Roundtable discussion: Biologics in plaque psoriasis
Transcript: Choosing the right treatment for the right patient
Professor Luis Puig, Professor Matteo Megna and Professor Matthias Augustin
Roundtable recorded Apr 2024. All transcripts are created from roundable footage and directly reflect the content of the roundtable at the time. The content is that of the speakers and is not adjusted by Medthority.
So now we are going to start with a discussion by Professor Matthias Augustin about choosing the right treatment for the right patient, biologics in moderate to severe plaque psoriasis. Matthias. Yes. Thank you, Professor, Puig. Thank you, Luis. In fact, we need to deal with this turn in perspective. In clinical trials, we choose the right patient for the right treatment, and we work, we choose the right treatment for the right patients, so it's the opposite direction. And there are several questions coming up.
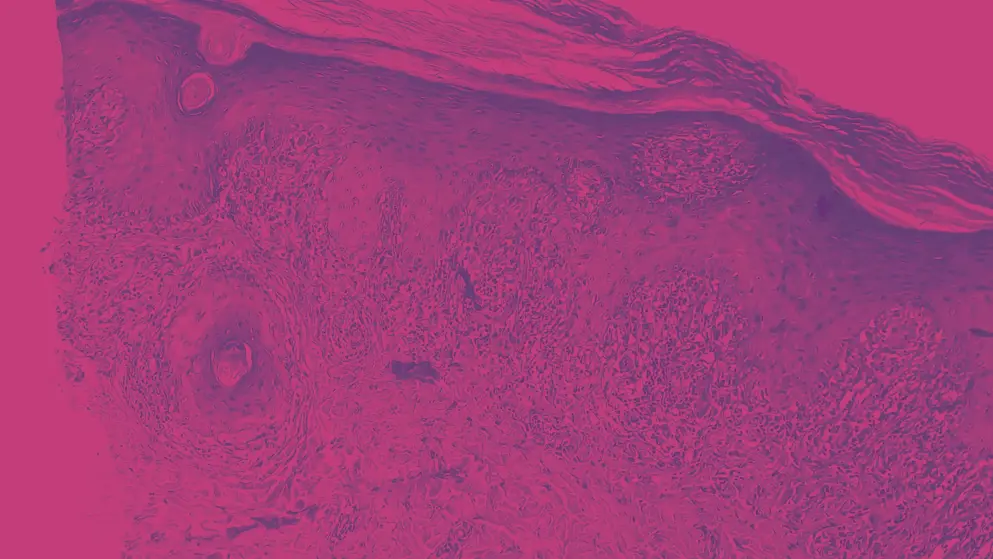
First is, who chooses? Ideally it's a shared choice following shared decision between the doctor and the patient. Second, what does right treatment mean? Is it the best, the most rapid, the safest, the most cost effectiveness, the most long lasting? This is also what we need to clarify in our decision making. And third, how can we optimise choices and learn from the expert? And that's why we're here. And we already see one of my routine patients could also be your patient, Matteo and yours Luis. It's a typical age, typical duration of disease. It's untypical that there's no comorbidities, but maybe [...] has not been screened. We need to screen for this when we see a new patient. And in this stage with those high ratings of the scores that you see, it's truly a patient for systemic treatment. And the question is how to start in which our thinking is in this selection of the drugs.
In Europe, we have 19 systemic drugs for plaque-type psoriasis and even more with when we include psoriatic arthritis. It's 24 different systemic compounds. And my question to my dear colleagues is, do you have this very quick thinking on how to allocate such a patient to a treatment group or a single drug? Is this something that you can do with a reflex or does it take more efforts? I start with Matteo, Professor Megna. Yes, Yes, I usually have to think about different factors before starting a treatment. Of course, in my ideal scenario, I would like to directly start with biologic drugs, but we know that country by country, we have different regulations. So for example, in Italy, we have to at first start with conventional systemic treatment because I see that this patient only used topical drugs. Mm-hmm, and what about Spain? Luis, please.
Oh, I was thinking that this patient, on the other hand, has no prior experience with systemics, and he might be a good candidate for, let's say, conventional, classic systemic treatment. If the flare is of short duration, there's no contraindication, hypertension, whatever, even cyclosporin might be an option, methotrexate for sure, or UBV could do perfectly well in this patient. Now the issues are about logistic accessibility, about which to become to, to serve children. There are some other issues about the potential liver, fatty liver or metabolic liver disease because this patient seems to be a bit overweight at least. But systemics would do, could do a very good job. There's no evidence of arthritis.
