Cancer immunotherapies
Cancer immunotherapies: Dr Marshall Pearce
It was the winner of the 1908 Nobel prize for medicine, Paul Ehrlich, who is first credited with discussing the concept of a “magic bullet”, able to target specific cells without damaging healthy tissue. With the advent of immunotherapy, as well as antibody-drug conjugates, we are beginning to realise this vision.
Relative to the doses of chemotherapeutic agents that are tolerated in patients, the immune system is an immensely powerful tool if used appropriately. When the immune system recognises an antigen as ‘foreign’, it has the potential to ramp up maturation of T cells until the target cells are entirely destroyed, repeating the process more quickly and efficiently should the antigen appear again. The theory behind immunotherapy is to modulate the immune system so it recognises and attacks malignant cells – in practice however, part of the reason malignant cells are able to proliferate is because they have signalling pathways that deactivate those defences.
To stimulate recognition, there are various options available or under investigation. These range from passive, such as the cytokines interleukin-2 and interferon-alpha (used in some haematological malignancies), to active checkpoint inhibitors and therapeutic vaccines which are predominantly useful against tumours expressing specific mutations.
Monoclonal antibodies
Humanised monoclonal antibodies can act to block cellular signalling pathways that are part of tumour growth. Bevacizumab (Avastin®) blocks vascular endothelial growth factor (VEGF) – one of the growth factors responsible for angiogenesis – limiting the potential expansion of tumours, and is used in several solid cancers. Trastuzumab (Herceptin®), binds to the overexpressed HER2 receptors which are a key driver of cell division, arresting that process and reducing proliferation. More relevant to this particular discussion are those monoclonal antibodies which can bind to a target and help to flag cancerous cells to the immune system. In theory at least, bavituximab fulfils that role, and remains in preclinical trials for liver cancer, non-small cell lung cancer (NSCLC) and rectal cancer; however, previous phase III trials did not demonstrate a benefit in lung cancer.
Figure 1. A representation of two targets for monoclonal antibodies. Drug molecules are able to either block the receptors that, if stimulated, promote angiogenesis or cell division; or bind to the signalling molecules, preventing them from stimulating these pathways.
Checkpoint inhibitors
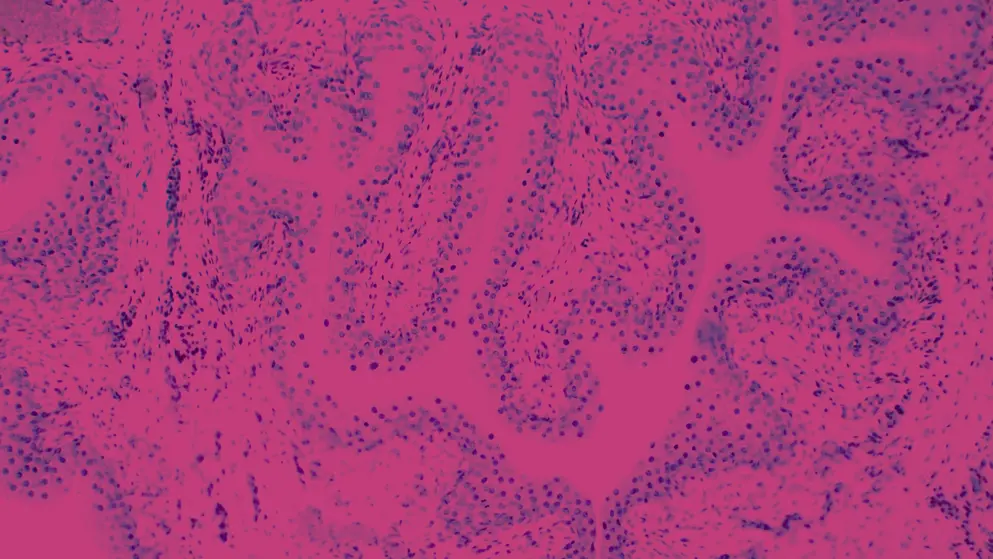
This class of drugs is based around the discovery of several “immune checkpoints”, which are molecular signalling pathways exploited by cancers that prevent T-cell activation – stopping the immune system from destroying an abnormal cell. The drugs investigated for this purpose have shown very positive results to date in some patients, but have proven to be of little benefit in others; the future of this class of drugs may lie in discovering biomarkers that will indicate efficacy prior to initiating treatment.
The first of these pathways, mediated by an antigen named CTLA-4, was discovered in 1987. It functions as an ‘off’ switch on T cells, preventing them from mounting a response to a foreign cell. Bypassing this response has led to the development of ipilimumab (Yervoy®), approved by the FDA and EMA for the treatment of metastatic melanoma, and the in-development tremelimumab.
Programmed Death 1 (PD-1) plays an important role in malignant cells being able to limit the activity of T cells in later stages of tumour growth. Blocking these interactions has shown benefit in several clinical trials, and has led to the development of pembrolizumab (Keytruda®) and nivolumab (Opdivo®). Pembrolizumab has been approved by the FDA and EMA for non-small cell lung cancer (NSCLC), head and neck cancers, while nivolimumab is approved for use in metastatic melanoma, metastatic NSCLC, renal cell carcinoma, Hodgkin lymphoma, squamous cell carcinomas of the head and neck, and urothelial carcinoma by the FDA and EMA.
