Managing High-Risk NMIBC
Transcript: A patient on navigating NMIBC diagnosis
Douglas Cappiello, MD; Camille Cappiello; Ashish Kamat, MD, MBBS, FACS
Podcast recorded November 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- [Ashish] Hello everybody and welcome to "Expert Voices - Navigating non-muscle-invasive bladder cancer." I'm Ashish Kamat, neurologic oncologist at MD Anderson Cancer Centre in Houston, Texas. And today we're gonna be tackling something that's extremely important to us, hearing from patient, caregiver perspective, really the heart of what we do, and really wanna learn from Dr Douglas Cappiello, who is a physician and a bladder cancer survivor, and his wife, spouse, supporter, caregiver, Camille Cappiello as well. So Douglas and Camille, welcome.
- Thank you. - Thank you. Nice to be here.
- [Ashish] So if you could briefly share your bladder cancer journey, you know, from the first symptoms you noticed to when you received a diagnosis, what did this feel like? How did those early symptoms feel like? How did it evolve? Share with us your journey a little bit.
- [Douglas] Yes, thank you. So I wanna kind of set the stage for a minute, if that's okay. As everyone is fully aware, in February of 2020, the COVID pandemic was just beginning to sweep the globe. All activities stopped. Cancelled all our travel plans. Doctor's offices, clinics, surgery centres were closed, hospitals were filling with sick COVID patients, and thousands of people were dying every day. And it was during that frightening backdrop in April of 2020, it was a Sunday night at 10:00 PM that I experienced my first ever symptom of bladder cancer. I had sudden massive hematuria with large clots upon voiding before I went to bed that night. I knew I was in big trouble, but I did not plan to go to the emergency department at midnight on a Sunday considering the backdrop. So I went to bed. The next morning, I woke up and thought maybe that was a dream, but unfortunately it wasn't. I tried to void again and there were even more blood and clots and to the point that my urine stream stopped and I began to panic. But COVID turned out to be a mixed blessing. I called my PCP that morning, and he immediately arranged a CT urogram and the urology appointment for that same morning because everything was available. Everything was closed for routine care. By this point, I was completely unable to void. And as you know, there's a fluid load that we take during the CT urograms. So my bladder was noticeably distended. I was very uncomfortable. Fortunately, the CT showed no stones, no masses in the kidneys, no hydronephrosis, but there was a questionable small mass in the bladder. When I went to the urology department later that morning, my bladder was markedly distended. The nurse who puts in Foleys for a living could not pass the Foley. My general urologist came in, but he was able to force the Foley in with extreme pain on my part. And I passed 1100 CCs of bloody urine with clots. And now again, due to the high suspicion for a bladder tumour and with the surgery centre closed for routine cases, I was able to be taken directly to the operating room that afternoon. And two small papillary masses were removed, about 1.5 centimetres each near the trigone. The pathology report came back the next day showing stage T1, high-grade non-muscle-invasive bladder cancer. So I had a very unique experience. I went from my initial symptoms to definitive diagnosis in about 48 hours with little time to contemplate what was happening to me. So that's kind of my story of how I got diagnosed.
- [Ashish] Well, you know, being a physician yourself, you were able to help navigate your situation and self-direct in a way that unfortunately many patients in the country, especially during the COVID pandemic, were probably not able to, right? So based on your experience and the conversation you've had, I'm sure with others, through BCAN and and other avenues, what advice would you give to patients that are trying to navigate the healthcare system, and how would you describe your understanding of what they're going through prior to receiving a diagnosis?
- [Douglas] Well, as I mentioned, COVID was a mixed blessing for me. Everything's happened so fast, there was no time to worry. But most patients, really, as you stated, they have a very different story and there's often significant delays in diagnosis. What we have discovered is that oftentimes primary care physicians don't appreciate or recognise the warning signs for bladder cancer, and they treat it for as a UTI, other issue before even contemplating cancer. And this is especially true for women. And we hear of long delays to obtain a urology visit and long delays getting into the OR for TURBTs, long delays to get the pathology report back. So patients are often waiting two to three months or longer for this process to play out. And this is particularly for women and patients living in rural communities, not near an academic medical centre. So they deal with a lot of fear and anxiety for patients and their families not knowing what to expect. They have no information available to them, and they don't know where to turn for information. The only advice that we can give, I think, is to be a strong advocate for yourself. And both yourself, your spouse, your caregivers, your family, have to really constantly pound on the medical system and make sure that you're getting the care you need.
