Managing High-Risk NMIBC
Transcript: A patient’s view on NMIBC care pathways
Douglas Cappiello, MD; Camille Cappiello; Ashish Kamat, MD, MBBS, FACS
Podcast recorded November 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- [Ashish] Hello, everybody, and welcome back to "Expert Voices: Navigating non-muscle-invasive bladder cancer." I'm Ashish Kamat, urologic oncologist at MD Anderson Cancer Center in Houston, Texas. And I'm joined today for our part two of the patient and caregiver perspective, very important perspective, by Douglas Cappiello and his wife, Camille Cappiello. Douglas is a retired physician and a bladder cancer survivor, and Camille is a nurse and, of course, a carer. So Doug and Camille, we talked about your experiences leading to bladder cancer diagnosis in episode one, and now in part two, we are gonna be talking about shaping care pathways following bladder cancer diagnosis through navigating treatment discussions. With that in mind, and you know, folks have already listened to the diagnostic part of it, so you had your diagnosis, it was during a difficult time, COVID, which helped you in ways that it didn't help others, because you got to your diagnosis sooner. But with that background after your diagnosis, how did conversations about treatment begin, and how did they actually make you feel at that time? You know, recognizing now in 2020, there weren't as many options as might be available today, but with that perspective in mind, walk us through your conversations with your care team and the different advice that you received.
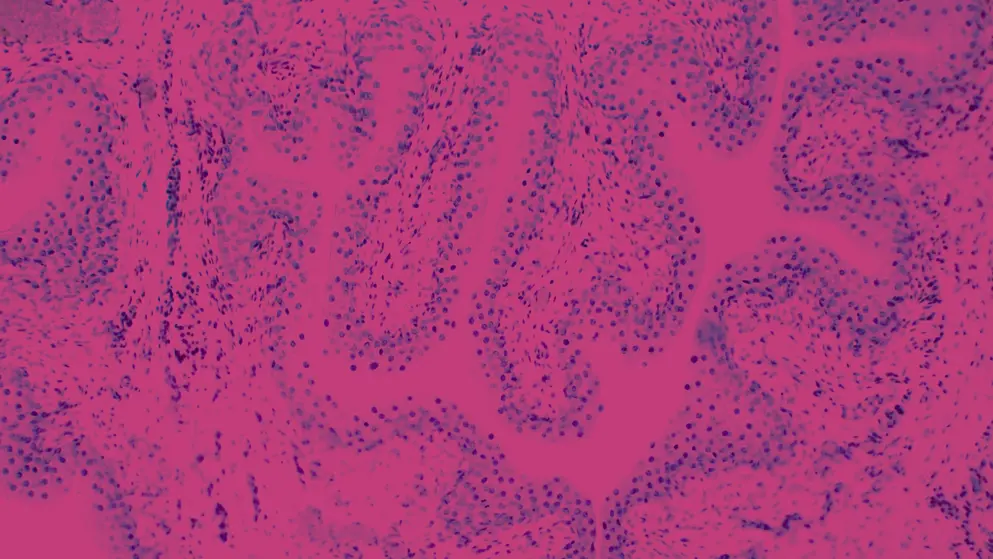
- [Douglas] Yes, thank you. So, as you mentioned, I was diagnosed with stage T1, high-grade non-muscle-invasive bladder cancer with CIS, and after that diagnosis was made with a confirming TURBT, there was a brief discussion with my urologic oncologist about going directly to radical cystectomy, as you so stated, there weren't that many other options at that time. But instead, she recommended a six-week induction course of BCG. My surgeon stated, this is standard of care for high-grade non-muscle-invasive bladder cancer, has a good chance of success with little risk of progression in the short term. I asked for some, you know, extra materials to kind of review the standards of care, and she referred me to the 2020 NCCN and AUA guidelines for non-muscle-invasive bladder cancer, so I could feel confident with the standard of care. And this really helped me understand what options were available, which, as you stated, were unfortunately very limited in 2020. I began a six-week induction course of BCG around June 2020. Great anticipation that it would be successful, and I felt fortunate my institution was able to obtain full-strength BCG during my induction course in spite of the worldwide shortage. But most other patients we've spoken to at this stage received similar treatment, although many were worried because they received diluted BCG or had to try other intravesical treatments entirely due to the shortage. And unfortunately, most patients are like a deer in the headlights during their doctor's visits, and they often don't understand much of what the doctor was saying. Is another reason why it's so critical to encourage spouses, caregivers, family members, or friends to accompany them to appointments.