There's quite a significant inflammation. Then I would like to go for a quick-acting biologic. I would say in my country, we should try first systemics or UVB. And then according, in most cases, unless there's a contraindication or some other reason, biosimilar in, nowadays, biosimilar anti-TNF-alpha agents, mostly adalimumab, will be the first choice. So I would take compelled, but there's a recommendation that I use biosimilars for 90% of my biologic-naive patients. So that's the situation here. Yeah, thank you for these great responses. In fact, these are the criteria we also, of course, consider, though we do not need to have a non-biological treatment as first line, first drug. We just need to justify when not to use it. And, of course, the prospect and the probability of a response is much higher with the biologics, and then we can use them. And the special criteria here where I didn't show you, but this is a truck driver, so he goes long distances and cannot be under continuous control once there are side effects. So we didn't use fumaric acid esters for this. They have a wish for a child. That's why we didn't use methotrexate, actually.
Cyclosporine is not in need and not also not a long-term option anymore. So we chose and IL-17 blocker here in this patient, and he did very well very soon. But behind this, of course, is a series of thinking and of decision processes which I tried to show you in a systematic way, how's the selection process? And for sure, we need a lot of information. We need the clinical criteria. We just saw a few on the phenotype, the locations, the severity. You need the scores. We need to know the comorbidity, we talked about this already, and pre-treatments which already were failing, for example. Then we need to pair this with the drug characteristics. What is the expectation of effectiveness also on comorbidity?
What about safety feasibility? And surely we need to integrate the patient in the decision making, the preferences, age, gender, special wishes, like for a child, the adherence to treatment in those who cannot come very often. And finally, the the label, of course. We don't want to be off-label in this indication. The cost and cost effectiveness, we need to identify the drug which provides the purpose with the least cost, that's imperative in most countries, and we have the regulations and also the access to the drugs. So a lot of choices to be made. And we already saw in our discussion, in three national discussion, that the framework for this may be quite different. If we come to the choice of drugs here, one of the earliest and accessible information is the clinical outcome from the RCTs. And since we have so many drugs in the meantime, we need to compare them, and for this, one decision aid is meta analysis or network meta analysis. In the next slide, I will present you one of many which have been conducted, and the outcome, the findings are really quite similar.
And here you see the one-year data roughly from 23 trials of many treatments depicting PASI 90 in violet and PASI 100 in green. And you already see that quite large number of drugs has almost the same meta analytic response rates in terms of PASI 90, the IL-17 blockers. IL-23 blockers are included. And you some more have come into healthcare in the meantime, but it already depicts that still, if we look just as one parameter, this is the PASI 90, PASI 100 responses, the choice means broad. There's still the the need to we find these choices. The question is, what else do we have to consider rather than just looking at the PASI 90, PASI 100 responses? And why do also other drugs which are listed here like adalimumab, infliximab, apremilast, why are also they sometimes a choice?
And this, what I will want to depict to you in the next and final slide, it's because there are many more patient needs than just the PASI 90, PASI 100 endpoint, which surely is important, but there's also the wish, and this is from many thousand patients published in the global report on psoriasis by WHO disease control, but also sometimes itch plays a role, the need to have a normal everyday life, leisure activities, that getting rid of pain, many more. You see this. And if we see all this, we clearly come to the conclusion that the right drug for the right patients is a very individualised decision that we have to drive, and we cannot just follow RCT data, that's what we heard already from Matteo, but we also cannot just follow one endpoint saying that just with the PASI 90, PASI 100 outcome we have a clear solution. It's more. It's beyond this. It requires shared decision making, and it requires to listen to the patient about the the things which for him are surely important. So with this, I open the discussion between us again, and maybe Luis is the first who can answer this.
Is it also your daily practise that you weigh up between different outcomes the patients find important, and does this drive your decision as well? Indeed, but the problem with depending, relying too much on subjective or perceptions from on the patient's side as opposed to objective assessment of signs of the disease is that sometimes the better the patient becomes, the more exacting or the greater the expectations, and there are some issues which might not depend on our treatment, so it might depend on the system or on some psychological traits, or even psychiatric comorbidities of our patients. Or sometimes, of course, for the patient, the expectation of of non-recurrence is important, but we cannot provide this for the time being. Perhaps, we might eventually be able to modify the course of the disease, but currently we cannot tell our patients, "Oh, I can assure you that this disease will not respond."