- [Ashish] Yeah, no, I couldn't agree more. And, you know, you bring up the delay from symptom presentation and, of course, referral and diagnosis. And at least in North America, it has been the case that this time has gotten shorter, but there's still parts of the world, including developed countries, for example, the UK or different types of healthcare system where that delay can be as long as one year, right? So we have to look at the global perspective too. And, yes, women for sure, you know, because bladder cancer is less common in women, and, of course, because women have other reasons to maybe have blood in the urine, it gets ignored sometimes, right? And let me focus a little bit on you now and have you put on your physician hat. So, you know, as a retired physician, what was your experience with bladder cancer prior to your own diagnosis? You know, did you have any experience, others that you'd spoken to in the medical community? You know, remove your head as a patient for a second and talk to us as a physician what your general experience was.
- [Douglas] Well, I'm embarrassed to say that, frankly, I knew next to nothing about bladder cancer prior to my diagnosis. I practised as an ophthalmologist for 30 years, and I honestly can't recall a single patient that I came across with the disease. None of our family or friends that I knew of had bladder cancer either. So it's interesting that after my diagnosis, I learned of several people who I know who've been fighting bladder cancer themselves or have a close family member with bladder cancer. In fact, I'm sorry to say that two of my former medical colleagues succumbed to the disease, but I didn't know about any of this prior to my own diagnosis. In my case, and taking off my medical hat for a moment, if you don't mind, the first thing our general urologist told us upon seeing the tumours in my bladder was to immediately go to the Bladder Cancer Advocacy Network's website. And I know that in other countries and in the UK and in Europe and other countries, there are organisations similar to the Bladder Cancer Advocacy Network or BCAN. And it's really important to learn as much as you can about the disease prior to having any kind of an in-depth discussion with your physician so that you're prepared. And BCAN opened up a whole new realm of information, and we wanted to learn everything we could. We read articles, we viewed expert webinars, some by yourself, Dr Kamat. We listened to podcasts. We ordered the Bladder Cancer handbook. There's also a website called Inspire, where it's kind of like a message board where survivors, you know, talk with each other and ask each other questions. And we even got a Survivor to Survivor volunteer who helped us navigate everything. So I will say that we would've been lost without BCAN, even though I was a physician and Camille was a nurse. And we'll be forever grateful to our general urologists for immediately recommending it to us. I also wanna say that we joined a bladder cancer support group, which was immensely helpful. And I think, you know, looking back, I will say that, unfortunately, the fact is that the healthcare system is often too overburdened to provide the time necessary for in-depth discussion with most patients. And fellow survivors and organisations like BCAN are needed to fill this gap. And we really wanted to learn as much as we could about bladder cancer to reduce our own fear and help us prepare for our meetings with our urologists.
- [Ashish] You know, I'm really glad to hear that because as you probably know, I have been involved with BCAN since its inception, and really I'm a strong supporter of advocacy groups and patients being not only their own champions, but recruiting friends and family and carers to help them. In fact, you mentioned some of the other global organisations, and the World Bladder Cancer Patient Coalition is a global organisation. And through that, actually during the pandemic, we launched a global effort to reach patients and their carers in 45 different countries to actually find out what is it that they want, what is it that they need, what is it that's missing. And BCAN's now replicating this in North America. So getting this information from a global perspective, from the US perspective will actually really help us, I mean, us as in physicians, but also advocacy groups, tailor our message to what patients and their carers are actually reflecting is missing, right? Because you said you had multiple resources available, but I'm sure there's more that you could have benefited from knowing. And with that, let me ask Camille a little bit. So, you know, Camille, you've obviously been a strong supporter of your husband, but you've also been a strong supporter of Survivor 2 Survivor volunteers within BCAN for several years. Now, based on your experience as a carer, share with us a little bit about what your thoughts are on these advocacy groups, how they support patients, how they support you, the family of patients. Share with us your insights a little bit.
- [Camille] Thank you, Dr Kamat. I want to share that, again, the support of BCAN, of course, was incredible, because, once again, I was coming out as a retired dermatology nurse and really didn't have much experience in the bladder cancer realm, probably since, you know, nursing school, which would be too many years ago. So, you know, reeducating ourselves. And it was, you know, a gift, in that, we could understand the medical language and that we were able to navigate that part of it, and at the same time, huge learning curve. So having the support of BCAN and these other resources, as Doug already mentioned, was incredible. And the BCAN caregiver tips for caregivers is also well done and really allows the caregiver to organise their thoughts and hopefully alleviate some of their own concerns as they walk alongside their loved one.
