Allergic rhinitis
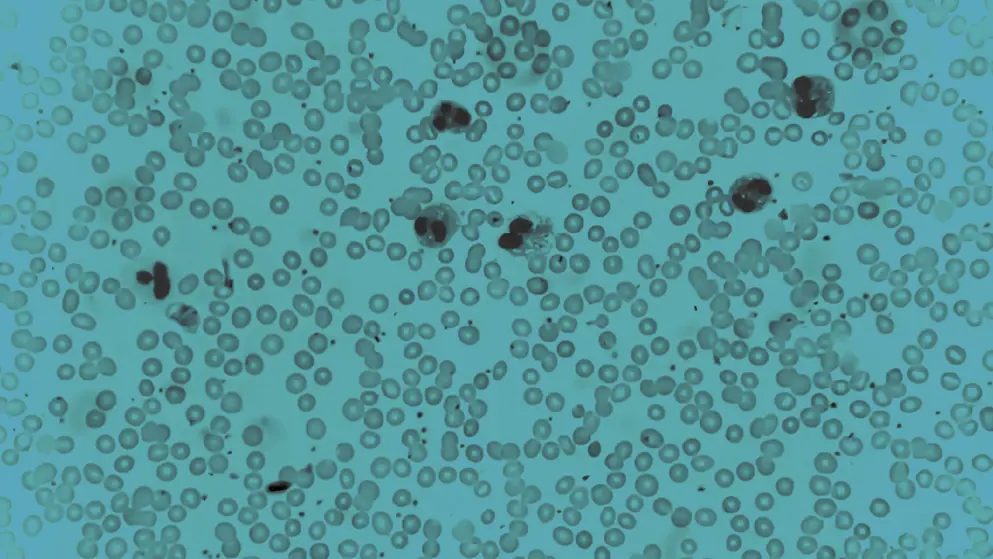
Allergic rhinitis is an immunoglobulin E (Ig E)-driven inflammatory disorder of the nasal passages, triggered by exposure to allergens such as pollen, dust mites, mold, or pet dander. Sensitization to these allergens provokes an abnormal IgE response in the nasal mucosa, leading to the release of histamine and other inflammatory mediators.
How prevalent is allergic rhinitis?
More than 400 million people globally are affected by allergic rhinitis, with a prevalence of 10–30% in adults and over 40% in children.
Who is most at risk?
Allergic rhinitis is caused by an allergic reaction and can occur in anyone. However, the likelihood of developing an allergy increases if family members also have allergies or conditions such as eczema or asthma.
How does allergic rhinitis affect people with the disorder?
Typical symptoms of allergic rhinitis resemble those of a cold and include frequent sneezing, nasal itching, nasal discharge, a cough, an itchy roof of mouth, and itchy, red, and watery eyes. Allergic rhinitis impacts quality of life, limiting daily activities, reducing productivity at work and school, and causing sleep disturbances.
Is there a treatment?
Self-management strategies, such as nasal irrigation and allergy avoidance techniques, are recommended prior to pharmacological treatment. First-line treatment options include intranasal corticosteroids and intranasal or non-sedating oral antihistamines, singly or combined. If there are additional eye symptoms, antihistamine eye drops or chromone eye drops can be used. In some cases, immunotherapy may be used to promote clinical and immunological tolerance.
Developed by EPG Health for Medthority, independently of any sponsor.

