Managing High-Risk NMIBC
Transcript: Diagnosis: Which tools should be used when?
Morgan Rouprêt, MD, PhD, and Ashish Kamat, MD, MBBS, FACS
Podcast recorded July 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- [Ashish Kamat] Hello, everybody, and welcome to "Expert Voices: Navigating non-muscle invasive bladder cancer." I'm Ashish Kamat and today I'm joined by Professor Morgan Roupret who really needs no introduction. Roupret is a well-known entity in the field of urology oncology, leads multiple efforts including editor-in-chief of urology oncology journal, and is a dear friend. Morgan, welcome to the podcast.
- [Morgan Roupret] Thanks a lot. I'm super happy to have the opportunity to discuss with you. - [Ashish Kamat] So Morgan, we're gonna tackle several topics, right? But the first one we're gonna tackle is essentially diagnosing non-muscle invasive bladder cancer and which tools should we be using. So when you consider a patient that is sitting in front of you and you're trying to make a diagnosis of non-muscle invasive bladder cancer, how do you approach that? What are you thinking in your mind? Are you gonna do cystoscopy? If you're gonna do cystoscopy, what type of cystoscopy et cetera. Walk us through that a little bit.
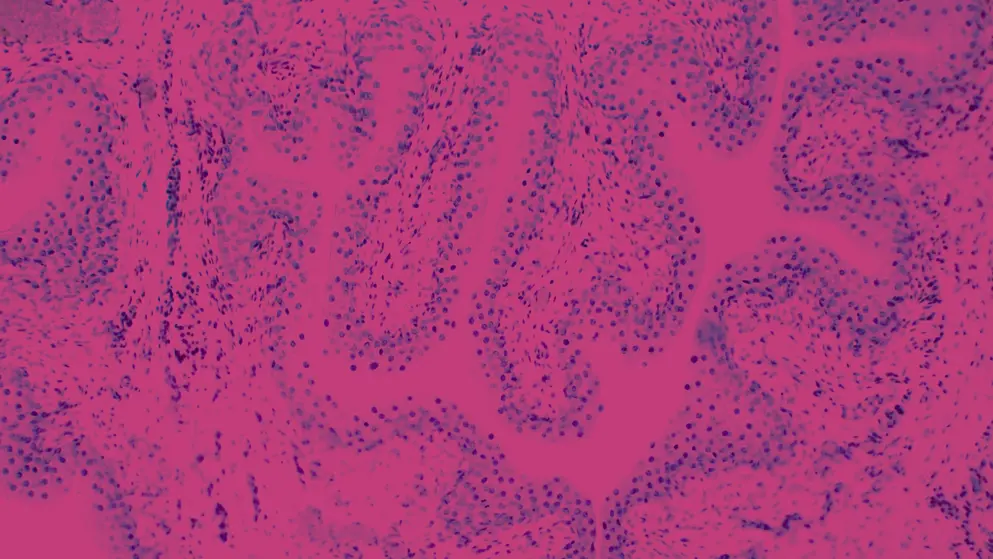
- [Morgan Roupret] Actually, Ashish, it's a good point because I know that many patients are referred to our centres with a positive diagnosis, which has already been done. As far as I'm concerned, I like to do my own bladder mapping. So, this is why I go into the bladder reservoir to see what's going on there to depict the number of tumours to assess whether or not there is a suspicion of CIS. So, I think it's very important to have the vision. I have also some patients who have been referred with an ultrasound and it was a median lab. And if you put the patient in the OR, and it has nothing to do with the bladder cancer, you look ridiculous in front of the anesthesiologist. So, I think that as a urologist and I only trust what I can see, what I see and I always do a cystoscopy which is mandatory and will help me to select the tools that I will use in the OR and that could enhance the visibility. If I consider from the beginning that the patient is likely to belong to the group with a high risk tumour, high risk of records and progression, then I need to optimise as much as I can my next step, which is the TURBT.