- [Ashish] Thanks for sharing that. Doug, let me now switch to an aspect of just cancer diagnosis, but bladder cancer specifically. You know, it clearly has an impact on patients' private lives, right? Because you alluded to the fact that you didn't really know much about bladder cancer prior to your diagnosis, and some of it is also because patients with bladder cancer, even celebrities, are reluctant to come forward and discuss this openly because of the implications on, you know, causation, et cetera, et cetera. So if I were to ask you, you know, how did your diagnosis impact your daily life, the relationships, how did your family react, conversations with friends and others?
- [Douglas] Well, first let me just say that I'm aware of that worldwide survey that you were involved in, and I read the results of that and I just wanna thank you and everyone involved for really starting to focus on the patient voice. I think it's really critical, and it really helps physicians who are caring for patients understand what they need, not just physically and medically, but also emotionally. So to get back to your question, you know, my first thought about hearing my diagnosis was I'm going to die. I experienced overwhelming anxiety, sleeplessness. I was unable to concentrate. Due to COVID, in our case, we were already isolated in our home. We couldn't visit friends. We were worried about even visiting family. And that made it much worse mentally. I always thank God for my wife Camille. She supported and encouraged me. She kept my spirits up and accompanied me at every doctor's visit and procedure, even though they wouldn't let her into the building. Our two grown daughters were also there for me always. Friends brought over delicious, healthy meals. They helped with shopping, but they couldn't come by to visit. It was a tough time for everyone, but it was especially difficult for someone dealing with a new diagnosis of cancer. And we have spoken, of course, to many other patients not involved during the COVID outbreak. And what they've done is they've often auto-isolated themselves. And that gets to the point you're asking, Dr Kamat. They're so anxious over their diagnosis, they don't want anyone to know. They don't wanna worry their kids or their family members. They don't wanna worry their friends. They don't share with family. And we often try, when we try to counsel them, we try to get them to open up and accept the love, support, and a friendship that people wanna give. But it's very difficult for some people to do. So it's really a tough time in everyone's life. But some people, when they auto-isolate, they make it even more difficult on themselves.
- [Ashish] Yeah, and, you know, in your own experience, you know, as you're alluding to and experiences of others you've supported, there are specific challenges related to identity, background, the care setting. You talked about rural versus urban. Did you or others you've spoken with face any specific barriers related to access or communication or stigma during the diagnosis? And if so, do you think healthcare professionals or others should make more an effort to understand this or do things differently?
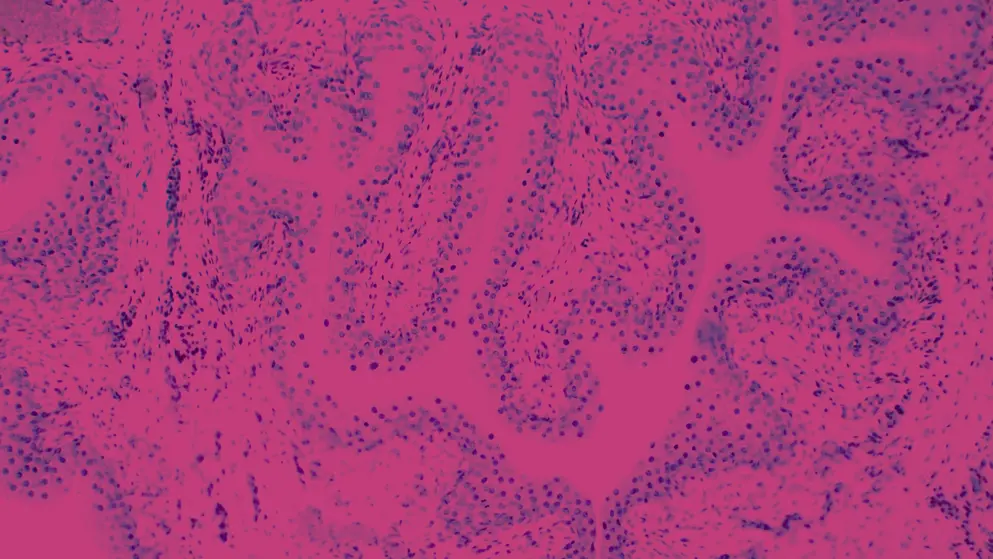
- [Douglas] Well, I think, and I've kind of alluded to this already, but I do wanna point out and emphasise that women we spoke with have had significant delays in diagnosis. And this is generally not related to the urology specialty, but more so to the primary care and OB specialists not recognising the warning signs of bladder cancer and endlessly treating for UTIs, et cetera. So I think education of primary care colleagues in your communities, raising awareness about bladder cancer would be very important in rectifying the issue. The second group that we've come across are those who live in rural settings, at least in the United States, far from an NCI or academic institution. Patients often stay with and receive their care locally, and they're treated by well-meaning physicians, but they have much less experience or inadequate facilities to treat bladder cancer patients. Or they must travel long distances, often three to four hours to an academic centre. So here, we believe really expanding the use of telemedicine and easing roadblocks to virtual second opinions at NCI centres, not just for uro-oncology, but I also wanna point out for GU pathology could be a key to assuring proper treatment is being delivered. I bring up the pathology because we've spoken with many people, and myself included, where the initial pathology report was actually inaccurate, where there was more extensive disease than was reported. And we ended up, our pathology report ended up getting sent out for a second opinion to Hopkins. And initially I was diagnosed with T1, high-grade non-muscle-invasive, but after Hopkins took a look at it, they also identified CIS, which is kind of a game changer. So I think that's really important as well. So we gotta make it easier for people living in rural environments to get the kind of care that they would receive in an academic centre through telemedicine. Now, in terms of care- - Yeah.
