Supportive care in oncology Learning Zone
Transcript: Haematological side effects
Dr Gary Lyman
All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
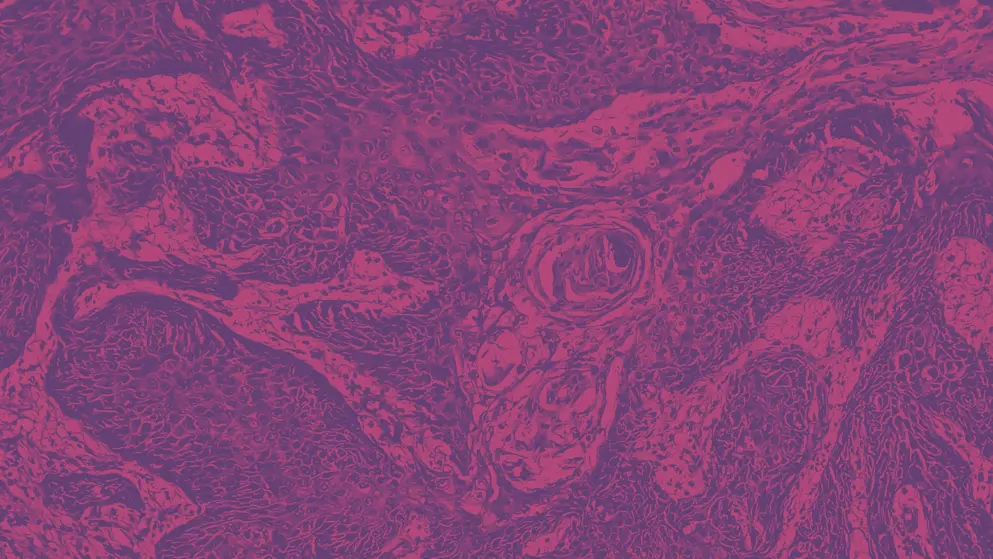
The most common haematologic side effects of cancer therapies are what one might expect. It affects myelosuppression based on the cytotoxic nature of traditional chemotherapies. These can impact particularly on neutrophils or white cell precursors, as well as, of course, red cells causing anaemia, and even sometime megakaryocytes causing low platelets, thrombocytopenia.
The most common, however, and probably the major dose-limiting toxicity associated with traditional cancer therapies is that of myelosuppression, resulting in neutropenia. The risk of fever or infection in the setting of neutropenia is considered a potentially serious and life-threatening complication. These patients who develop what we call febrile neutropenia require urgent evaluation, often are hospitalised for empiric broad spectrum antibiotics. And, we know that these occur with considerable frequency in patients getting more intensive therapy.
There are very costly, but effective preventative agents. The myeloid growth factors, such as granulocyte colony-stimulating factor, are uniformly recommended across clinical practice guidelines for high risk, and many intermediate risk patients receiving chemotherapy. And again, it has potential dual effect, both causing a life-threatening infection, in some cases, but also sometimes leading to early termination of therapy or reduced dose intensity of therapy that may compromise their long-term cancer control. Routine use of these in high and intermediate risk patients is recommended across guidelines, including those in the American Society of Clinical Oncology, ASCO, the European Organisation for Research and Treatment of Cancer, EORTC, and here in the States, the National Comprehensive Cancer Network, NCCN, all recommend that patients at 20% or greater risk of febrile neutropenia should routinely receive prophylactic GCSF [Granulocyte Colony-Stimulating Factor]. Patients less than 10% should not receive these agents because of their cost and potential adverse effects. There's still a grey area in the intermediate risk between 10 and 20% risk of these complications, where the current guidelines recommend if you have one or more additional risk factors for febrile neutropenia, then you should consider using these agents. Fortunately, we have developed risk models for assessing that level of risk, and they are available from a number of organisations. The downside from these agents, major side effect for some patients, is severe bone pain, which is transient, and often it recovers within a day or two. But, particularly important in the States is the exceptionally high cost of these agents that may impose a financial burden or financial toxicity on patients. There's also been a suspicion that there may be an increased risk of acute leukaemia or myelodysplastic syndrome, although we always mention that these are being used to support patients getting known leukemogenic chemotherapeutic agents, so it's hard to sort out major effect. Recent addition to the armamentarium is the CDK [Cyclin-Dependent Kinase] 4/6 inhibitor trilaciclib, which transiently arrests haematopoietic stem cells that are dependent on CDK4/6 for proliferation. So, in selected tumours like small cell lung cancer, they've been shown to reduce the risk of severe neutropenia and febrile neutropenia, and have been recently approved by the FDA for that. Finally, because of the cost issues, a number of biosimilars, highly similar myeloid growth factors, forms of GCSF, have been developed that are now providing competition. And some early data suggests they may help reduce the price and overall cost associated with these agents in clinical practise.
Updates in your area
of interest
of interest
Articles your peers
are looking at
are looking at
Bookmarks
saved
saved
Days to your
next event
next event
Developed by EPG Health for Medthority. This content has been developed independently of the sponsor, Sandoz, who has had no editorial input into the content. Medthority received unrestricted educational grant funding from the sponsor in order to help provide its healthcare professional members with access to the highest quality medical and scientific information and associated relevant content, without any promotional intent. This content is intended for healthcare professionals only.

