Supportive care in oncology Learning Zone
Transcript: Neurological and muscular side effects
Dr Gary Lyman
All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
The neurologic effects of cancer therapies, cancer-related neurotoxicities are, as you mentioned, quite broad. They include cognitive impairment, what many are calling "chemo brain".
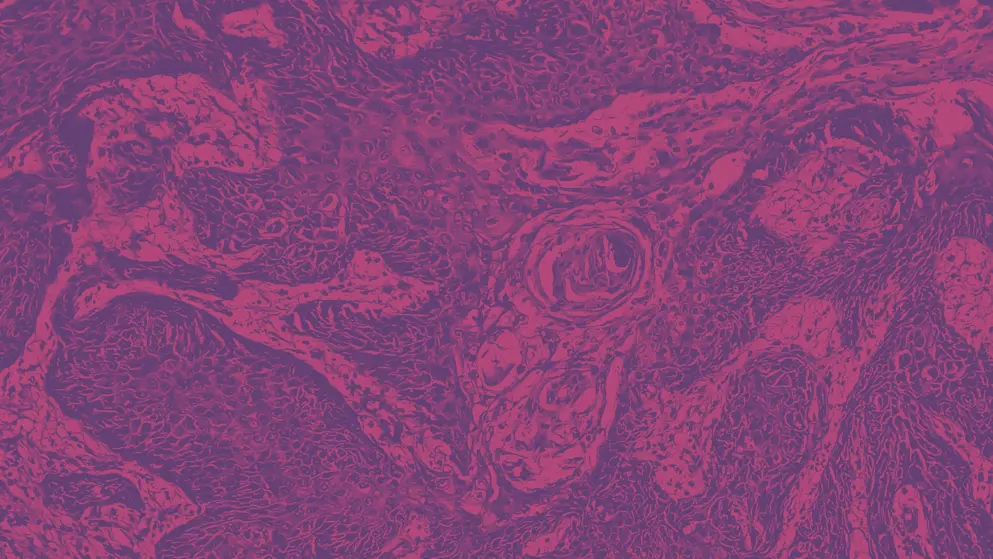
Patients became aware of this even before clinicians and researchers recognised this as a real problem. It's commonly experienced in individuals throughout the disease course, and even after treatment, and can have a more protracted impact on quality of life and functional ability, and obviously a major impact on quality of life when this occurs. It's been reported with a variety of agents, including the anthracyclines and taxanes, so myelosuppressive agents in both haematologic and solid tumour malignancies. It's important that we do whatever we can to prevent or minimise these effects, although we need more information on the real mechanism involved in this toxicity, and hope, fortunately, this seems to be coming from novel imaging studies, as well as preclinical work. It's just fundamentally important at this point that oncology providers be aware of this risk, identify it early in the course of, and of course, that requires close communication and interaction between the physician and the patient, and education of patients and caregivers about the potential of these adverse effects. Most studies have studied the effects of chemotherapy, as I said, but endocrine therapy has also been associated with these, and even some of the newer targeted therapies, but the date is very limited across these newer agents. You have to keep in mind that the impact of cognitive dysfunction or chemo brain is compounded by ongoing active disease status. So, if the patient has progressive cancer, or have they've added targeted therapy to traditional chemotherapies, that may further increase the risk. And, even the increased use of immunotherapy checkpoint inhibitors is being studied, as it may further add to the risk of these problems. And then finally, other things that we might talk about, like fatigue, depression, sleep disturbances, all may contribute to the risk of chemotherapy-related cognitive impairment. As far as neuropathy, particularly peripheral neuropathy, this can be apparent a perineoplasticQ manifestation of the cancer itself, but it's important to recognise that there are specific chemotherapeutic agents, the classic example are the vinca alkaloids or the taxanes, may increase the risk of more severe neuropathy. And, of course, again, this may limit the dose and duration of these agents that are utilised for patients or permitted by patients, as it may impact on their quality of life, their employment, their general functional wellbeing. So, it can impact both disease control and long-term outcomes. Recent guidelines on the management of chemotherapy-induced peripheral neuropathy have confirmed that there really are no well recognised agents for prevention of this complication, although a lot of research is ongoing, and the fundamental recommendation to clinicians is to continually assess the occurrence of chemotherapy-induced peripheral neuropathy, and consider again, modifying the treatment when safe to do so, reducing the dose and prevent the development of intolerable neuropathy, and its impact on the patient's quality of life and functional ability. The recent agent duloxetine has been used by some, but the data has limit, but it is sometimes used for established painful chemotherapy-induced peripheral neuropathy.
Updates in your area
of interest
of interest
Articles your peers
are looking at
are looking at
Bookmarks
saved
saved
Days to your
next event
next event
Developed by EPG Health for Medthority. This content has been developed independently of the sponsor, Sandoz, who has had no editorial input into the content. Medthority received unrestricted educational grant funding from the sponsor in order to help provide its healthcare professional members with access to the highest quality medical and scientific information and associated relevant content, without any promotional intent. This content is intended for healthcare professionals only.

