Congress highlights
The 2022 Congress of the World Muscle Society took place from 11–15 October in Halifax, Canada. Read about developments in Pompe disease.
Advances in the treatment of Pompe disease
By Dawn O’Shea
The 27th International Annual Congress of the World Muscle Society (WMS) has kicked off in Halifax, Canada, and runs through October 15th. Having been curtailed to the virtual world for the last two years as a result of the COVID-19 pandemic, this is the society’s first hybrid annual meeting. Attendees have welcomed the return of the in-person event.
The five-day programme is packed with oral sessions and abstract presentations on a range of conditions including congenital myopathies, Duchenne muscular dystrophy, spinal muscular atrophy and Pompe disease.
Figure 1. Pompe disease is inherited in an autosomal recessive pattern.
Enzyme replacement therapy (ERT) has significantly influenced the treatment of Pompe disease. Akiko Ishii and colleagues from Japan’s University of Tsukuba demonstrated the impact this therapy has had by presenting the case of a patient with childhood-onset Pompe disease who has been on ERT for more than 10 years.1
The patient was diagnosed at 14 years of age. Now aged 24, he is currently walking with a walker and using non-invasive positive pressure ventilation only at night. After initiation of ERT, the following was observed:
- Improvement in forward-bending posture
- Liver CT values improved
- Slight decrease in the CT values of the semimembranosus, rectus femoris and gracilis muscles
- Small decrease in respiratory function (% VC) shortly after commencing ERT, with a decrease of ~1.6%/ year, but a decrease of 3%/year in patients not treated with ERT: considered as the effect of ERT
Imke Ditters from The Netherlands presented the findings of a prospective survey of 116 patients who were receiving homebased ERT with alglucosidase alfa.2 More than 85% of patients experienced no health problems related to ERT. Health complaints during or within 48 hours after infusion were reported 27 times by 17 patients, and those that were reported the complaints were mostly mild. These results will be reassuring for other countries considering or implementing a similar programme.
In the arena of ERT, avalglucosidase alfa is the ‘new kid on the block’, having received approval from the FDA last year and the EMA this year. Jordi Diaz-Manera from John Walton Muscular Dystrophy Research Centre and Newcastle University Centre for Life in the UK, and colleagues, presented new findings from the COMET trial, comparing avalglucosidase alfa to alglucosidase alfa in treatment-naïve patients with late-onset Pompe disease.3
This new analysis of the COMET trial showed treatment with avalglucosidase alfa was associated with a higher likelihood of benefit in respiratory function and in exercise capacity and duration. Using the win-ratio method for reporting composite endpoints and identifying clinically important events, the authors were able to show that these outcomes were clinically meaningful.
Data presented at the congress demonstrate that home-based enzyme replacement therapy with alglucosidase has a tolerable safety profile2
Benedikt Schoser from Friedrich-Baur-Institut in Germany, and colleagues, presented results from the ongoing phase 1/2 ATB200-02 trial which is evaluating the safety and efficacy of cipaglucosidase alfa plus miglustat (Cipa+mig)in adults with Pompe disease.4
Results to date show that the treatment achieved durable clinical benefits up to 48 months.4 ERT-experienced and ERT-naïve participants showed improvements from baseline in six-minute walk distance (6MWD) and mean change in manual muscle test score for the lower extremity. Mean change from baseline in forced vital capacity (FVC) was generally stable in ERT‑experienced cohorts over the follow-up period and improved numerically in the ERT-naïve cohort. Urine Hex4 and plasma CK declined in both cohorts, with greater reductions in ERT-naïve patients.
The most common treatment emergent adverse events (TEAEs) included fall, nasopharyngitis, arthralgia, headache and diarrhoea. The majority of TEAEs were mild or moderate and did not lead to study withdrawal.
But how does Cipa+mig compare to existing treatments for Pompe disease? In the absence of head-to-head trials, Jeffrey Castelli, Chief Development Officer at Amicus Therapeutics Inc, and colleagues, presented the findings of an indirect treatment comparison of three enzyme replacement treatments for late-onset Pompe disease.5
The study found that Cipa+mig was more favourable than both avalglucosidase alfa and alglucosidase alfa in 6MWD and FVC. The findings suggest the new treatment might have a different clinical profile to the existing ERTs, particularly in people who have previously received ERT.