- [Ashish] You know, I absolutely agree. I think, you know, there's been a BCG shortage across the globe, but especially in North America since 2014, when one of the manufacturers of BCG decided not to go ahead with making BCG for various reasons, which we won't really go into. But since then, since the BCG shortage, there has been a surge in patients being recommended and choosing radical cystectomy because even today, BCG really works better than anything else we have. And sometimes patients get confused, or they get misinformed about BCG and are told that it's an older drug, so don't try it. Let's try something new. But it really works really well. And you know, with that in mind, I also want to probe a little bit into your thought process because I think factors that you consider as a patient when you're deciding on a treatment plan, given all the information you had, you mentioned in the earlier episode of this podcast that the pathology slides had to be sent somewhere else, and that's what led to the diagnosis of CIS in addition to T1, which clearly puts it in a very high-risk category. And I'm sure that factored in a little bit in your decision-making. So, share with us a little bit, what factors were most important to you as a patient when deciding on a treatment?
- [Douglas] Well, there was only one thing important to me during treatment, and that was survival. And I was willing to go through whatever it took to stay alive. Therefore, I wanted to make sure the risk of recurrence, and especially the risk of progression, was very low. I was willing to deal with side effects, discomfort, long recovery times to meet that goal. Most other patients feel the same way. And I know many who went directly to RC without even trying BCG, and this is mainly due to those who have high-risk cellular variants like micropapillary and things like that. But we have come across some people who feel strongly that they want to keep their bladders, and they're willing to take on various amounts of risk in order to achieve that goal. And as you stated, there are fortunately newer drugs that were not available when I was diagnosed that make the playing field much more encouraging but also much more bewildering. These new drugs, they have very complex mechanisms of action, they produce varying success rates, and there's a lot of terminology, you know, complete response rate, disease-free survival, overall survival, progression-free survival, it goes on and on that are used with these medications that patients can't understand. I think for this reason, it's critically important for physicians to understand that most patients only wanna know a few things. What is the chance of recurrence in the first 12 and 24 months, and what is the chance of progression to muscle-invasive bladder cancer? And I think those are the two questions that really need to be answered whenever you are discussing treatment options with your patients.
- [Ashish] So, I couldn't agree more. I think it's very important, and that's why, you know, one of the first questions I will always ask a patient sitting in front of me is, "We'll get into the discussion, but what's the most important thing in your mind right now about your diagnosis, and what's the most important thing you are trying to attain? Because what's important to one patient is not important necessarily in the same priority to somebody else, right? And we may think that, for example, not doing a bladder removal is really, really important to a patient. But like you said, if your ultimate goal is survival, then removing the bladder is a price to pay, but you're willing to pay the price because you want to actually be alive and not have to worry about the recurrence. So it's very important, like you said, for us on the physician side to actually understand what's most important to you. Share with me a little bit about your experience from the emotional side of things during the treatment phase, understanding the nuances of different options, the ability of the different options to affect your work, travel routines. How did you kind of factor that in your selection of treatment?
- [Douglas] Well, again, as I mentioned, BCG was certainly the standard of care at the time, and it still is, as I understand it. And BCG induction from a physical standpoint was relatively easy for me. The only hard part was that I had developed a meatal stenosis, which sometimes made it difficult for the urology nurse to pass the catheter to instil the BCG, and it was always very painful for me. But other than that, I did very, very well, and I had very few side effects from BCG, which made me worry that the BCG was not working and not initiating a good immune response. So please let physicians know that patients worry about everything, even lack of side effects. (Camille laughs) From an emotional standpoint, though, I will say it was a very difficult time. The weekly intravesical instillations took precedence over all my other life priorities, and I was often distracted and worried. And after completing the six-week course, my surgeon arranged a follow-up blue light TURBT about four weeks later, and I worried constantly about how that would go. So I guess the main term is worry. There's a lot of it.
