ACR 2025: Biomarker advances in HLH/MAS
Biomarker-driven breakthroughs in MAS and HLH
By Litha Mfiki
Three studies presented at the American College of Rheumatology (ACR) Convergence 2025 highlighted emerging diagnostic and therapeutic strategies for macrophage activation syndrome (MAS) and hemophagocytic lymphohistiocytosis (HLH), with a focus on biomarker-driven approaches and early intervention.
Edward Behrens (Children’s Hospital of Philadelphia, Pennsylvania, USA) and Alexi Grom (Cincinnati Children's Hospital Medical Center, Ohio, USA) shared pooled data from two prospective trials evaluating emapalumab in children and adults with MAS secondary to Still’s disease.
Among 39 patients, ranging in age from 9 months to 64 years, 53.8% achieved a complete response (CR), and 76.3% achieved a complete or partial response (overall response [OR]) by week 8. Median time to first OR was 16 days.
Looking at the subgroups individually, CR was similar for classical MAS (n=5; CR, 60.0%), MAS at Still’s disease onset (n=18; CR, 61.1%), and chronic relapsing MAS (n=13; CR, 54.4%). OR was high across all MAS subgroups (classical MAS, 100%; MAS at Still’s disease onset, 88.9%; chronic relapsing MAS, 72.7%).
Baseline levels of CXCL9, ferritin, and soluble CD25 (sCD25) were significantly higher in responders than nonresponders. During treatment, CXCL9 and ferritin levels dropped by 98% and 99%, respectively, in responders, compared with 86% and 89% in nonresponders. sCD25 levels fell by 80% in responders but rose by 21% in nonresponders.
Glucocorticoid tapering was successful in all groups, with mean daily doses reduced to 0.8 mg/kg per day by week 8 regardless of MAS subtype.
“These markers reflect [interferon gamma] activity and lymphocyte activation,” Behrens explained. “Patients with elevated baseline levels responded better to emapalumab, consistent with its mechanism of action.”
Complementing these findings, Erdem Bektas (Istanbul University, Turkey) presented a retrospective study evaluating serum procalcitonin (PCT) as a potential biomarker for MAS in Still’s disease. Among 110 patients meeting Yamaguchi criteria, the 35 with PCT ≥0.5 ng/mL had significantly higher rates of pleuritis and MAS, elevated inflammatory markers, and increased need for biologic disease-modifying antirheumatic drugs (DMARDs), most commonly anakinra.
Logistic regression – including 59 healthy controls and 56 people with a bloodstream infection – revealed a 6.4-fold increased risk of MAS in the high-PCT group and a 4.3-fold increased risk after multivariate adjustment.
“High PCT in Still’s disease may reflect a strong inflammatory response and serve as an independent predictor of MAS,” Bektas concluded.
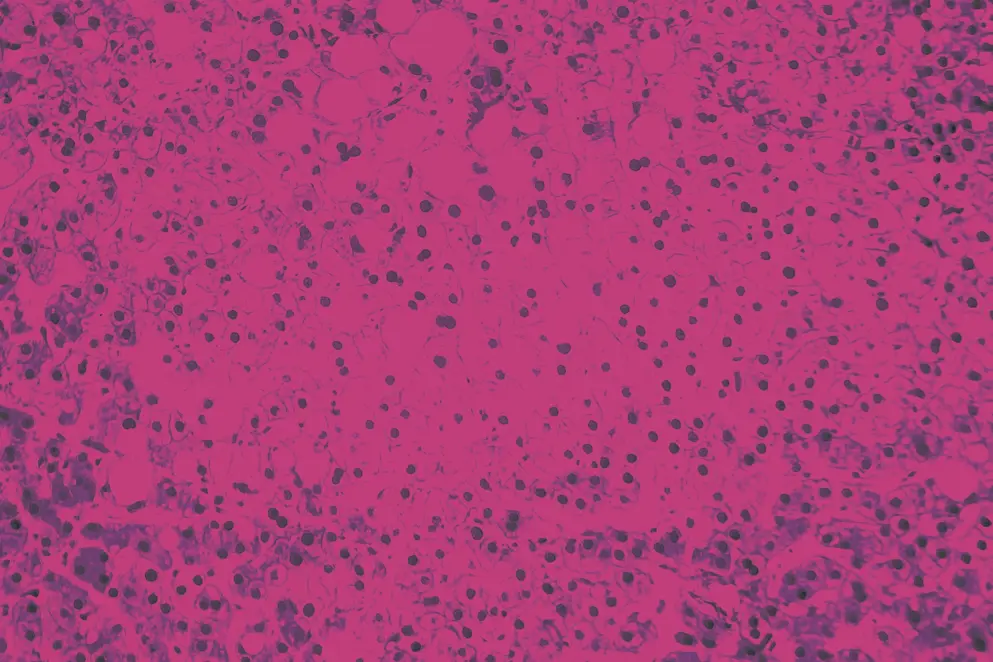
In a separate study, Chen Chao (Albert Einstein College of Medicine / Montefiore Medical Center, New York, USA) and colleagues evaluated serial ferritin as a surrogate biomarker for HLH diagnosis in critically ill adults. They noted that HLH diagnosis often relies on HLH-2004 criteria, which include bone marrow biopsy and soluble interleukin-2 receptor (sIL-2R) testing, both with delayed turnaround times.
Most patients were critically ill: 60% required intensive care, 25% needed renal replacement therapy, and 42% required mechanical ventilation. sIL-2R was highly specific for HLH but slow to return, limiting its utility for early treatment decisions.
Among 88 patients (definite HLH, 59; probable HLH, 16; non-HLH, 13), ferritin emerged as a promising early marker for HLH. With a cutoff of 2,684 ng/mL, it was 89% sensitive and 53.8% specific at diagnosis, while a cutoff of 5,000 ng/mL achieved 67.2% sensitivity and 91% specificity at 1 week. At 2 weeks, a cutoff of 2,182.5 ng/mL showed 85.5% sensitivity and 72.7% specificity.
Elevated sIL-2R levels were associated with increased in-hospital mortality (OR, 2.09; 95% CI, 1.32–3.30; P=0.002).
Together, these studies underscore the value of biomarker-guided strategies in diagnosing and managing MAS and HLH, offering new avenues for timely intervention and personalized care.
Developed independently by EPG Health, which received an educational grant from Sobi, awarded to EPG Health to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
