Genitourinary cancer
Genitourinary cancers are among the most prevalent malignancies in the USA, presenting a significant challenge to healthcare professionals due to their biological diversity and rapidly evolving treatment landscape. Prostate, bladder, and kidney cancers account for the majority of cases, with prostate cancer alone affecting over 3 million men annually. Advances in molecular profiling and biomarker testing have enabled more personalized approaches, particularly in prostate and bladder cancers. However, the high morbidity and mortality associated with metastatic genitourinary malignancies highlights an urgent need for new therapeutic options.
What are the most common types of genitourinary cancer?
The most common genitourinary cancers include prostate, bladder, and renal cancers. Prostate cancer is the most prevalent among men, with 12.8% diagnosed during their lifetime. Less common types include testicular, penile, and adrenal cancers.
What are the key risk factors associated with genitourinary cancers?
Risk factors for genitourinary cancers vary by cancer type but commonly include family history, smoking, age, race/ethnicity, chemical exposures, diet, and high blood pressure. Certain medications and herbal supplements may also increase risk for specific genitourinary cancers.
What are the key developments shaping the future of genitourinary cancer treatment?
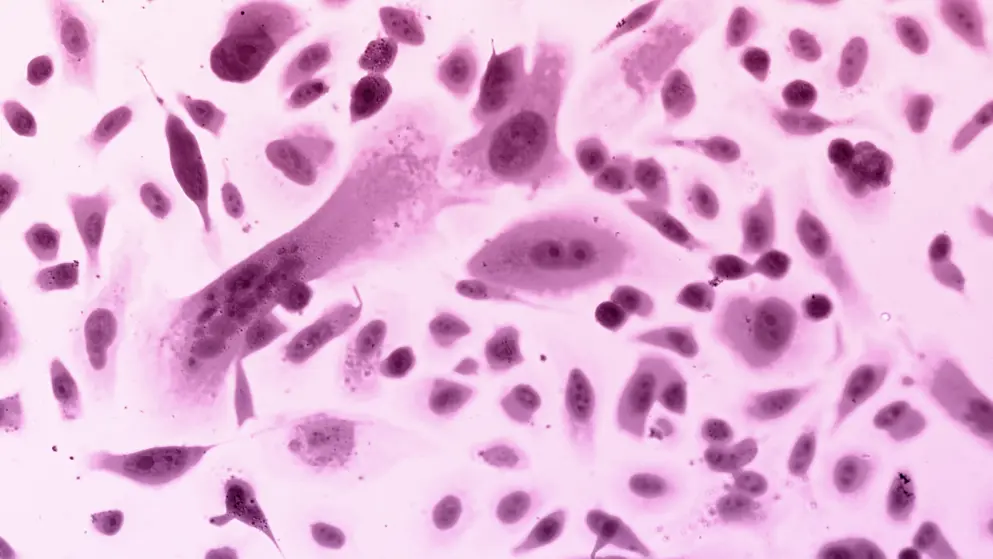
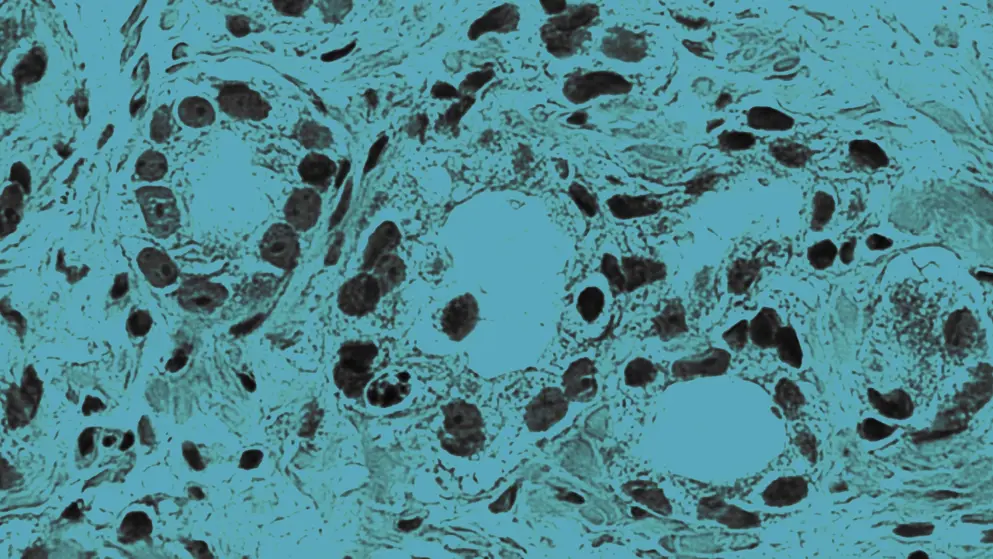
Genitourinary cancer treatment is evolving rapidly, driven by molecular-level insights and precision medicine. Advances in immunotherapy, targeted anti-angiogenic agents, and combination strategies are expanding options across multiple lines of therapy. A deeper understanding of tumor biology, oncogenic drivers, and the tumor microenvironment are enabling more tailored and effective interventions.
What are the limitations of current clinical trial designs in genitourinary oncology?
Despite new promising agents, many clinical trials in genitourinary oncology focus on proof-of-concept rather than direct comparisons. The lack of head-to-head studies limits clarity on optimal sequencing of therapies, leaving clinicians without level-one evidence to guide treatment decisions.
Developed by EPG Health for Medthority, independently of any sponsor.