Managing High-Risk NMIBC
Transcript: Unpacking NMIBC insights from ESMO 2025
Paolo Gontero, MD, and Ashish Kamat, MD, MBBS, FACS
Podcast recorded November 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- [Ashish] Hello, everybody, and welcome to "Expert voices: Navigating non-muscle-invasive bladder cancer." I'm Ashish Kamat, urologic oncologist at MD Anderson Cancer Center in Houston, Texas, and it's a distinct pleasure to welcome to the forum a friend, a colleague, an expert in bladder cancer, someone who sits on multiple guidelines, chairman of urology, Professor Paolo Gontero. So Paolo, welcome. - [Paolo] Oh, thank you very much, Professor Kamat. It's a great pleasure for me also to be here, and have the privilege to have a discussion with you. - [Ashish] So Paolo, you know, we're gonna be unpacking ESMO 2025. That's the title of today's podcast, and there was a lot that happened at ESMO, a lot that happened in bladder cancer, and one of the posters that was presented that was quite interesting was essentially on global BCG shortage and real-world challenges. So what is your take from, essentially, the real-world challenges in delivering BCG therapy for bladder cancer patients as it stands today? - [Paolo] Well, let's say that I'm happy to look to this study, which was a global survey on 2,000 patients of high-risk of non-muscle-invasive bladder cancer, so patients that should have received BCG.
I was especially quite shocked about these respective figures, because 40% of these actually did not receive BCG at all, and that was a study run in Europe. That's personally not my perception, because my institution, at least, and I think, in my country, all patients end up receiving BCG if they have high-risk non-muscle-invasive bladder cancer, unless for some reason they are actually candidates for radical cystectomy. But in that study, those who received BCG, only 50% received adequate therapy. From this point of view, I think that I can understand that, because a couple of years ago, we tried, actually, to collect a multicentric series, and what we found was that 50% of patients who should have received a full course of BCG with maintenance, actually, did not receive any maintenance. And what is really, really interesting in this study is that 50% of these patients in the global survey of 2,000 patients actually had an early discontinuation due to toxicity, of course, but there was also patients refusing to do BCG, and also, there was some shortage. But now, I think if you look at the reason why patients refuse BCG, it was because they were afraid to get a bacteria, a vaccine, and that's really underlying the lack of communication.
So I think that we should probably really, really make a lot of effort trying to improve the patient communication to avoid this misconception of BCG toxicity, and of course, we have also to keep in mind the excellent performance of BCG that was shown in recent Phase III trial where they compared BCG with combination of systemic immune checkpoint inhibitors, but really, indeed, BCG was fantastically effective. On the other side, I don't think that we can really do very much for BCG shortage. BCG shortage is not an issue, for instance, in my country, but it is an issue, I know, in USA, and I think that that should probably to find an effective alternative to BCG. - [Ashish] Yeah, Paolo, I think you raise very important points, and I would actually suggest that the issue of BCG shortage is something that is such a major pressing issue that it needs to be solved, and I think that the company that makes most of the BCG in the US, Merck, has publicly stated that they will have a plant that's up and running at the end of next year, and then hopefully we won't have a BCG shortage anymore. I think that's very important because of the points that you raise, because when BCG is given appropriately, it works really well, and it's important for us to educate our patients that just because BCG is a, quote, unquote, "older therapy," doesn't mean that they should be afraid of it, doesn't mean that they should be looking for newer alternatives, because the newer alternatives are not necessarily better, right? And they're more expensive, and of course, may even have more side effects. So that brings me, in some ways, to a perfect segue to a combination study, and you alluded to this a little bit. We'll touch upon three major studies, but let's focus on POTOMAC, essentially, first. This was a combination of BCG plus durvalumab.
As you know, De Santis presented this data, and the data suggested that there was a slight improvement in disease-free survival in patients getting combination of durvalumab plus BCG compared to BCG alone. So specifically to POTOMAC, and then we'll, of course, talk about CREST, which was BCG plus sasanlimab, where again, there was a slight benefit, in this case, to event-free survival in patients receiving BCG plus sasanlimab. So with the combination of the two studies, or if you want to discuss each one separately, what's your opinion? - [Paolo] Well, if we start with POTOMAC, who actually used the one year of durvalumab as a systemic checkpoint inhibitor combined with BCG with two years of maintenance, indeed, it was found out that compared to BCG only with maintenance, there was actually a marginal advantage. Actually, the advantage was significant, and the advantage was significant in, as you said, event-free survival, which I think event-free survival should be considered as a clinically-relevant endpoint, since it pertains a disease condition that, at best, would be considered BCG unresponsive. We should keep in mind that in this study, but also in the other study, where they used sasanlimab as a systemic checkpoint inhibitor, patient received an average of 14 installations, so they really received sufficient, adequate BCG. Now, if we look at POTOMAC, and we consider the magnitude of effect, which was reported as 32% reduction in the risk of having a high-risk recurrence, which, as I said, is a relevant endpoint, I think that we need to interpret this also in light of the impressive efficacy of BCG, because we actually had a disease-free rate in the BCG-only arm, which was 81% at two years, and it was 71% at fifth year, because POTOMAC has a relatively long follow-up, but that translated into a net benefit of about 5% and 9% event-free survival events respectively after two year and fifth year. So you know, 32% is okay, but it's 32% where the baseline effective for the control arm was actually around 80%, and those, we have to balance this advantage with the added grade 3 or more toxicity, which was predominately immune-related.