There might be relapses might be longer with some drugs than with others, depending on the half-life and some other characteristics of the drugs. But again, I'm a bit concerned about this, or the patient benefit index, because also it's the same with the DLQI. It's so subject to cultural variations to depending on the sex, the age, or the occupation status of the patients. There are so many factors that go beyond our practise, our abilities to treat the disease. What was your take, Matteo, in that respect? Yes, yes, I perfectly agree. We, of course, have to analyse different factors, not only objective, PASI, BSA, and so on. We, of course, have to listen about patient's expectation and symptoms and so on, but we as a clinician must drive the situation because it will be very dangerous if we just blindly follow patient's reports on each and so on, or impact on quality of life that is very difficult to objectively determine the impact.
So, of course, it's important patient's wellbeing, but we so have a very difficult do. We have to select the best treatment, just trying to make an equilibrium between objective data, patient expectations, and so evidence from real-life. So we have to do personalised medicine and just try to catch at the first time the best drug for the patient to avoid switch and so on. And so it's not easy to try to have a balance between all these factors. There are many differences across countries and even among regions, but also in the pattern of health practise. In some countries, nurses are plentiful. In some others, they're a luxury item. In some countries, any dermatologist can prescribe a biologic or whatever, can care for complex patients with psoriasis. In some others, this is restricted to hospitals. So there are so many factors that it is very difficult to provide to a generalisation in that respect. Yes, I'm very scared... Just one second, let just little phrase.
I'm very scared about an unnecessary switch because now we have plenty of drugs. So there might be the tendency to more easily switch the drug, just like three months to three months, and so we must avoid when it's not necessary just to try to change the drugs. I think that we owe the patient an answer to the question if his disease-related symptoms and complaints get better with the treatment. And this goes beyond PASI. It goes into fields like itch and atopic dermatitis. Even more, we know that itch is the central symptom that can also be in psoriasis, and so all these even not directly accessible components of the disease should be covered. I think today we have a really easy life in our decision making because once we choose the drug which has the highest probability of clearing the skin, many of these other goals also improve.
That's what we have seen, not completely, but there is a trend that with the more powerful drug in terms of the clinical outcome, many of the problems are also managed. And this is why my conclusion from this is not to relate to all these single problems, the patient's focus, but to provide the drug which provides the best expectation of success and start with the most powerful drug rather than with the weakest. And this is what is my way of doing it, but I am happy to hear your comments on this. Oh, patients, we are not seeing them so often, so we must tell them that there might be some fluctuation in signs and symptoms of the disease. And as a matter of fact, I get a bit of, I wouldn't say nervous, but when the patient is completely clear at each appointment, sometimes I think that I would like to adjust the dosing so that there's a bit of inflammation that I know I'm treating, because, otherwise, I'm not concerned about over-treating, but I like to have something which is the basis, the inflammatory basis of psoriasis that they want to be able to treat. And this is something that there might be some differences of opinion.
I now practise in that respect. I don't know how do you approach that, but perhaps it's a bit of attention deficit disorder, but when a patient comes completely clear, I get a bit nervous. Yeah. Yes- Now the questionI think, first of all, I'm happy when the patient comes and is clear, but the question then comes, do we have to modify, can we taper, can we play with the dosage and intervals? Of course because we do not want to overtreat him. And as you say, if there's no sign at all, then the treatment may be not needed in this dosage, for example. On the other hand, maybe, Matteo, you can also comment on this in terms of comorbidity. We are not only treating the skin but also the chronic systemic inflammation, and if we don't see anything, it doesn't mean that there's existing inflammation in the system. This is why also emphasise long-term treatment if patients have the disease, severe disease for a long time.
Yes, yes. With the pandemic, we just observe like different classes of biologic react after a discontinuation. We see that some drugs may be effective longer after their discontinuation, some other drugs for a lower time. This is the comparison between anti-interleukin-23, anti-interleukin-17. We know that there are some studies on like, for example, a guide study of tapering the dosage, for example, of guselkumab every 16 weeks and not eight weeks. For me, so this is the future, the topic of the future.
This content has been developed independently by Medthority who previously received educational funding from UCB Biopharma SRL in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