The first day of WMS 2022 presented multiple studies detailing developments and clinical results for efficacy and safety of ERT in Pompe disease
Patient factors and characteristics
By Dawn O’Shea
Patient-reported unmet care needs in Pompe disease
People with rare neuromuscular diseases often face a distressing and lengthy path to diagnosis, sometimes dotted with misdiagnoses. This delay in diagnosis and treatment initiation adds significantly to the disease burden.
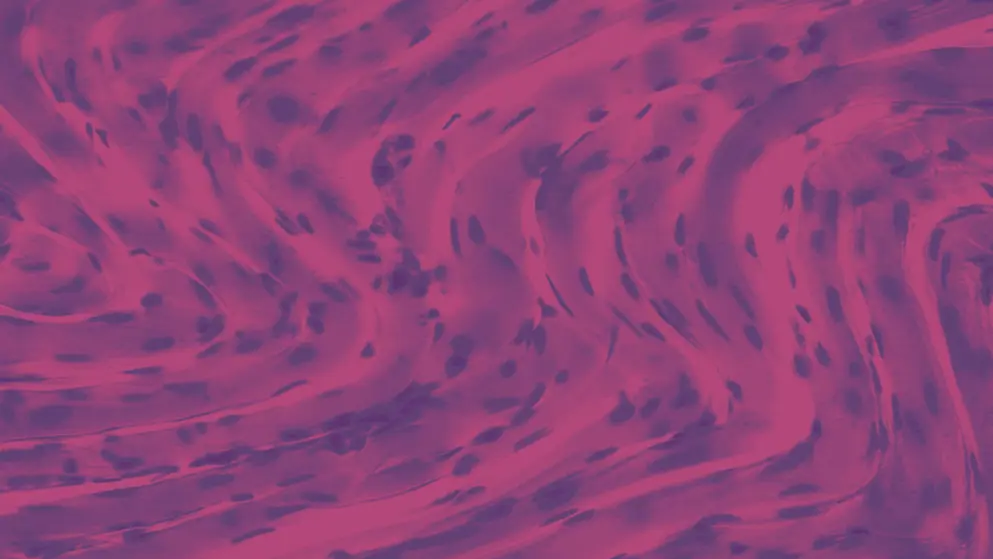
Figure 1. Pompe disease is a rare congenital disorder of the neuromuscular system in which there is progressive muscle weakness.
UK data, presented at the 2022 International Annual Congress of the World Muscle Society, show that people with Pompe disease wait almost 10 years for a confirmed diagnosis, and a significant proportion receive at least one misdiagnosis along the way6. Val Buxton, Chief Executive of the Association for Glycogen Storage Disease UK, presented the findings of an in-depth online quantitative survey of 37 people in the UK living with late-onset Pompe disease (LOPD).
The data showed that the average time between symptom onset and diagnosis was 9.3 years, with an additional two-year wait until treatment initiation with enzyme replacement therapy (ERT).
Forty-six per cent of these patients had received at least one misdiagnosis
More than 90 per cent of participants reported walking difficulties, fatigue and muscle weakness. Almost 85 per cent reported balance issues.
Twenty-six participants were receiving ERT, with half having been on ERT for more than 10 years. Approximately 77 per cent felt their condition had deteriorated since starting therapy.
The survey also asked participants to identify unmet needs. Physiotherapy was top of the list, cited by 73 per cent of respondents as a supporting therapy that would help manage the condition. Interestingly, almost half cited counselling as a top unmet need, which highlights the emotional and psychological burden of Pompe disease.
The emotional journey of people with Pompe disease
Allan Muir, Chair of the Board of Trustees of the UK-based Pompe Support Network, presented the results of a study which identified a characteristic emotional journey which was similar among patients with Pompe disease7.
“Our interviews with people living with LOPD led to the creation of an archetypal emotional journey figure, characterising the rollercoaster experience from symptom onset through to living with a diagnosis of Pompe disease,” he said.
“Unfortunately, people can go through a period of months to several years when their condition is misdiagnosed, often with a frustrating delay before seeing a Pompe disease specialist. Understandably this is a highly distressing time for patients.”
The interviews revealed that receiving a firm diagnosis triggered a range of emotions. As well as relief at receiving a diagnosis, shock, disbelief and anger were common, and many patients experienced guilt about the impact their condition would have on their family. These negative emotions were more pronounced in younger patients.
Despite these changes in circumstances, it’s striking how well people adapt, as LOPD becomes their new norm.
