ISA 2022 - Highlights article 3
Unmet medical needs in managing tissue toxicity and organ dysfunction
The third highlight article from the 18th International Symposium on Amyloidosis (ISA) 2022 is an overview of the Satellite Symposium, ‘Unmet Medical Needs in AL Amyloidosis’ presented by Giovanni Palladini from the Amyloidosis Research and Treatment Center, University of Pavia and IRCCS Fondazione Policlinico San Matteo, Italy, on Wednesday 7, September 2022, in Heidelberg, Germany.
Current treatments for AL amyloidosis
Current treatments for amyloid light-chain (AL) amyloidosis aim to eliminate anti-plasma cell dyscrasia (PCD):
- Cyclophosphamide and melphalan damage the DNA, leading to apoptosis
- Bortezomib forms a reversible adduct with β5 subunit, resulting in apoptosis
- Dexamethasone induces apoptosis through the nuclear glucocorticoid receptor
- Daratumumab binds to the CD38 transmembrane glycoprotein, inducing apoptosis
Daratumumab is the only monoclonal antibody approved for treating AL amyloidosis12. Immunomodulators can manage refractory AL amyloidosis13. Comprehensive supportive care to maintain organ function in AL amyloidosis should be initiated at diagnosis with anti-PCD treatment14.
Watch the following video to hear Professor Giovanni Palladini discuss his opinion on how clinicians should best use approved treatments.
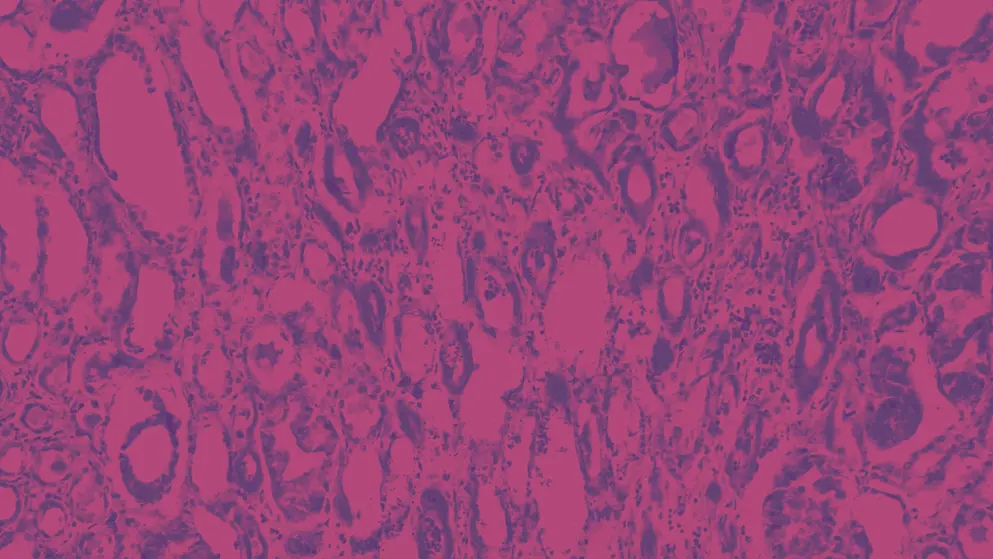
Organ tissue damage due to amyloid fibrils is an unmet need – eliminating amyloid fibril deposits can hasten recovery of organ function14
Targets of investigational anti-fibril antibodies
CAEL-101, dezamizumab, and birtamimab are current investigational agents that target existing amyloid fibrils.
- CAEL-101 results in degradation of misfolded light chains and amyloid fibrils
- Dezamizumab exposes amyloid fibrils to degradation
- Birtamimab cross-reacts with and degrades misfolded light chain amyloid fibrils
Panel discussion on the suitability of treatments to assess organ damage
Professor Giovanni Palladini invited the expert panel to comment on the suitability of treatments to assess organ damage, particularly cardiac damage, in AL amyloidosis.