- [Ashish] Yeah. No, and again, you're alluding to certain points that are really near and dear to my heart because I think it's really important to let patients know what to expect from their treatment and to let them know, do side effects... Are they good? Are they bad? How to deal with side effects. And, you know, again, just to clarify for folks listening, till today, nothing has beat BCG as treatment of choice for patients that present with what you had other than removal of the bladder. So you're absolutely right. Even today, BCG is still a gold standard, and just because it's something that's been around for 30, 40 years, will sometimes have patients ask, "Is there something newer? Is there something better than what's been around for 40 years?" And I often have to sit and set expectations, saying, "Just 'cause it's old doesn't mean it's not good," right? Because it really works well. And like you said, patients don't often wanna challenge their physician because they feel that they'll let their physician down. So I totally agree with that, the comments that you've made. Now, what kind of support do you think would've made a difference as far as these side effects that you're thinking about or symptom management? I mean, I know you talked about you being worried, but would you have found it easier to deal with this, say, if somebody had recommended online resources other than BCAN, such as apps or digital tools, anything like that?
- [Douglas] Well, I had a wonderful care team to work with. You know, one of the things that people don't think about is how important the other members of the team are. We had an amazing nurse that works in our urology clinic. She performed all my intravesical instillations, and she provided such compassion and empathy. She focused on my comfort and support. Both she and my surgeon were great at responding to questions and concerns, either by phone or secure messaging using the MyChart program, which I think most institutions are using today from Epic. We both continue to stay engaged with BCAN. We made use of the Inspire website to stay abreast of things and speaking with other survivors and caregivers. There were written handouts, after-visit summary. So I think we were very well informed, but we know it takes a significant effort on the part of healthcare providers to prepare all these written materials. But we wanna say in the long run, the effort is worthwhile and much appreciated, and it's actually a time saver for busy clinicians by eliminating many of the phone calls they would've otherwise received. So I think it does require a lot of preparation on the part of healthcare providers to take care of bladder cancer patients, but the effort is worthwhile.
- [Ashish] Well, thanks. Thanks for stating that, because oftentimes you'll feel or hear that, well, there's so much effort being put into X, Y, and Z, and is it appreciated by patients? And I know that it is, but I'm glad you brought that up because folks listening in really should not feel that it's not appreciated or noticed. Camille, you were Doug's caregiver throughout this journey and, of course, have supported others with their volunteer work. So, from your perspective, from a caregiver's perspective, or a carer's perspective, what are some of the most important roles that you and others could play, and what do you think healthcare providers, physicians, nurse practitioners, physician assistants, everybody, pretty much as part of the team should understand about involving caregivers in the patient's care?
- [Camille] Thank you, Dr Kamat. I think that the caregiver is actually an integral part of the entire care team for the patient. And I think it's important for the team to understand the relationship, you know, that the caregiver brings, because it's usually a spouse, but often it can be, you know, a sister or a brother or, you know, good friend, other, you know, close significant other. And so understanding that relationship, really good communication with the caregiver, I would say validating, you know, just their presence in their role, understanding that they do bring, you know, an extra set of ears, and listening carefully, and can also sometimes share concerns that the patient might be having that the patient themself cannot articulate. You know, it's important for the caregiver to get permissions, you know, from the patient as far as like HIPAA clearance and medical information, and who is gonna be that go-to person, specially if, you know, there's an unforeseen event, and how are they gonna access information so that they continue to properly advocate for the patient, trying to have the healthcare team join them where they're at in really heartfelt listening and appreciating their story and what the goals are. You know, as you have shared earlier, you know, the patient's desire in the decision-making of next steps and how we can all work together. Having a trusted confidant is so important. Sometimes the caregiver is overwhelmed and distraught. They're trying to help, you know, their loved one, and they don't always get full cooperation. (laughs) And so sometimes they have to bring in some fierce compassion, if you will. And it's important for them to have a trusted confidant in the office. And I spend a lot of time helping other caregivers understand, you know, that they're doing the best they can and that it's okay for them to call if they have questions. And is there someone in the office that they felt like they connected with, who they can trust, who they feel would be a good liaison, let's say, to the physician or nurse practitioner, PA. I have one patient who really, really built a great relationship with an office manager, and she actually ended up being an incredible advocate for this caregiver. And it all worked out. But again, you know, sometimes there's a lot of fear, as Doug mentioned earlier, and they don't want to sort of disappoint anybody in the office or, you know, quote, "be a problem." Sometimes they feel like if they're questioning things that, you know, they're gonna be judged. So I think it's really important that people are just listening really carefully, that they're consistent in their responsivity, and also timely in their responses, because the caregiver is also alongside the patient. They carry that suffering with great compassion, and they know they can't fix it, but they can be very helpful in soothing some of the patient's concerns just by getting the support and the answers that they need from the healthcare team.