Insights from a Pompe disease registry
Several presentations at the conference focused on the benefits and importance of disease registries for neuromuscular diseases.
Rafael Jenaro Martínez-Marín from Hospital Universitario La Paz, reported on some of the valuable information that has been extracted from the 122 patients entered into the Pompe registry in Spain between 2019 and 2022, which was established by doctors in 20138. Nine of these cases were infantile onset Pompe disease and 113 were LOPD.
The mean age was 28.65 years, with mean creatine kinase (CK) being was 716 UI/L. The most common mutation was IVS1-13T>G. Axial and lower limb weakness were the most common ongoing symptoms, followed by respiratory symptoms, fatigue and upper limb weakness respectively.
Figure 2. Data from the Spanish Pompe Registry indicated lower limb and axial weakness as the most common ongoing symptoms of Pompe disease.
Martínez-Marín highlighted the value of the registry by showing what they have been able to find out about juvenile onset Pompe disease (JOPD), defined as symptom onset between two and 18 years of age9.
In a study of JOPD patients in the Spanish Pompe Registry, 28 children were identified. The mean age at symptom onset was 8.51 years and the main symptom of onset was hyperCKaemia. More than two-thirds reported muscle symptoms and approximately one-third reported respiratory failure.
The data demonstrated differences in the presentation, symptom profile and progression of JOPD compared to LOPD, including significantly higher CK values initially in the former.
These studies provide much needed information on the characteristics, experiences and needs of people with Pompe disease.
Check in tomorrow for more updates from the 27th International Annual Congress of the World Muscle Society.
Research presented at WMS 2022 shines a light on the emotional journey of people with Pompe disease, their ongoing unmet needs, and the value of disease registries for gaining new insights into the condition
The Big Debate
By Dawn O’Shea
Nicol Voermans from The Netherlands debated Jim Dowling from Canada on whether biomarkers should replace outcome measures in neuromuscular disease clinical trials
One of the highlights of the 27th International Annual Congress of the World Muscle Society was the big debate – should biomarkers replace outcome measures in clinical trials10? This engaging debate featured Nicol Voermans from Radbound University Medical Center in The Netherlands versus Jim Dowling from the Hospital for Sick Children in Toronto and a member of the congress organising committee.
Before the participants took to the stage, a pre-debate poll showed that 65% of the attendees were against the motion that biomarkers should replace outcome measures.
Voermans was first to take to the podium. “If biomarkers are the answer, which is the question?” she asked. “You can answer the question, does it work? Can it be used safely? How does it work? But not whether or not it helps the patient, which is what it’s all about.”
Biomarkers reorient the focus of a trial on the biological process of the disease. But for the patient, their condition is an illness, an experience or a feeling of ill health, which is entirely personal. Even in clinical trials, she said, the ultimate endpoint is the benefit to the patient.
Dowling countered, pointing out that biomarkers are already used routinely in clinical practice, and highlighted the use of blood glucose, heart rate and blood pressure measures. In the field of neuromuscular diseases (NMDs), there has also been a shift from clinical diagnostics to genetic diagnosis. “Now we rely on genetics as our way of diagnosing patients,” he said.
The definition of a biomarker is something that can reliably and accurately measure and quantify the presence of disease or the severity of the disease state and response to treatment. Biomarkers are quantifiable, while clinical outcome measures are a qualitative observation of functional measures.
After both opponents had presented their arguments, another audience poll showed that the proportion of people who were opposed to the motion had increased from 65% to 75%. A blow for Dowling but he wasn’t done yet.
The question of whether biomarkers or outcome measures are more relevant for clinical trials partly hinged on the stage of disease being studied and other factors, but on the whole, made for a lively debate
The first comment from the floor put him on the spot. How many patients had he met willing to take on the burden of monitoring just to say, “I’m so happy because my fat fraction infiltration has changed by 2%”? Dowling was quick with a reply. “It’s a matter of education,” he said, “You have to explain to the patient why the marker is important and what it means.”
Voermans also came under fire from the floor. She was asked whether she would use a functional outcome measure or a biomarker if conducting a trial early in the disease process. She acknowledge that early in the disease, biomarkers might be more relevant than clinical outcome measures, but ultimately, the goal of any trial is to deliver real benefit to the patient.