Dr Rodney Falk (Brigham and Women’s Hospital, USA) observed that, “We only know what we know”. Cardiac magnetic resonance imaging (MRI) provides clinicians accurate information on extracellular volume, although it is now understood that extracellular volume results from amyloid deposits and fibrosis. Patients treated with antibodies for cardiac amyloid deposits can still fail to meet treatment outcomes because of cardiac fibrosis. Current clinical trials of CAEL-101, dezamizumab, and birtamimab, should provide a more complete picture of the efficacy and safety of these antibodies for AL amyloidosis.
Professor Julian Gillmore (National Amyloidosis Centre, UK) agreed with Dr Falk. He added that we really don’t know the effects of accelerated removal of amyloid deposits from the heart with the use of new antibody treatments. New antibody treatments could cause, or worsen, cardiac fibrosis, or weaken the ability of the heart of pump. Preclinical studies of investigational agents that target existing amyloid fibrils are nonetheless promising.
In response to Professor Gillmore, Professor Vaishali Sanchorawala (Amyloidosis Center, Boston University School of Medicine, USA) observed that there are no preclinical data showing that amyloid deposits, once removed through anti-fibril antibody treatment, has permanently regressed. We rely on animal data from surrogate cardiac biomarkers of organ dysfunction, which are only proxies. Therefore, cardiac MRI is critically important in assessing treatment efficacy in humans.
Professor Ashutosh Wechalekar (National Amyloidosis Centre, UK) noted that tracking full-body amyloid loads is important. Improved understanding of how the amyloid fibrils impact on the organ is another unmet need. He said, “We don’t really know what the fibrils are doing when they are sitting there”. Even when patients have achieved complete response (CR) status, it can take several years before the patient shows normal functional values. Therefore, we need to better understand the cardiac remodelling that occurs following amyloid degradation.
Evidence linking amyloid deposits to cardiac and renal dysfunction
Professor Palladini invited Professor Gillmore to summarise the evidence linking amyloid deposits to cardiac and renal dysfunction. A rule of thumb, Professor Gillmore pointed out, is “No amyloid, no disease”. On the basis of SAP (serum amyloid P component) scintigraphy evidence, if amyloid deposits increase, then cardiac or renal function deteriorates. However, compared with liver function, there is no fixed relationship between amyloid regression and improved cardiac or renal function.
Moving endpoints during treatment and patient follow-up
Professor Wechalekar acknowledged that this is a challenge, given the dual nature of endpoints in AL amyloidosis treatment: (1) quantity of amyloid deposit, and (2) amyloid improvement in the target organ. These endpoints are unrelated. All current therapies target the precursor. It could be easier to change the goal of treatment based on patient response to treatment. It is unclear how frequently treatment endpoints or goals should be tracked. Large, long-term collaborative studies could help solve these questions.
Professor Sanchorawala noted that frequent changes in treatment are not usually assessed in relation to patient quality of life, as a management goal.
Watch Professor Giovanni Palladini discuss some of the unmet patient and medical needs affecting the management of AL amyloidosis in the following video.
To conclude the panel discussion, Professor Gillmore urged the audience to collect a range of data to help determine “what we should be looking for” in a given patient.
About Professor Giovanni Palladini
Giovanni Palladini is a Professor of Clinical Chemistry at the University of Pavia and the Director of the Amyloidosis Research and Treatment Center at the Foundation IRCCS Policlinico San Matteo, Pavia, Italy. He has contributed to the introduction of novel agents in the treatment of AL amyloidosis. His studies led to the establishment of standards of care for the treatment of patients with AL amyloidosis, to the introduction of NT-proBNP as a marker of diagnosis, prognosis, and response of cardiac involvement in this disease, and to the establishment and validation of criteria for hematologic and organ response to therapy in AL amyloidosis.
