Supportive care in oncology Learning Zone
Transcript: Febrile and non-febrile neutropenia
Dr Gary Lyman
All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
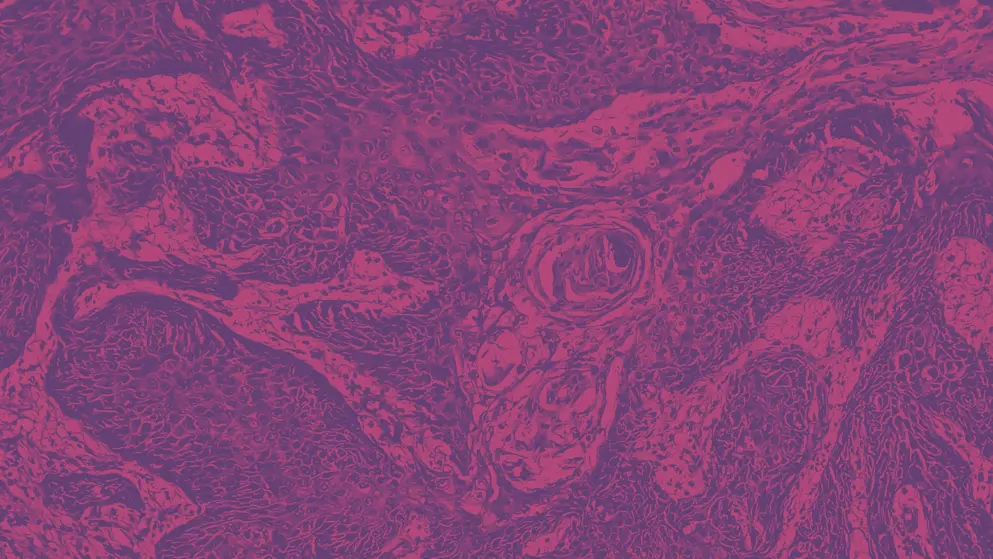
Fever, or signs of infection, in a patient with cancer may represent a complication of myelosuppression, or bone marrow suppression, due to myelosuppressive chemotherapy.
So, it's important if a patient develops a fever, and has been on chemotherapy, to urgently assess the neutrophil count, so the patients need to have blood counts obtained, and then if the patient is neutropenic and febrile, this is considered tantamount to a potentially serious, life-threatening infection, and that patient needs to be evaluated clinically, often with cultures and imaging studies. If an infection is suspected or confirmed, these patients are frequently hospitalised for empiric broad spectrum antibiotics while awaiting the results of culture and imaging studies.
So, it is an urgent, and considered a medical emergency. Now, there are some situations, in some patient settings where the risk remains low, or the ability to treat these in the ambulatory setting has been established, but this requires, of course, a considerable institutional support system, and a way of maintaining a close coordination with the patient and the family to be sure if the symptoms or signs of disease worsen, that they are promptly hospitalised. The, as I mentioned, and many of us know, there are effective, but very costly preventative agents, for febrile neutropenia in patients receiving cancer chemotherapy.
These are recommended across guidelines, from major professional organisations in patients at high risk, considered 20% or greater for febrile neutropenia based on their chemotherapy, but also in patients at intermediate risk, between 10 and 20% risk of febrile neutropenia. If they have other risk factors for febrile neutropenia, or risk factors for serious outcomes from febrile neutropenia, comorbid clinical conditions, and history of prior febrile neutropenia, should prompt consideration of the use of these preventative agents.
Once a patient is hospitalised with febrile neutropenia, the treatment of choice is antibiotics, and then refining those antibiotics based on culture results. But, keeping in mind that probably about half of patients with febrile neutropenia, the cultures may return negative, and many of them do not have pneumonia, or other clear imaging documentation, and yet with antibiotics, with empiric antibiotics, they most often recover. However, our own data here in the States would suggest in the real world setting where many patients have comorbidities, or comorbid illnesses that were not, would have precluded their being in randomised trials, those patients are at particularly high risk for febrile neutropenia, prolonged hospitalisation and even mortality, despite effective therapies.
So it remains a serious, potentially life-threatening problem, and the need for prompt evaluation, prompt risk assessment, so that you've identified the patient at greatest risk for the use of these effective agents that, again, are very costly. And, then of course, we need to find a way to make the cost to the healthcare system, and particularly to patients here in the US, patients suffer from out of pocket costs and under insurance. So, the development of highly similar agents to these myeloid growth factors, what we call biosimilars, has been very important.
We now have six biosimilar forms of GCSF [Granulocyte Colony-Stimulating Factor] in the US, and again, early data suggesting that there's the competition is beginning to lower the price, but these are still very expensive. Even the biosimilars are expensive. Because these are complicated biologic agents, that are very costly to develop and get approved. So, we, a lot more work on the cost side is needed, so as to prevent these complications from leading to patients stopping therapy, or reducing the effectiveness of therapy that may impact on their chance of curing the cancer.
Developed by EPG Health for Medthority. This content has been developed independently of the sponsor, Sandoz, who has had no editorial input into the content. Medthority received unrestricted educational grant funding from the sponsor in order to help provide its healthcare professional members with access to the highest quality medical and scientific information and associated relevant content, without any promotional intent. This content is intended for healthcare professionals only.

