Multiple sclerosis
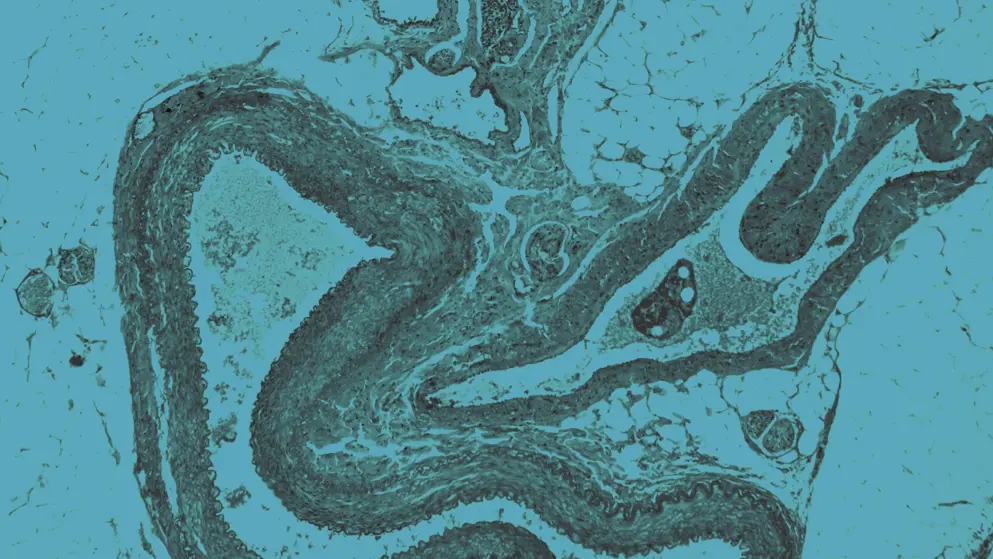
Multiple sclerosis (MS) is an autoimmune disease that disrupts both adaptive and innate immune systems in the periphery and central nervous system (CNS), causing myelin loss and axonal damage. Despite numerous effective disease-modifying therapies (DMTs), novel therapeutic targets are still needed.
What are the common features of multiple sclerosis?
Symptoms include sensory or visual disturbances, motor and coordination impairment, spasticity, fatigue, pain, and cognitive deficits. Diagnosis is based on neurological symptoms and CNS lesions, typically observed using magnetic resonance imaging (MRI). Diagnostic criteria have evolved with updates to the McDonald criteria, reflecting the growing understanding of MS.
Clinical courses of MS include relapsing–remitting (RRMS), primary progressive (PPMS), and secondary progressive (SPMS). However, understanding of progression is shifting away from distinct phenotypes to a continuum model.
Who is affected by multiple sclerosis?
MS typically develops between ages 20–40, with females twice as likely to be affected as males.
Genetic and environmental risk factors include the HLA-DRB1 allele, Epstein–Barr virus (EBV) infection, smoking, limited sun exposure and low vitamin D levels, and adolescent obesity.
What treatments are available for multiple sclerosis?
Treatment options have expanded over the past 30 years. Newer DMTs have increased efficacy compared with traditional therapies but may be associated with increased side effect profiles because of higher levels of immunosuppression.
The main goal of treatment is to delay disease progression and limit disability accrual. Therapeutic strategies with DMTs comprise escalation therapy, intensive continuous treatment, or induction strategies based on risk–benefit profiles.
Treatments for MS include:
- Interferons
- Glatiramer acetate
- Fumarate derivatives
- Pyrimidine synthesis inhibitor
- Sphingosine-1-phosphate (S1P) receptor modulators
- Anti-alpha(4)-integrin antibody
- B-cell-depleting antibodies
- Immune reconstitution therapy
Currently, no therapeutic strategies support remyelination or brain repair, but several potential treatments are under investigation.
Developed by EPG Health for Medthority, independently of any sponsor.
Related news and insights
Related Guidelines
References
- Yang JH, Rempe T, Whitmire N, Dunn-Pirio A, Graves JS. Therapeutic advances in multiple sclerosis. Front Neurol. 2022;13:824926.
- Kuhlmann T, Moccia M, Coetzee T, Cohen JA, Correale J, Graves J, et al. Multiple sclerosis progression: time for a new mechanism-driven framework. Lancet Neurol. 2023;22(1):78-88.
- Rodríguez Murúa S, Farez MF, Quintana FJ. The immune response in multiple sclerosis. Annual Review of Pathology: Mechanisms of Disease. 2022;17(1):121-139.
- Brownlee WJ, Hardy TA, Fazekas F, Miller DH. Diagnosis of multiple sclerosis: progress and challenges. The Lancet. 2017;389(10076):1336-1346.
- Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sørensen PS, Thompson AJ, et al. Defining the clinical course of multiple sclerosis: The 2013 revisions. Neurology. 2014;83:278-286.
- Giovannoni G, Popescu V, Wuerfel J, Hellwig K, Iacobaeus E, Jensen MB, et al. Smouldering multiple sclerosis: the ‘real MS’. Therapeutic Advances in Neurological Disorders. 2022;15:175628642110667.
- Alfredsson L, Olsson T. Lifestyle and environmental factors in multiple sclerosis. Cold Spring Harbor Perspectives in Medicine. 2019;9(4):a028944.
- MS International Federation, Atlas of MS. Epidemiology: Number of people with MS. https://www.atlasofms.org/map/global/epidemiology/number-of-people-with-ms. Accessed 20 July.
- Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS, third edition. Mult Scler. 2020;26(14):1816-1821.
- Callegari I, Derfuss T, Galli E. Update on treatment in multiple sclerosis. Presse Med. 2021;50(2):104068.
- Oh J, Bar-Or A. Emerging therapies to target CNS pathophysiology in multiple sclerosis. Nat Rev Neurol. 2022;18(8):466-475.