- [Douglas] I'm sorry. Go ahead.
- [Ashish] No, I was just gonna say, I totally agree with the aspect of pathology being crucial. And unfortunately today with AI, digital pathology, you know, faster computing, hopefully we'll be able to address that issue by having folks even in rural areas or pathologists at least be able to digitise the slides and send those to a referral centre for instant viewing, right, rather than actually physically sending the slide. So that's just, I wanted to agree with you there. Sorry. Didn't mean to interrupt, so continue.
- [Douglas] Oh, no, and I didn't know that that was being done. So I mean, I've been retired too long to know what's happening in the medical field any longer, but I'm really excited to hear that. I was just gonna make one last point. In terms of the care received by different ethnic groups, and I don't know if you were driving at some of that, we know this problem exists. We've seen evidence to that effect at some of the BCAN think tanks and other meetings that we've been to, but we have not personally had any experience with that sort of challenge. But I do think that that is a third area where we have to close those gaps.
- [Ashish] No, we absolutely do, because when we and others have studied this, there is a clear delay in certain ethnic groups as far as the diagnosis of bladder cancer is concerned. And it's not necessarily a delay on the part of the physician. It's sometimes driven by socioeconomic factors where, you know, someone can't ask their grandson or granddaughter to take time off and drive them to the physician or just can't afford to actually take the time off. So those factors come in as well. You know, I really appreciate you sharing your diagnostic journey. We're gonna have a next podcast that we'll deal with treatment and so on. But in closing, I just wanna give you and Camille as well maybe 30 seconds a minute each to tell us your closing thoughts on reflecting your own diagnostic journey.
- [Douglas] Well, I just wanna emphasise to physicians treating patients that the moment of diagnosis is terrifying. Patients usually panic due to lack of understanding. That's why it's important to refer patients to BCAN and similar organisations or to join a support group. And each subsequent scan, TURBT, cystoscopy, whatever it is, scanxiety, as they call it, it's real. But a couple of more subtle things that I think it's important for physicians to understand. Patients often don't wanna disappoint their doctor, so they minimise their anxiety, they pull it all together for their appointments and put on a positive facade. They're also fearful of upsetting their doctors by requesting a second opinion. So it's critical that physicians proactively tell patients that this is a lot to deal with and that you're there to do what's best for them, encourage them to seek a second opinion if they desire. Tell them you wanna hear about what concerns them, what side effects they're experiencing, which will help build trust and confidence. And the other thing is remind the non-muscle-invasive patients that their prognosis is actually quite good and that there's never been a better time than today when you can optimistically say that there are many effective new treatments available, something that really wasn't available to us just a few years ago. Lastly, patients are often too distressed to understand what is said at a doctor's appointment. So it's really important to have them make sure they bring their spouse or other caregiver with them to support them and help take notes during visits. Those are just a few of the recommendations we have at this very early stage of diagnosis. - [Ashish] Thank you so much, Doug and Camille, for sharing your insights with us. This was a great discussion, and I think a lot of pearls, not just for patients and the carers, but also healthcare professionals, all of us taking care of patients like you. So thank you very much for joining us, and stay tuned for the next episode where we'll talk about your treatment journey.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