Another audience member posed the scenario of an ultra-rare NMD, or one that has been newly defined, where the genotype is known but little is known about the phenotype. In that situation, would she agree that a favourable pharmacodynamic biomarker response to a treatment would be sufficient to warrant regulatory approval of that therapy? Voermans said that, given that she was arguing against biomarkers, she would have to say no.
Dowling was also put under pressure. Another audience member observed, “If you’re just using biomarkers and you’re looking at the muscle on MRI but you’re not looking at contracture, it may look by the biomarkers that things are getting better but if you look at functional outcomes it might show that the patients is getting worse.” So, from Dowling’s perspective the treatment would be a success but for the patient, it was a failure; not an ideal outcome.
A final audience vote gave the victory to Voermans, with 60% voting against the motion, agreeing that biomarkers should not replace outcome measures in clinical trials in the field of NMDs.
The best of the late breaking abstracts
By Dawn O’Shea
Three late breaking abstracts made it onto this year’s programme, including new data from the ongoing phase 3 COMET trial, which is examining the efficacy and safety of intravenous avalglucosidase alfa and alglucosidase alfa for treatment-naïve patients with late onset Pompe disease
Results have previously been published from the 49-week primary analysis period, which showed greater improvements in forced vital capacity (FVC), 6-minute walk test (6MWT), and other outcomes with avalglucosidase alfa compared with alglucosidase alfa.
Figure: Compared with alglucosidase alfa, avalglucosidase alfa at 49 weeks demonstrated greater improvements in FVC, 6MWT and other outcomes.
At the congress, Benedikt Schoser presented findings from the 145-week open-label extended treatment period of the trial, which show that these improvements were maintained through 145 weeks of treatment11.
In the primary analysis period, treatment-naïve participants with late onset Pompe disease (LOPD), aged three years or older were randomised (1:1) to receive avalglucosidase alfa at a dose of 20 mg/kg body weight every other week (qow) or alglucosidase alfa 20 mg/kg qow.
During the extended treatment period, all 51 people who received avalglucosidase alfa in the primary analysis period continued this treatment (avalglucosidase alfa arm), and 44 of 49 people who received alglucosidase alfa in the primary analysis switched to 20 mg/kg qow avalglucosidase alfa (switch arm).
At 145 weeks, the avalglucosidase alfa arm maintained a benefit compared with baseline in upright FVC% predicted, upright maximal inspiratory pressure (MIP)% predicted and maximal expiratory pressure (MEP)% predicted, and 6MWT.
In the switch arm, predicted FVC% stabilised and there were continued improvements in upright MIP% and MEP% predicted.
There were also improvements at Week 145 in lower extremity composite score (hand-held dynamometry [HHD]) and the Quick Motor Function Test (QMFT) total score in both groups.
In relation to health-related quality of life, the Short Form-12 (SF-12) Mental Component Score (MCS) stabilised in both arms, while the SF-12 Physical Component Score (PCS) improved in both arms compared with baseline.
In addition, levels of urinary hexose tetrasaccharide (Hex4), a biomarker of glycogen burden, improved in both arms. Benefits were also observed in both arms with respect to plasma creatine kinase (CK), plasma aspartate aminotransferase (AST) and alanine aminotransferase (ALT). By week 145, mean biomarkers levels were within or close to normal range.
Avalglucosidase alfa treatment compliance (<2 consecutive missed infusions) up to the last follow-up treatment was 51 per cent for participants in the avalglucosidase alfa arm and 45.5 per cent in the switch arm.
Fifty of 51 participants in the avalglucosidase alfa arm and 43 of 44 in the switch arm reported treatment-emergent adverse events (TEAEs). Of these, 27 in the avalglucosidase alfa arm and 25 in the switch arm were considered TEAEs potentially related to treatment.
Thirteen (25%) participants in the avalglucosidase alfa arm and 12 (27%) in the switch arm had treatment emergent serious adverse events (SAEs), three and two of which, respectively, were treatment related.
Five participants discontinued treatment during the extended treatment period due to six TEAEs. Four of these were deemed to be treatment related: ocular hyperaemia and erythema (experienced by the same person), urticaria and respiratory distress.
These longer-term results from the COMET trial show a similar safety profile for avalglucosidase alfa among participants who were treatment naïve at the start of avalglucosidase alfa or switched to avalglucosidase alfa.