So we have to keep in mind that we have around 20% of grade 3 toxicity, which is immune-related, to get this advantage. So I think that hint of higher efficacy in a subgroup of so-called higher risk probably points out the fact that we would probably end up selecting, somehow, among the, let's say, quite broad population of high-risk non-muscle-invasive bladder cancer, those who may benefit of durvalumab in this respect. - [Ashish] Yeah, no, I agree with your points, Paolo. I think it's, again, like you said, it's important to emphasize that BCG works really well, and of course, when all of the studies who designed, whether it's POTOMAC, that you mentioned, CREST, ALBAN, which was a negative study using atezo, they were all powered to BCG results from the old days, but as we have discussed on this forum, and you have as well, with today's scopes, better diagnostic, better biopsies, better patient risk stratification, and better pathology, BCG works really well. So it's not surprising in all of these studies to see that the two-year event-free survival in the control arm was 80%, 83%, 87%, you know, it was really, really high, and that's why it was hard to show any benefit or any real major clinical benefit to the patients. I think the other thing that you mentioned is important to emphasize that the event-free survival was mainly powered by recurrence, and we don't know that this recurrence is actually clinically relevant to the patient, because it doesn't mean that the patient necessarily needs to have a radical cystectomy, because today, we have several different options available for patients to undergo, and of course, the results of KEYNOTE-676 will be very informative, because that's where patients get BCG and they don't have a robust response, and then you come in with the IO agent, which is pembrolizumab.
So if I could ask you, because you brought this up, if all of these drugs are approved, let's say, you know, CREST study, sasanlimab was approved, and durvalumab was approved, and you had access to those, do you know, based on the results of the studies, at least, which subgroup of patients you would consider for upfront combination therapy versus BCG alone? - [Paolo] Well, there was actually a slight difference on subgroup analysis, which as far as I know, in CREST, was somehow preplanned. So in the CREST trial, actually, the subgroup of CIS, whether it was pure or concomitant with a papillary disease, actually had the best hazard ratio, which was 0.5, and I think a combination of CIS with a papillary disease, particularly a PC-1 disease, according to the European guidelines, these actually define the very high-risk subgroup of patients, and this seemed to benefit the more about these citizens. So probably, I would think that in the end, the patients who might be considered for a broad combination will be those who are at very high risk of progression and those, that nowadays, we still consider for upfront cystectomy, although there is, anyway, a shifted paradigm. As you pointed out, we have a lot of rush to treatments.
We also know that being BCG responsive does not convey a significant risk if the patient is treated with conservative treatment. So I think that even in the very high-risk group, we should be more open towards conservative therapy, which, as far as we know now, should be primarily BCG-based. - [Ashish] Yeah, no, I agree with that. I think, you know, things are changing so rapidly, it's good to have so many choices for our patients. You know, on this topic of identifying very high-risk patients, you know, AI-based pathology is coming into vogue. There are studies here in the US, and published studies using the CHAI, C-H-A-I, platform. At ESMO, there was an AI-based pathology tool for FGFR detection presented. In general, I mean, you could talk about the poster specifically by Juan Ramon, but in general, what's your thought process for tissue availability, AI processing, conventional diagnostic methods? What do you think AI is gonna be?
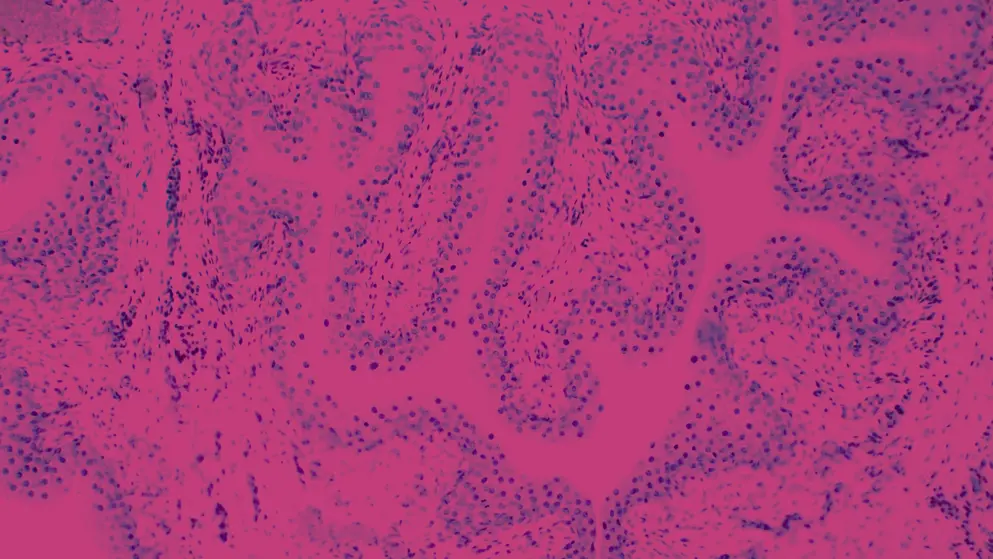
- [Paolo] Well, yes, it was interesting to see this AI-based study where they actually defined FGFR alterations based on AI, and of course, it was much less cumbersome, because by doing this, using an RT-PCR, they had to use more slides, and you know, thinking about, and also including the so-called genetic testing, which anyway, is going to play a major role in a treatment that she's making in the future, we are actually facing a dramatic improved workload for the pathologist, and we are moving towards a world, I don't know whether it's the same in the USA, we are actually having shortage of pathologists. So I think that this kind of AI-based digital pathology is going to become a standard of care, because otherwise, we would not be able to actually face, to counteract what is really, really the amount of workload. And the same was true for this very nice genetic profiling and immune-related profiling of the patients that received TAR-200 alone, and these were patients patients treated in the Arm 2 of the SunRISe-1 study, and again, they did a lot of genetic profiling.
