Yescarta receives FDA approval as first CAR T-cell therapy for initial treatment of relapsed or refractory large B-cell lymphoma .- Kite/Gilead Sciences
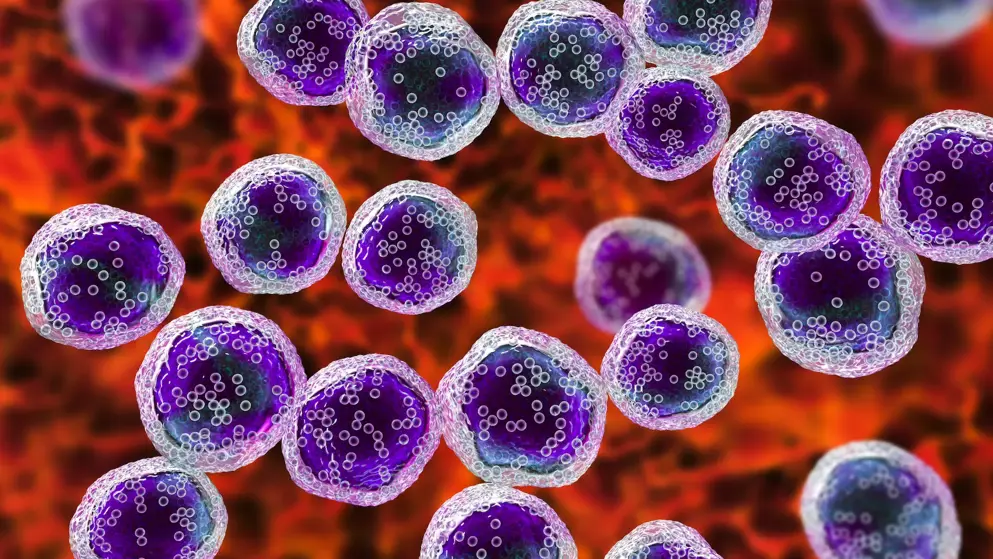
Kite, a Gilead Company announced the FDA has approved Yescarta (axicabtagene ciloleucel) CAR T-cell therapy for adult patients with large B-cell lymphoma that is refractory to first-line chemoimmunotherapy or that relapses within 12 months of first-line chemoimmunotherapy.
Yescarta demonstrated a clinically meaningful and statistically significant improvement in event-free survival (EFS; hazard ratio 0.398; P< 0.0001) over the current standard of care (SOC) that has been in place for decades. EFS was determined by blinded central review and defined as the time from randomization to the earliest date of disease progression, commencement of new lymphoma therapy, or death from any cause. Additionally, 2.5 times more patients receiving Yescarta (40.5%) were alive at two years without disease progression or need for additional cancer treatment, after their one-time infusion of Yescarta vs. SOC (16.3%), and the median EFS was four-fold greater (8.3 months vs. 2.0 months) with Yescarta vs. SOC.
Yescarta is also being reviewed by global regulatory authorities for additional indications inclusive of the ZUMA-7 patient population. ZUMA-7 is considered a landmark trial for being the first and largest trial of its kind, with the longest follow-up.
Earlier this month, the National Comprehensive Cancer Network (NCCN) updated its Clinical Practice Guidelines in Oncology for B-cell Lymphomas to include Yescarta for “Relapsed disease <12 mo or primary refractory disease” under diffuse large b-cell lymphoma (dlbcl) as a category 1 recommendation. yescarta is the first car t-cell therapy to receive a nccn category 1 recommendation. nccn defines category 1 as recommendations based upon high-level evidence with uniform nccn consensus that the intervention is appropriate.></12>
SOC therapy for this patient population has historically been a multi-step process expected to end with a stem cell transplant. The process starts with chemoimmunotherapy, and if a patient responds to and can tolerate further treatment, they move on to high-dose chemotherapy (HDT) followed by a stem cell transplant (ASCT).