- [Ashish Kamat] Yeah, and that's a very important point that you brought up, which I think is key because you know, if patients are referred with just an ultrasound or something else or even an incidental MRI, you can sometimes see a prostate lobe. And if you just take the patient to the oR, then you subject the patient to anaesthesia, which is, you know, really not good for many of our older patients. So, I'm glad you mentioned that one of the first things to really do is to take a look in the bladder with a flexible cystoscopy in the office. Do you use any particular technique with your flexible cystoscopy? Any tips there as to some of the younger folks that might be listening- - Oh, the thing that the way we do that has changed because before the COVID-19, we are a bit limited in the numbers of I would say cystoscopes that were available and the single use cystoscope market has been expanding a lot. So, it's very convenient and actually, I mean a big hospital with a big area and sometimes there is no way the patient is likely to come to the office, so we can come to the bed to the, of the patient and to do the cystoscopy. So, what I see is that the quality of the flexible cystoscopy, single use cystoscope is as good as it is for the, I would say, pure diagnosis description. And the only announcement of visibility that I would use is in the OR when I think about the blue light cystoscopy, or when I think of NBI, or these tools are only in the OR as far as we are concerned.
- [Ashish Kamat] So tell me Morgan, you know, I use blue light when I'm really trying to look for tumour in a patient that has say a positive cytology and nothing seen or when I'm doing a resection in someone with multiple papular tumours, because I'm trying to see all the small little tumours in the bladder. Do you use blue light in every patient or do you select the patients? - [Morgan Roupret] Actually, I select the patient. It was used to be reimbursed massively in Europe before. It's not the case anymore. So, it's at the cost of the hospital or the medical where you are practising urology. So, we use it on taking time but as you mentioned, we select as much as possible the patient. And I think it's good to go back to basics and you mentioned the positive cytology. And when you look at the survey about the practising neurologists, there is minority of urologists, who are indeed requesting a cytology before the TURBT. And I think any positive cytology or multiple tumours are a good criteria to select the patient who are suitable for the blue light cystoscopy. So, we use it in one third of our patient roughly.
- [Ashish Kamat] Yeah, now speaking of cytology, you know the quality of cytopathologists or those that doing cytology dedicated bladder has drifted across the world and many places don't trust their cytopathologists, which is why now there are multiple biomarkers that are constantly being used. Here, you know, in our practise we still trust our cytopathologists. We don't really use ancillary biomarkers. But what's your practise, what do you do with biomarkers?
- [Morgan Roupret] Biomarkers is very interesting because the pathologist can be sick, can be indication, especially in Europe. So, I trust my pathologist who used to be the comparable. She moved to another country. So, we are at a moment in time where it is true that there is a huge discrepancy between observers and pathologists and it is, I believe, a good cytology done by a good pathologist appears to be and to remains the standard. But the reality is there are so many companies that are coming on the market with new markers, methylation markers, DNA/RNA markers. So, we have open at the national level in France a registry, prospective registry to evaluate these markers. It's not a marker. It's a panel usually of markers that you are going to use. The question is whether or not these markers are similar in terms of detection, diagnosis, or for the follow up and even the follow up of low grade or high grade. So, I do believe there is not one just single panel that is going to be useful. But maybe according to the stratification of the tumour, the situation where you are, you will be more keen to use these markers or those markers. At the moment, I'm just saying that it is under evaluation. The particularity of these markers is that they are using the technology I would say is not ready for prime time, but we don't know in which setting we should use that. The two questions that are arising is for the diagnosis and we see screening in a targeted population or for the follow up and probably not the same brand of markers. There are several companies there. There is no head to head comparison. So the only situation we had, we signed with the French Association of Urology and this companies the possibility to evaluate it prospectively. So, we have it for free and we are, we have been starting to enrol patient in the huge registry over 35 centres in France. And we expect to enrol a lot of data and patient and to have a clear vision of the situation, where we could implement the marker to maybe decrease the number of cystoscopies in the follow up. So, it's surely interesting. Not yet ready to give you a strong statement on which one should be the one for the follow-up or the diagnosis.