It was only based on a subgroup of patients, 63 patients. There was really no relation between any specific mutation burden or genetic profile in general with treatment response, but this doesn't really mean that this is not the way to go. I think that in the future, ideally, any clinical study prospective, or whether it's randomized, should actually report as a secondary analysis also a correlation with genetic profile, because this will be the only way where we'll be able, in the future, to pave, really, the way toward a more personalized approach. Everybody's talking about personalized treatment, and I think this kind of genetic relation with response are actually the way to go, and that's the only way, actually, where we will be able to make a breakthrough to the so-called correlation, clinical correlation, of genetic profile of non-muscle-invasive bladder cancer. - [Ashish] Yeah, and I think personalized medicine is extremely important, and in order for us to do better personalized medicine, as you mentioned, we need to have trials at least build in, even if they're not powered, build in analyses upfront to allow us to look at subgroups and molecular markers, and you know, urine utDNA, ctDNA, imaging, all of that different stuff or different markers are very important. Now, talking about markers, of course, you know, one of the markers that has been studied in bladder cancer is HER2, and we know this from systemic disease, we know this from localized disease.
We also know that HER2 correlates pretty significantly with micropapillary bladder cancer, which falls into the very high-risk category, both at the AUA and the EAU risk classifications, so it was exciting to see the results of the Formula-01 study, which essentially used disitamab vedotin, which has been studied and reported in metastatic patients, but it's also used in a Phase II study with BCG in patients with non-muscle-invasive bladder cancer that were HER2 positive. What's your take on what this means moving forward? Do you think it's something that you would like to see expanded? What are your implications? Or what are the implications of the study from your perspective?
- [Paolo] Well, I certainly read it with a great interest, the presentation of this study, disitamab vedotin combined with BCG. In those, actually, it's a 30% probability that high-risk non-muscle-invasive bladder cancer will over-express the oncogene, HER2, and that was a Phase II, single-arm study, and I think that there are several attractive points of strength in this study. First of all, early oncological outcomes with one year disease-free rate exceeding 90% are certainly promising considered that we are talking about the high-risk cohort of non-muscle-invasive bladder cancer that are known to be resistant to BCG, more resistant to BCG because of the HER2 expression. The treatment is, of course, delivered to a selective group of patients to target the mutation using a marker-driven, personalized approach, so we are, in this way, potentially minimizing overtreatment exposure to patients, but while this data are promising, they need to be interpreted with caution due to the short follow-up. There are potential biases related to a single-arm design.
For instance, the cohort has some favorable feature in this way, because if I remember well, there was only an 11% of CIS, considered that these are high-risk diseases, and of course, I think that we lack robust data on BCG resistance of HER2 expression in non-muscle-invasive bladder cancer. So I think that a control arm in dissecting of an RTD is probably mandatory to interpret the real and the true efficacy of gaining a drug that has some toxicity. Notably, it was reported that the majority of toxicity was grade 1 and grade 2, but think about alopecia. Alopecia was affecting 50% of the patients in this trial, and I think that it might have, actually, a dramatic negative impact in our non-muscle-invasive bladder cancer population that used to receive only chemotherapy that do not really convey systemic side effects like alopecia. When we say to the patient, "We're giving you intravesical mitomycin," we say, "Don't worry, it's not going to be absorbed. You will not develop alopecia." So this is going to be a change in paradigm if we think about these new combinations, and I think we have to be very, very careful the way we interpret systemic side effects of treatment in a population of non-muscle-invasive bladder cancer patients. - [Ashish] Again, Paolo, you raise excellent points. It's always a pleasure to have you to discuss anything and everything related to bladder cancer. Thank you so much for taking the time to join us and unpack all that happened in non-muscle-invasive bladder cancer at ESMO 2025. Stay safe, and hope to see you soon. - [Paolo] Thank you, thank you very much, Professor Kamat. It was a real pleasure to have the opportunity to run this great discussion with you. Thank you.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