These data suggest avalglucosidase alfa delivers long-term clinically meaningful outcomes
These results may be reassuring given that avalglucosidase alfa was only recently approved in Europe (in June 2022), and approved in the US in August 2021 for the treatment of late-onset Pompe disease for people aged ≥1 year.
The other two late breaking posters looked at biallelic variants. Mridul Johari from the University of Helsinki presented data which indicate that biallelic variants in ASCC3 expand the phenotypic spectrum of congenital myasthenic syndromes12. A team from France and Italy found that biallelic MYO15B variants are associated with a congenital core myopathy with rigid spine, and PAX7 deficiency13.
Join us tomorrow for our final round-up of news from the 2022 Annual Congress of the World Muscle Society
Advances in Pompe disease assessment and surveillance
By Dawn O’Shea
A novel portable device to assess gait features
The COVID-19 pandemic has required changes in the way health care is delivered. For example, telemedicine has provided a new avenue for healthcare delivery, reducing the burden on patients.
Another example of a technological advance that may help meet an unmet patient need was presented by Jordi Diaz-Manera. Diaz-Manera and his team have examined the value of a portable system for gait analysis in people with late onset Pompe disease (LOPD), presenting their findings at the congress. This system may help shift the management of Pompe disease14.
The new device, Ephion mobility, uses a set of commercial wearables embedded within a platform. It includes electromyography (EMG) sensors and plantar pressure sensors integrated in shorts and insoles to enable measurement of muscle and cardiovascular activity, kinematics, plantar pressure and spatial-temporal features.
Diaz-Manera reported on a study of the Ephion device in 18 people with LOPD and 27 unaffected controls. All participants with LOPD were symptomatic and were being treated with enzyme replacement therapy (ERT).
In the six-minute walk test, people with LOPD walked a significantly shorter distance compared with controls.
Individuals wore the sensors while performing the six-minute walk test (6MWT) and the 10-metre walk/run (10M).
People with LOPD walked a significantly shorter distance in the 6MWT (compared to controls (423 ±103.5m versus 655 ±140m, respectively). There were also significant differences in the gait pattern between the groups in relation to kinematics, plantar pressure, spatial-temporal measurements, and EMG signals.
People with LOPD demonstrated greater oscillation of the trunk and pelvis during the stance phase that was associated with a longer extension of the knee, and an increased foot inversion. There were also significant differences in muscle activation using EMG walking, with participants showing longer co-contraction of the knee flexor and extensors while walking compared to the control group.
A decrease in the ground reaction force (GRF) in the heel strike coupled with an increase in the mid-stance resulted in a flattened GRF profile.
Presenting the findings, Diaz-Manera said:
The Ephion mobility device is an easy-to-use assessment to study an array of gait characteristics. We observed some significant differences between the gait pattern of patients with Pompe and control in this cross-sectional study, suggesting that multiple potential outcome measurements to distinguish between these two populations.
However, Diaz-Manera stated that longitudinal studies are needed to identify whether these measurements can capture disease progression over time.
Could neurofilament light act as a biomarker for CNS involvement in patients with classic infantile Pompe disease?
Enzyme replacement therapy (ERT) has led to vast improvements in the management of infantile Pompe disease, which was formerly a lethal metabolic myopathy. As children with this condition now live longer, white matter abnormalities (WMA) and neurocognitive problems have become apparent.
Maarten Mackenbach from Erasmus Medical Center, Rotterdam, The Netherlands, and colleagues have studied the potential of Neurofilament Light (NfL) to act as a biomarker for central nervous system (CNS) involvement in people with classic infantile Pompe disease and its correlation to clinical outcome measurements such as MRI brain scan scores and cognitive tests15.
The researchers collected 74 serum samples from people with infantile Pompe disease (n = 17), and 71 samples (n = 71) from age and sex-matched controls. They found that NfL levels in people with classic infantile Pompe disease increased by 6.0 per cent yearly from a baseline of 10.3 pg/ml, while NfL levels in controls decreased by 8.8 per cent yearly from a baseline of 11.0 pg/ml (p < 0.001).
A doubling of NfL levels led to a statistically significant decrease of 7.7 IQ points and a significant decrease of 13.9 points on the processing speed score
People with higher NfL levels tended to have more WMA on MRI scans, however due to the instability of the mixed effects continuation model, statistical analysis of this datum was not possible.