- [Ashish Kamat] You know, I think that's very astute of you to do that because there are so many markers. They don't really make it into the guidelines because there's evidence, but it's not enough to be recommended for all patients. So, selecting the guideline for the right patient I think is something that is the art of bladder cancer management, right? And that also brings me to now imaging as an adjunct for staging. There's a lot of interest in using imaging to replace what you and I do. You know, there are some groups that are saying you don't need to do a TURBT. You can use MRI to give you the T stage for the bladder cancer. I think that the good resection and a good pathology is still key, but there are people that are saying that you don't need that. You can use MRI. What are your thoughts there?
- [Morgan Roupret] Now, I think there are medical legal issues there and we need to bear in mind that the TURBT is not only there to perform a diagnosis, but also to cure the patient. And BCG or chemotherapy in the bladder is just adjuvant treatment. The main treatment is endoscopic surgery. So, I believe there is a role for imaging. And going back to the initial words of this discussion where we said that the positive cytology beforehand or multi at the diagnosis, cystoscopy is likely to trigger sometimes pretreatment workup before the TURBT to check on the peri-urinary tract, to check on the nodes and so on. Sometimes when it's a small spot of tumour and I believe from the beginning that I will be addressing a very low risk disease, I will do I would say the imaging after the TURBT. So, the way I will organise the path of the patient and the prescription is going to be really influenced by the first division of the tumour and the bladder reservoir. But I believe that I know about the study of my colleagues in England and Nick James about the fact that you could keep just do a biopsy or cytology and maybe skip the TURBT. But I believe it's a bit dangerous to go into that direction at the moment. Endoscopic surgery is real surgery is I would say if I want to be provocative a bit, I would say it's more or less a partial cystectomy, you know, endoscopic partial cystectomy. And so, it has nothing to do with just believing that bladder cancer is going to be cured by intravesical drugs or systemic drugs and there is an action of the surgeon. And I don't want to go into any misunderstanding from that perspective.
- [Ashish Kamat] Yeah, I think that's a practical issue because you know, when you're looking at systems such as in the UK where they're trying to streamline the patient's pathway from diagnosis by the general practitioner to the healthcare mandate, that timelines, that's where that MRI sort of comes in handy. And if you look at the data, it only enhances the patient's time to radiation or the patient's time to palliative care but not to cystectomy, not to intravesical therapy. So, I think absolutely right, when you're looking at streamlining both the diagnosis and promoting equity and amongst patients, it's really important to keep in mind that what is good for your place or my place may not be true in all populations. And maybe something like an MRI might help in a place where they don't have good enough surgeons, right, or they don't have good enough urologists or that timeliness. But if they have good access to folks like yourself, I absolutely agree. I think the patient should have visualisation of the tumour and resection of the tumour and I'm glad you made that statement. But that brings me to an interesting point, Morgan, where do you think there are gaps between what you and I would recommend, right? We sit on multiple guidelines panels. We publish, and we say, "This is what's in the guidelines." But then you have the reality. You have people that are seeing patients in small countries where they don't have enough resources or even in a large country where they're just not interested in bladder cancer. They have so many other things that they have to do. Where do you see that disconnect between what you're recommending and the bare minimum quality that someone should be applying? Like how do you advise someone there?
