-DXd than in those who received T-DM114.
DESTINY-Breast04 trial
Given the unique bystander effect of T-DXd, a subsequent clinical trial, DESTINY-Breast04, was undertaken to determine whether T-DXd would in fact prove effective against HER2-low breast cancer4. DESTINY-Breast04 was a randomised, multicentre, open-label, phase 3 trial that evaluated the efficacy and safety of T-DXd, compared with treatment of physician’s choice (TPC), in patients with HER2-low metastatic breast cancer4. Patients who had been treated previously with one or two lines of chemotherapy in the metastatic setting were recruited to the study. TPC included capecitabine, eribulin, gemcitabine, paclitaxel or nab-paclitaxel15. At 18.4 months follow up, progression-free survival was significantly greater in patients on T-DXd than those on TPC (9.9 months vs 5.1 months; hazard ratio [HR] 0.50; 95% confidence intervals [CI] 0.40, 0.63; P<0.0001). T-DXd also increased overall survival (23.4 months vs 16.8 months; HR 0.64; 95% CI 0.49, 0.84; P=0.0010). This amounts to an impressive 50% reduction in the risk of disease progression and a 36% reduction in the risk of death4.
The incidence of adverse events was similar in the two treatment groups4. The most common side effects of T-DXd were nausea and neutropenia, but these could be managed with medication. An important risk associated with T-DXd treatment is interstitial lung disease, which occurred in 12% of patients in the DESTINY-Breast04 trial. Patients treated with T-DXd, therefore, require careful monitoring to ensure early detection and intervention to prevent or minimise serious outcomes4.
In August 2022, only two months after completion of DESTINY-Breast04, the FDA approved the use of T-DXd for the treatment of metastatic breast cancer in patients with the newly identified designation of HER2-low
Development of the anti-HER2 monoclonal antibody trastuzumab was rightly considered a breakthrough in the treatment of HER2+ breast cancer. The development of ADCs, including T-DXd, may well be considered a sophisticated advance in drug design for targeted cancer therapy.
Learn more about cancer treatments
References
- Eiger D, Agostinetto E, Saúde-Conde R, de Azambuja E. The Exciting New Field of HER2-Low Breast Cancer Treatment. Cancers (Basel). 2021;13(5).
- Mendes D, Alves C, Afonso N, Cardoso F, Passos-Coelho JL, Costa L, et al. The benefit of HER2-targeted therapies on overall survival of patients with metastatic HER2-positive breast cancer – a systematic review. Breast Cancer Res. 2015;17(1):140.
- Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol. 2018;36(20):2105-2122.
- Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. N Eng J Med. 2022;387(1):9-20.
- Miglietta F, Griguolo G, Bottosso M, Giarratano T, Lo Mele M, Fassan M, et al. HER2-low-positive breast cancer: evolution from primary tumor to residual disease after neoadjuvant treatment. npj Breast Cancer. 2022;8(1):66.
- Gampenrieder SP, Rinnerthaler G, Tinchon C, Petzer A, Balic M, Heibl S, et al. Landscape of HER2-low metastatic breast cancer (MBC): results from the Austrian AGMT_MBC-Registry. Breast Cancer Res. 2021;23(1):112.
- Hafeez U, Parakh S, Gan HK, Scott AM. Antibody-Drug Conjugates for Cancer Therapy. Molecules. 2020;25(20).
- Pettinato MC. Introduction to Antibody-Drug Conjugates. Antibodies (Basel). 2021;10(4).
- Walko CM, West H. Antibody Drug Conjugates for Cancer Treatment. JAMA Oncology. 2019;5(11):1648-1648.
- Modi S, Park H, Murthy RK, Iwata H, Tamura K, Tsurutani J, et al. Antitumor Activity and Safety of Trastuzumab Deruxtecan in Patients With HER2-Low-Expressing Advanced Breast Cancer: Results From a Phase Ib Study. J Clin Oncol. 2020;38(17):1887-1896.
- Ogitani Y, Aida T, Hagihara K, Yamaguchi J, Ishii C, Harada N, et al. DS-8201a, A Novel HER2-Targeting ADC with a Novel DNA Topoisomerase I Inhibitor, Demonstrates a Promising Antitumor Efficacy with Differentiation from T-DM1. Clin Cancer Res. 2016;22(20):5097-5108.
- FDA. @US_FDA. FDA grants regular approval to fam-trastuzumab deruxtecan-nxki for breast cancer | FDA. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-regular-approval-fam-trastuzumab-deruxtecan-nxki-breast-cancer.
- European Medicines Agency. Enhertu: Summary of Product Characteristics. https://www.ema.europa.eu/en/documents/product-information/enhertu-epar-product-information_en.pdf.
- Cortés J, Kim S-B, Chung W-P, Im S-A, Park YH, Hegg R, et al. Trastuzumab Deruxtecan versus Trastuzumab Emtansine for Breast Cancer. N Eng J Med. 2022;386(12):1143-1154.
- Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab deruxtecan (T-DXd) versus treatment of physician’s choice (TPC) in patients (pts) with HER2-low unresectable and/or metastatic breast cancer (mBC): Results of DESTINY-Breast04, a randomized, phase 3 study. J Clin Oncol. 2022;40(17_suppl):LBA3-LBA3.
of interest
are looking at
saved
next event