Presenting the findings at the congress, Mackenbach said; “There is a significant difference in NfL between classic infantile Pompe patients and controls. NfL increases in Pompe patients while it decreases in controls, on a group level, with a clear deviation starting at around age five.”
NfL deserves further exploration as a biomarker for CNS involvement in classic infantile Pompe patients.
And that brings our coverage of the 27th International Annual Congress of the World Muscle Society to an end. Work has already begun on the 28th Congress which will be held in Charleston, USA, on 3–7 October 2023.
References
- Ishii A, Yamamoto N, Nohara S, Hosak T, Kajita T, Miyauchi H, et al. 10-year course of treatment with enzyme replacement therapy for childhood-onset Pompe disease. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. VP.31.
- Ditters IAM, van der Ploeg AT, van der Beek NAME, van den Hout JMP, Huidekoper HH. Safety analysis of home-based enzyme replacement therapy with alglucosidase alfa in Pompe disease; a prospective study. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. VP.29.
- Diaz-Manera J, Ishak J, Caro J, Hamed A, França LR, Thibault N, et al. Avalglucosidase Alfa Improves Motor and LSVP.15 Respiratory Function in Late-onset Pompe Disease: A COMET Win-Ratio Analysis. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. LSVP.15.
- Schoser B, Kishnani P, Bratkovic D, Clemens PR, Goker-Alpan O, Ming X, et al. Long-term follow-up of cipaglucosidase alfa/miglustat in ambulatory patients with Pompe disease: an open-label Phase I/II study (ATB200-02). Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. FP.17.
- Fu S, Hummel N, Mozaffar T, Castelli J, Fox B, Keyzor I, et al. Indirect treatment comparison of three enzyme replacement treatments for late-onset Pompe disease: a network meta-analysis with patient-level and aggregate data. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. LSVP.19.
- Buxton V, Muir A, Johnson N, McCaughey G, Slade P, Hughes D, et al. Quantification of the burden, unmet needs, management, and COVID-19 impact of living with Pompe disease in the UK: results of an online patient survey. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. VP.33.
- Muir A, Hughes D, Bashorum L, Buxton V, Johnson N, McCaughey G, et al. Living with Pompe disease in the UK: characterising the patient journey; burden on physical and emotional quality of life; and impact of COVID-19. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. VP.32.
- Martínez-Marín RJ, Reyes-Leiva D, Nascimento A, Muelas N, Vilches J, Dominguez C, et al. Spanish Pompe Registry: Update of the 122 patients included. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. P.86.
- Martínez-Marín RJ, Caro JMS, Reyes-Leiva D, Nascimento A, Muelas N, Vilches J, et al. Analysis of Juvenile onset Pompe disease patients included in the Spanish Pompe Registry. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. P.85.
- Voermans N, Dowling J. Debate Clinical trials: Biomarkers or functional outcomes? Presented at the World Muscle Society Annual Congress 2022, 14 October. Halifax. I.13, 1.14.
- Schoser B, Kishnani PS, Kushlaf H, Ladha S, Mozaffar T, Straub V, et al. Efficacy and Safety of Avalglucosidase Alfa in Participants with Late-Onset Pompe Disease after 145 Weeks of Treatment during the COMET Trial. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. LBP.1.
- Johari M, Herman I, Polavarapu K, Nalini A, Lupski J, Töpf A, et al. Biallelic variants in ASCC3 expand the phenotypic spectrum of congenital myasthenic syndromes. . Presented at the World Muscle Society Annual Congress 2022, 14 October. Halifax. LBP.3.
- Onnée M, Taglietti V, Cecconi B, Becdelièvre Ad, Bastu S, Villanova M, et al. Biallelic MYO15B variants are associated with a congenital core myopathy with rigid spine, and PAX7 deficiency. Presented at the World Muscle Society Annual Congress 2022, 14 October. Halifax. LBP.2.
- Claramunt M, Idelssohn-Zielonka S, James M, Corti M, Smith B, Salabarria S, et al. Gait analysis of patients with Pompe disease using a portable system. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. P.84.
- Mackenbach MJ, Willemse EAJ, van den Dorpel J, van der Beek N, Díaz-Manera J, Rizopoulos D, et al. Neurofilament Light: a potential biomarker for brain involvement in classic infantile Pompe patients. Presented at the World Muscle Society Annual Congress 2022, 12 October. Halifax. VP.30.
This content has been developed independently by Medthority who previously received educational funding from Amicus in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