- [Morgan Roupret] No, I think you have a strong point and in the field of gene cancer when it comes to bladder cancer compared to prostate cancer, kidney cancer, the field where our colleagues are not following the guidelines is bladder cancer, because there are so many steps and there is a schedule and we have to be flexible. All along, I would say the natural story of the disease, the recurrence, the progression, so the ability to adapt, to understand the disease and to have a good, I would say discussion with the patient is going to evolve. It's a chronical condition. So all along the way, we are losing patients but we're also losing colleagues that are I would say becoming a bit trying to I would say skip some steps. And it's absolutely fascinating to see that finally we are looking at the new data in the field of metastatic bladder cancer and so on. The vast majority of our patient in the western world, our localised early bladder cancer and the way we need to discuss about optimization of of the bladder, of the good I would say schedule for the instillation, the choice of the instillation, it's absolutely mandatory. There is a lot going on because the pipeline is very rich and many, many pharma companies are coming, which means that they should bring to the market new drugs, but they bring also a lot of money, a lot of interest, and a lot of science because behind any trial that is in the pipeline of non-muscle invasive bladder cancer, there are ancillary data, better understanding. So, I understand actually with your group IBCG, AUA, EAU, and so there are some discrepancies I would say on endpoints definition of refractory patient. But all along the way, the way we should treat the patient is more or less the same, but we have to be highly motivated to treat these patients. And if you are not well organised in your practise, if you don't consider that bladder cancer is an emergency, then you should definitely skip and focus on I would say is it one prostate cancer for active surveillance, because bladder cancer is really a matter of organisation. And you mentioned, we mentioned the trials in the UK, but during a long period of time, bladder cancer has such an influence on the healthcare system of the UK, because people were complaining about the fact that they were queuing, waiting list, and so on. And because of bladder cancer, it has to be changed and reorganised. So, I think it's a major problem and it has been an orphan disease for many, many years in the field of urology, but the picture is changing dramatically and for sure in a better manner for the patients and for us.
- [Ashish Kamat] Those are great points, Morgan. You know again to summarise everything for our listeners, walk us through now a assimilation of everything that you just said. You have a patient that comes to you, is sitting down, and you are trying to make a diagnosis on that patient. Let's assume it's a 63-year-old female that comes to you with gross hematuria. Just walk us through the best way to make a diagnosis in the opinion of Professor Morgan Roupret.
- [Morgan Roupret] She would definitely undergo a cystoscopy as we mentioned. She will meet immediately after the positive visual diagnosis, the anesthesiologist and she will be scheduled to the OR very rapidly, which means that it is not within one month or two months and so on. And if the OR is very busy, I will make room for her. So, which means that of course we have some patients with some comorbidities and so on. So we don't want to skip the mandatory I would say pre-surgical workup if necessary, if she has anticoagulants and so on. But she has to be scheduled within two weeks. And thereafter, we'll send the sample to the pathologist of course immediately. But if I feel, because I will not have the feedback from the pathologic immediately, if I feel that the patient is likely to be a T1 high-grade, for instance, she will be immediately scheduled for a second look TURBT.
And if in between I received a report saying that I was wrong and it was a TA of low grade, which can happen from time to time, I will cancel this second surgery. But as I said from the beginning, it's a question of organisation and go back after the, immediately after the surgery to tell to the patient, "Look, I removed entirely the tumour. I didn't do a biopsy. Your bladder reservoir is clean. But now, we need the assessment of the pathologist to know whether or not the muscle has been touched is very important." And I would like to go also to the imaging. I will request an imaging at some time in the history of this patient to see the tract. But what I told you initially is if I feel that the patient is a regular non-invasive bladder cancer, then I can organise a CT urogram within a few weeks after the surgery. If I feel that it is invasive from the beginning and that after the clinical exam, I'm afraid that we are facing a muscle invasive bladder cancer situation, then I will request some imaging before the TURBT and probably try to to get an MRI. From the positive and the pathological assessment, then we will decide about the adjuvant programme of instillations. - [Ashish Kamat] That's a great comprehensive way and a very inclusive way to take care of patients. Morgan, thank you for your insights. This was a very rich and practical discussion and it brings us to the end of this episode. But to our listeners, stay tuned. And until then, thank you for joining, "Expert Voices: Navigating non-muscle invasive bladder cancer." - [Morgan Roupret] Thank you.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.
Updates in your area
of interest
of interest
Articles your peers
are looking at
are looking at
Bookmarks
saved
saved
Days to your
next event
next event

