Surgery for HS
EADV 2024
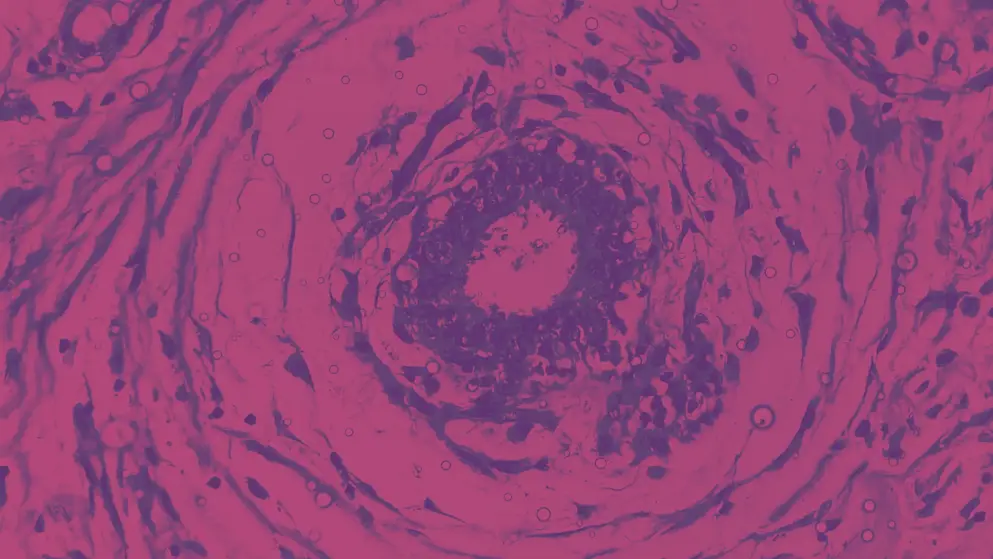
A systematic review and meta-analysis highlighted variations in recurrence of hidradenitis suppurativa (HS) associated with different surgical methods.
Kaiyang Li (McGill University, Montréal, Québec, Canada) and team included 32 studies with over 8,000 procedures performed on 6,992 people with HS.
For excisional surgeries, wide local excision was associated with significant 43% and 50% reduced risks for recurrence relative to limited local excision and to incision and drainage, respectively. The number needed to treat with wide local excision to prevent one recurrence was six.
For wound closure methods, simple primary closure was associated with a 24% reduced recurrence risk relative to split-thickness skin grafting. There were no recurrence rate differences between the assessed healing methods.
Another study, from Antonio Martorell (Hospital de Manises, Valencia, Spain) and colleagues, demonstrated the benefits of ultrasound-guided surgery, with no recurrence found among 122 patients over an average 22 months of follow-up.
EHSF 2024
Surgery for HS
Watch Professor Falk Bechara discuss the use of surgery in hidradenitis suppurativa (HS), including his thoughts on when surgery should be performed and the short-term future of the treatment landscape.
Professor Falk Bechara discusses the use of surgery in HS, including when surgery should be performed and addressing barriers. View transcript.
“After surgery, the story is not over.” Professor Bechara discusses recurrence in people with HS and offers his thoughts on areas of surgical treatment requiring further research. View transcript.
Professor Bechara shares his thoughts on the short-term future of the treatment landscape and stresses the importance of education in HS. View transcript.
This content has been developed independently of the sponsor, UCB Biopharma SRL, which has had no editorial input into the content. EPG Health received funding from the sponsor in order to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