- [Ashish] Thanks so much for sharing that. I couldn't agree more. And from my perspective, I always feel, and I get the caregiver involved early on, because I truly think that getting the whole team together, and I mean team now, not on my side, but the team on the patient's side, helps improve outcomes. It helps improve the ability of the patient to deal with complications. It helps the patient's ability to deal with difficult decision-making. There is no stigma, there's no bravado. Sometimes we'll see where men don't want to admit to their wives or children... You know, again, disclosing to young kids a separate issue, but otherwise, adult children getting them involved is very, very important, very early on. And it really helps. In my opinion, I think it's as important a predictor of good outcomes as any of the drugs or other things that we might be using. So I think it's really very important that these people listening recognize that physicians really want you to be involved. And I can't imagine any physician not wanting the caregiver to be involved. And if it appears like that, it probably is just, you know, a miscommunication on the part of the physician. So thank you for bringing all those points to the forefront. In closing, Doug, I'm gonna switch back to you as the patient. You've alluded to a lot of this already, but in summary, for those listening, patients and caregivers, and healthcare professionals, what would you give to us as physicians, and also patients and their families listening in, as far as supporting one another, physicians supporting patients, and patients supporting physicians through the treatment decisions and beyond?
- [Douglas] Well, the first thing upon diagnosis is make sure they're aware of resources like BCAN, local bladder cancer support groups. Encourage them to seek out these resources because the medical system itself can't really provide the kind of support that they need. Encourage them to bring their spouses and caregivers to their appointments, get another set of ears available. But make sure that you make it clear from the beginning that your only concern is their health and well-being. Make sure they know that your feelings won't be hurt if they wish to seek a second opinion and that you want to hear about any side effects they're experiencing from their treatment. You understand anxiety they're experiencing; it's only natural to be anxious, but you and your team are there for them. I think another really important point is this whole issue of shared decision-making. I think most patients want to be fully involved in all decisions, but there is a small minority who prefer to leave it in the doctor's hands and have faith that all will be well. These patients are too stressed with the challenges of shared decision-making. So, while it's a small minority, I think it's important to ask people how they wish to proceed in terms of the decisions around their care. Regarding some of these newly approved treatments for non-muscle-invasive bladder cancer, make sure people understand the advantages and the success rates, but it has to be in words that they can understand. And lastly, try to really understand patients' risk tolerance. As I mentioned, in my case, my risk tolerance was very low; my bladder meant very little to me compared with my fear of progression and certainly the fear of death from bladder cancer. But for other patients, their risk tolerance and priorities could be very different, and some are willing to take on substantially more risk to keep their bladders. And I know that the topic of bladder preservation versus radical cystectomy is coming up in another podcast, so maybe I'll leave it there. But I have quite a bit more comments to make on that next upcoming podcast.
- [Ashish] And we really look forward to hearing those comments, Doug, because that, as you know, is a really hot topic right now. Things that physicians thought were important to patients, such as bladder preservation, are maybe not as important from a patient perspective. And I think that's what you're alluding to. But in the interest of time, we will wrap this up. I really appreciate both you and Camille taking the time to join us today, share your insights into the diagnosis in part one. And of course, the treatment decisions and the pearls of wisdom that both of you imparted to both the healthcare professionals as well as the patient and the carers are really, really important. Because I think, like you mentioned, when patients are empowered, it also empowers us to provide you with the best possible chance of cure, right? And that's what we're all doing this for. So once again, thank you for taking the time, and thank you for everybody listening. Stay tuned for the next episode.
- [Douglas] Thank you, Dr Kamat.
- [Camille] Thank you.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

