Roundtable discussion: Biologics in plaque psoriasis
Transcript: Real-world evidence update
Professor Luis Puig, Professor Matteo Megna and Professor Matthias Augustin
Roundtable recorded Apr 2024. All transcripts are created from roundable footage and directly reflect the content of the roundtable at the time. The content is that of the speakers and is not adjusted by Medthority.
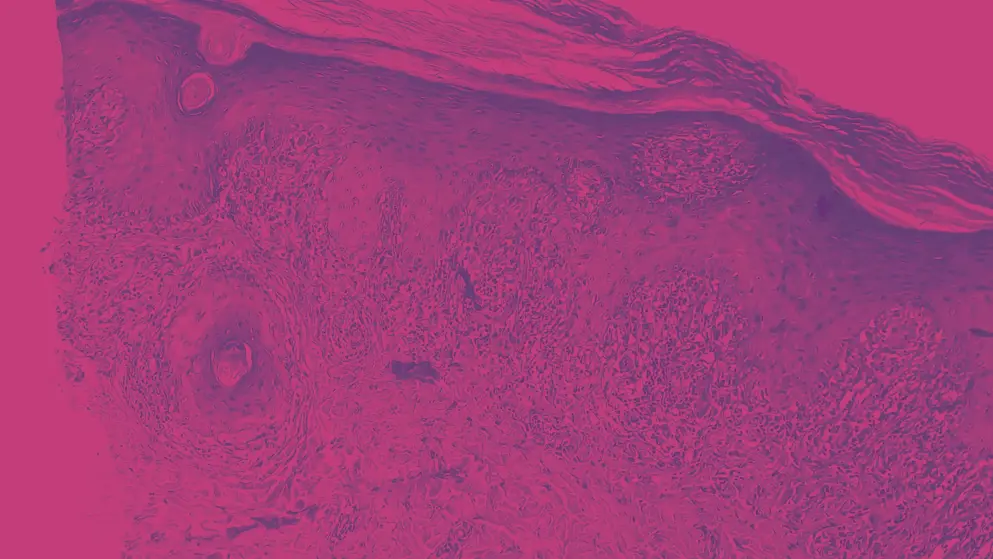
I will be happy to introduce Professor Matteo Megna with his topic, "Biologic therapies for moderate-to-severe plaque psoriasis: real-world evidence update." Matteo, the lectern is yours. Many, many thanks. I'm very happy to be here with you this afternoon to share our experience regarding neurologic drugs and plaque psoriasis. As regards my topic, we all know that in the last 15 years, we have numerous advance in psoriasis pathogenesis knowledge, which clarify the proinflammatory cytokine axis which guide psoriasis pathogenesis. So we know that interleukin-23/interleukin-17 axis is the key axis of psoriasis pathogenesis, and this led to the development of selective drugs, biologic drugs, which completely positively revolutionised psoriasis treatment scenario.
But we all know now that we have 12 different biologic drugs to treat psoriasis, and so we must choose the best drug for our patient, and so to select the right drug in the right moment for the right patient. And to do so, we cannot rely only on safety and efficacy data from trials, but we all know that we deal with the more complex and complicated patients in real life for different reason. We all know that the population of trials is ideal, selective. For example, in the past, with anti-TNF-alpha, it was very difficult to include patient that were more than 65 years of age. Now the situation is different with new trials of anti-interleukin. So we all know that we need efficacy and safety data from real life, we need evidence from real world to base our treatment selection for our patient. And so before to proceeding the slides and deeply investigated this important difference, I will be very happy if my colleagues can make some consideration in this topic before going on. Well, I would like to introduce that one of the first papers that covered the huge difference between real-life patients and those in clinical trials was the Spanish registry, the Spanish registry. 30% of our patients would never be able to enter clinical trials.
