Sodium Intake and Chronic Kidney Disease
Sodium Intake and Chronic Kidney Disease
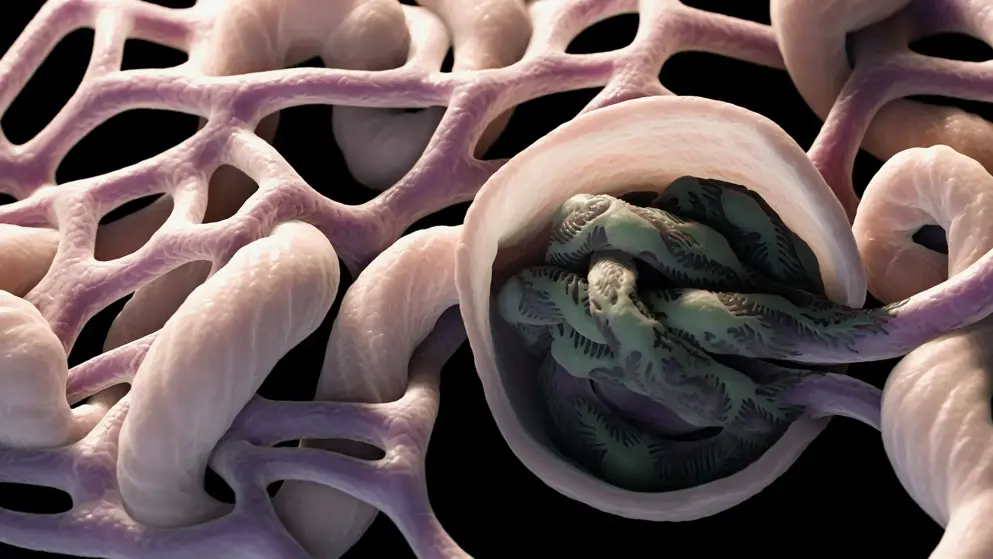
In Chronic Kidney Disease (CKD) patients, elevated blood pressure (BP) is a frequent finding and is traditionally considered a direct consequence of their sodium sensitivity. Indeed, sodium and fluid retention, causing hypervolemia, leads to the development of hypertension in CKD. On the other hand, in non-dialysis CKD patients, salt restriction reduces BP levels and enhances anti-proteinuric effect of renin-angiotensin-aldosterone system inhibitors in non-dialysis CKD patients. However, studies on the long-term effect of low salt diet (LSD) on cardio-renal prognosis showed controversial findings. The negative results might be the consequence of measurement bias (spot urine and/or single measurement), reverse epidemiology, as well as poor adherence to diet. In end-stage kidney disease (ESKD), dialysis remains the only effective means to remove dietary sodium intake. The mismatch between intake and removal of sodium leads to fluid overload, hypertension and left ventricular hypertrophy, therefore worsening the prognosis of ESKD patients. This imposes the implementation of a LSD in these patients, irrespective of the lack of trials proving the efficacy of this measure in these patients. LSD is, therefore, a rational and basic tool to correct fluid overload and hypertension in all CKD stages. The implementation of LSD should be personalized, similarly to diuretic treatment, keeping into account the volume status and true burden of hypertension evaluated by ambulatory BP monitoring.
Read abstract on library site Access full article