Disclosures: Professor Giovanni Palladini has been involved with Janssen-Cilag, The Binding Site, Gate Bioscience, Alexion, Protego, Argobio, Pfizer, Prothena, Sebia and Siemens.
References
- Sanchorawala V, Boccadoro M, Gertz M, Hegenbart U, Kastritis E, Landau H, et al. Guidelines for high dose chemotherapy and stem cell transplantation for systemic AL amyloidosis: EHA-ISA working group guidelines. Amyloid. 2022;29(1):1–7.
- Wechalekar AD, Cibeira MT, Gibbs SD, Jaccard A, Kumar S, Merlini G, et al. Guidelines for non-transplant chemotherapy for treatment of systemic AL amyloidosis: EHA-ISA working group. Amyloid. 2022:1–15.
- Kastritis E, Palladini G, Minnema MC, Wechalekar AD, Jaccard A, Lee HC, et al. Daratumumab-Based Treatment for Immunoglobulin Light-Chain Amyloidosis. New Eng J Med. 2021;385(1):46–58.
- A Study to Evaluate the Efficacy and Safety of CAEL-101 in Patients With Mayo Stage IIIb AL Amyloidosis. 2022. Available at: https://clinicaltrials.gov/ct2/show/NCT04512235.
- A Study to Evaluate the Efficacy and Safety of CAEL-101 in Patients With Mayo Stage IIIa AL Amyloidosis. 2022. Available at: https://clinicaltrials.gov/ct2/show/NCT04504825.
- A Study to Evaluate the Efficacy and Safety of Birtamimab in Mayo Stage IV Patients With AL Amyloidosis. 2022. Available at: https://clinicaltrials.gov/ct2/show/NCT04973137.
- Gertz MA, Tripuraneni R, Kinney GG. Birtamimab in Patients with Mayo Stage IV AL Amyloidosis: Rationale for Confirmatory Affirm-AL Phase 3 Study Design. Blood. 2021;138:2754.
- Edwards CV, Rao N, Bhutani D, Mapara M, Radhakrishnan J, Shames S, et al. Phase 1a/b study of monoclonal antibody CAEL-101 (11-1F4) in patients with AL amyloidosis. Blood. 2021;138(25):2632–2641.
- Valent J, Zonder JA, Liedtke M, Silowsky J, Kurman MR, Daniel E, et al. Safety and Tolerability of Cael-101 in Combination with Anti-Plasma Cell Dyscrasia Therapy in Patients with AL Amyloidosis: 1-Year Results from an Open-Label Phase 2 Trial. Blood. 2021;138:468.
- Gertz MA, Landau H, Comenzo RL, Seldin D, Weiss B, Zonder J, et al. First-in-Human Phase I/II Study of NEOD001 in Patients With Light Chain Amyloidosis and Persistent Organ Dysfunction. J Clin Oncol. 2016;34(10):1097–1103.
- Gertz MA, Cohen AD, Comenzo RL, Du Mond C, Kastritis E, Landau HJ, et al. Results of the phase 3 VITAL study of NEOD001 (Birtamimab) plus standard of care in patients with light chain (AL) amyloidosis suggest survival benefit for mayo stage IV patients. Blood. 2019;134:3166.
- FDA. DARZALEX FASPRO® Highlights of Prescribing information. 2022. Available at: https://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/DARZALEX+Faspro-pi.pdf.
- Vaxman L, Gertz M. Recent Advances in the Diagnosis, Risk Stratification, and Management of Systemic Light-Chain Amyloidosis. Acta Haematol. 2019;141(2):93–106.
- Ciberia MT, Ortiz-Pérez JT, Quintana LF, Fernádez de Larrea C, Tovar N, Bladé J. Supportive Care in AL Amyloidosis. Acta Haematol. 2020;143(4):335–342.
Developed by EPG Health. This content has been developed independently of the sponsor Alexion, which has had no editorial input into the content. EPG Health received unrestricted educational funding from the sponsor in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.
of interest
are looking at
saved
next event