And we all know that many of them have comorbidities, infectious diseases and cancer, old age, pregnancy or possibility to become pregnant, which make this real life quite different from clinical trials. Yes, agree. Yes, in fact, Luis, if I may follow you, I just wanted to mention the same first paper and several others followed from different registries across Europe and beyond, coming always to the same conclusion, it's not just that there's a high selective effect of the RCTs compared to the real-world population, but there's also a misdiagnosis, a known mistake of the risk of, in terms of safety in the RCT data. In other words, the registry data also show that those who were not eligible for the clinical trials had higher risks in terms of safety and also had poorer outcomes, at least of those drugs which were the first generation of biologics and non-biological systemics. So we surely underestimate the outcomes, the safety, if we only focus on RCTs instead of real-world evidence. The problem with registries is that most of them focus on adverse events and there is not, for a long time, there was not much evidence gathered as regards to efficacy. And then we have been left with the drug persistence or survival as a distillate or somehow a surrogate of the effectiveness and safety of the drug in real world, but this has some limitations also, we might discuss them later on. Yes. Absolutely. Yeah, I think this is why Matteo wisely posted both on a scales with an equivalent weight. We need to know the RCT data, we also need to know the real-world data.
Yes, completely agree. We can make several examples of this huge difference between trials and real life. We know that in trials, we must perform a washout period from the previous drug to another. This thing is not usually performed in real life. We know that patient with multiple comorbidities, for example, hepatitis C, hepatitis B, HIV, and so on, are excluded from clinical trials. And there is one classical example, latent tuberculosis infection. We all know the concern regarding antitumor necrosis factor drugs, which can reactivate latent tuberculosis infections. But now we know that, of course, in limited amount of patients, we have also some trials of anti-interleukins where a small group of patient with latent tuberculosis infections, when enrolled, even if they didn't perform, in some cases, the prophylaxis with the rifampicin or isoniazid, and this is a very important topic because we all know the toxicity of the drugs used for tuberculosis prophylaxis. And so we all know that it's not simple to always perform the prophylaxis, not to treat with biologic drugs and wait one month before treat our severe psoriasis patients. And we also know that from real-world data, we not only verify the efficacy and safety of biologic drugs in more complicated patients for comorbidities, polypharmacy, age range, and so on, but also because new safety issue or new paradoxical events comes from directly real-life data.
For example, with anti-interleukin-17, with first trials, there was a huge terror regarding candidiasis, so Candida infections. But with secukinumab and ixekizumab, we observed a small amount of infection respect what trials was putting attention, while, for example, with another anti-interleukin-17 drug, bimekizumab, we are now observing a little difference, a more frequent Candida infection respect ixekizumab or secukinumab. So this is to highlight that we need the real-life data, we need this kind of evidence to highlight the peculiarities of each drugs and so to use them in the best way for our patients, but this is only one example. We know the issue of paradoxical eczematous reactions that we observed with anti-interleukin-17, and that was something that was not highlighted by clinical trials, it was something that's just raise up during our clinical practise. And so before going on just, and continue to highlight the new evidence from real-life studies, just want to ask you once again your consideration for this starting point before to continue these slides.
There's one comment I would like to make regarding another difference of this in some countries, is the adjustment or individualisation of the dosage that takes place in some patients, and also the procedure of combination that I will cover a little bit in my talk in our discussion later on. I think ideally, it's also a circle process. Once we have identified the important questions from the real-world data, we may get into the controlled environment and set up another RCT to verify this. And I think RCT research doesn't end with the approval of the drug, but there's important questions which still need to be clarified with this integrated into real-world questions. Yeah, among the comorbidities that you have been discussing, the psoriatic arthritis might be one of the most relevant ones because also to large extent, it determines the choice of the biologic in many patients. So this is something that has been covered in different registries, in different real-world drug survival data, that there's a bit of a difference in terms of persistence across different biologics and across also based on the indication for the treatment.