Figure 2. A diagrammatic representation of the role of a PD-1 inhibitor. The tumour cell is able to deactivate the T cell, preventing it from initiating cell death; however with a PD-1 inhibitor able to blockade the receptor pathway, the tumour cell can be recognised and destroyed.
Therapeutic cancer vaccines
In contrast to a standard prophylactic vaccine against infection, therapeutic cancer vaccines are not preventative, but encourage the immune system to recognise cancers as a viable target. While there are numerous treatments in development, there is only one that is currently approved for use. Treatment with sipuleucel-T (Provenge®) involves harvesting antigen-presenting cells from a patient, artificially mounting an antigen on them, then reintroducing them – where they will activate T cells to recognise malignant cells (figure 3).
Figure 3. The process of treatment with sipuleucel-T. Adapted from Di Lorenzo et al., 2011.
Randomised controlled trials have demonstrated an overall survival benefit for sipuleucel-T over standard treatment, although the effect did not reach statistical significance in one of the trials. It is currently only licensed in the USA, indicated for the treatment of asymptomatic or minimally symptomatic metastatic castrate resistant (hormone refractory) prostate cancer.
Cytokines
The small proteins responsible for intercellular signalling at close ranges, cytokine-based therapies are well established in the treatment of several cancers. Interferon-alpha has been demonstrated to have a number of negative effects on malignant cells, while also boosting differentiation and activity of host immune cells. Interleukin-2 induces proliferation and differentiation of several types of T cells, and can stimulate release of tumour necrosis factors.
Areas in development
Oncolytic virus therapy is one of several potential options for the future of immunotherapy. The theory is not new – find a virus that selectively damages malignant cells; tumour regression has been observed frequently during a viral infection. Dating back to the late 1940s, numerous viruses have been trialled on patients with cancer, but the inability to adequately control the virulence discounted these efforts. More recent techniques have enabled engineered viruses to be used; talimogene laherparepvec (Imlygic®) is the first to be approved by both the FDA and EMA for limited use in patients with unresectable melanoma. Its application is still limited at present, and it has yet to demonstrate a clear overall survival benefit. Other treatments remain in development.
Adoptive T-cell transfer is another interesting therapeutic area in development. The goal is to extract lymphocytes, culture and manipulate them to induce recognition of a tumour antigen by exposing them to resected malignant cells, then reinfuse them. There are not yet any approved therapies using this basis, although there are several in development.
Practical application
There are anecdotal success stories which have surrounded immunotherapies since their inception, and the success of these treatments in some patients is beyond dispute; dramatic recoveries from the brink of death are frequently described. When looking at the wider spectrum of how we think of disease, randomised trials demonstrating a few months of increased overall survival often make the economic case for newer immunotherapeutic agents difficult. A possible solution to this problem is to have better methods to determine which patients will benefit, and to maximise effect in marginal cases. To that end, much research is being done into the use of biomarkers as indicators of success.
Another issue being investigated is “hot” versus “cold” tumours. In this context, hot tumours are those with many aberrant proteins which are detectable by the host’s immune system, and checkpoint inhibitors have proven markedly useful in these cases. Determining whether the immune system can be primed in the case of cold tumours by killing some cancer cells, allowing dissemination of those proteins and then initiating checkpoint inhibitor therapy is also under investigation.
The tolerability of immunotherapy is another question to be addressed as the availability of these drugs grows; the side-effects are diverse, and are different for every therapy that has been developed to date.
Future potential
Immunotherapy continues to demonstrate that it is one of the key areas of interest for the future of medicine – named “breakthrough of the year” in 2013 by Science, it has demonstrated huge potential, although lack of universal application has tempered its success to date.
References and further reading
Bellmunt J, Powles T, Vogelzang NJ. A review on the evolution of PD-1/PD-L1 immunotherapy for bladder cancer: The future is now. Cancer Treat Rev. 2017 Mar;54:58–67.
Di Lorenzo G, Buonerba C, Kantoff PW. Immunotherapy for the treatment of prostate cancer. Nat Rev Clin Oncol. 2011 May 24;8(9):551–61.
Hirbod-Mobarakeh A, Gordan HA, Zahiri Z, Mirshahvalad M, Hosseinverdi S, Rini B, et al. Specific immunotherapy in renal cancer: a systematic review. Ther Adv Urol. 2017 Feb;9(2):45–58.
Jain A, Chia WK, Toh HC. Immunotherapy for nasopharyngeal cancer-a review. Chin Clin Oncol. 2016 Apr;5(2):22.
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010 Jul 29;363(5):411–22.
Li Y, Li F, Jiang F, Lv X, Zhang R, Lu A, et al. A mini-review for cancer immunotherapy: molecular understanding of pd-1/pd-l1 pathway & translational blockade of immune checkpoints. Int J Mol Sci. 2016 Jul 18;17(7).
Mittendorf EA, Peoples GE. Injecting Hope–A Review of Breast Cancer Vaccines. Oncology (Williston Park). 2016 May;30(5):475–81, 485.
Tsiatas M, Mountzios G, Curigliano G. Future perspectives in cancer immunotherapy. Ann Transl Med. 2016 Jul;4(14):273.