Some patients with psoriasis, skin psoriasis, skin manifestations predominate, in some others, arthritis might predominate. And then the persistence of any drug, it might be prolonged because it's less easy to to identify loss of response or loss of efficiency in patients when we are treating psoriatic arthritis, it's the problem of the subjectivity of symptoms or outcomes in psoriatic arthritis. Yes. Yes, so the real-life landscape is more complex. We need to, yes, highlight and investigate on different factors to choose the best drugs for our patients. So just to continue on this topic, what we learned from real-world data? Of course, we learned that biologic drugs are also efficacious in safety in elderly patients.
There are plenty of publication of real-life, especially on anti-interleukin-17 and anti-interleukin-23, regarding the use in patient with more than 75 years of age. So now we are not scared anymore respect the past to use these drugs in elderly patients. We are less scared about pregnancy. Of course, we all know that there is certolizumab, which is an anti-TNF-alpha that we can use during pregnancy. But now we also know that in the first trimester, the biologic drugs doesn't cross the placenta. And we all know that there is no study that show that is a higher risk of foetal damage with use of biologic drugs compared to people who do not use biologic treatment. So also in this context, we have different case series or case reports that highlight this topic. Now we know that we can use biologic drugs also in patient with severe kidney function, so also patients on dialysis can be treated by biologic drugs, there are plenty of case series and case report on these topics.
And one that is also emerging in this time is the use of biologic drugs for plaque psoriasis in patient with a cancer, especially if the patient has got very recently the cancer and performing immunotherapy, which make worse psoriasis. We are observed now different cases of severe psoriasis which is induced by immunotherapy for cancer disease. And now we know that in guidelines, there is this cutoff of five years respect the onset of cancer, but there are plenty of publication of real life with use of biologic patients in people with less than five years from the onset of cancer or with an actual cancer, especially for new anti-interleukin-17 or 23 that are considered the most safe drugs in this kind of patients. And of course, also patients with hepatitis C or hepatitis B, which are always excluded by clinical trials, there are plenty of real-life studies which show the safety of these drugs, of course, with the antiviral prophylaxis when indicated.
So. Yes. No, the only explanation for this five-year gap is because sponsors wanted to get a clean slate, they did not want to get their patients taken away from the clinical trials because of the appearance of cancer. But even so, sometimes, investigators get some patients into clinical trials which probably would not be into them that can develop pancreatic cancer after three months, and this is a problem of selection. And the same happened with, for instance, suicidality or suicides in famous clinical trials when only that company which did not pre-select for patients with depression or suicidality were the ones in which this signal appeared. It's interesting in that respect, I would like to comment a bit on the adverse events. What's your take on inflammatory bowel disease in patients treated with IL-17 agents? Yeah, yeah, it's a very good questions. We all know that they are contraindicated in patients with a history of inflammatory bowel disease, but there are plenty of meta-analyses which show that the use of these drugs do not increase the risk of inflammatory bowel disease in patients who not suffer from this disease.
There are plenty of meta-analyses on this topic, but of course, their use is able to make worsening inflammatory bowel disease. So I don't know your clinical practise, but we just rely on a good anamnesis and medical history. But for example, we do not perform some tests like faecal calprotectin before start anti-interleukin-17 drug because it's very specific. No, actually, we also rely on the history, and I think that, once the patients have active symptoms of IBD, they may be not included in IL-17 treatment, but those who have a previous history or a family history, they are still candidates, and this is also what the registries show. Yeah. Of course, and the reason why we mostly do not use IL-17 blockers in patients with a short history of IBD is that other drugs are more helpful as a treatment against the IBD, as we know from ustekinumab, for example, for long, they have an approval for this, and so this is the choice, but not the risk of inducing IBD. Completely agree. Yeah, my index of suspicion is especially raised in those patients who also happen to have axial psoriatic arthritis, because in patients with spondyloarthritis or axial psoriatic arthritis, subclinical microscopical evidence of intestinal mucosal alterations can be found in up to 40%, even in the absence of symptoms.
Updates in your area
of interest
of interest
Articles your peers
are looking at
are looking at
Bookmarks
saved
saved
Days to your
next event
next event
This content has been developed independently by Medthority who previously received educational funding from UCB Biopharma SRL in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
