HRR Mutation Testing in mPC
Transcript: Interpreting HRR results with confidence
Bertrand Tombal, MD, PhD, and Alicia Morgans, MD, MPH
Interview recorded October 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- [Moderator] Hi, and welcome to another in our series on Expert Exchanges on HRR in metastatic prostate cancer. I'm so excited today to speak with Dr. Bertrand Tombal, who is going to be speaking with us about understanding the report, interpreting HRR results with confidence. Thank you so much for being here with me today, Bertrand.
- [Bertrand] Oh, my pleasure. It's always fun and interesting to helping you, so I'm here.
- [Moderator] Wonderful, thank you. So, you know, these reports can be complicated, but they're a critical part of what we do clinically and certainly a really important part of treatment decision making for patients with prostate cancer. Let's start from the basics. How do you approach interpreting these HRR genetic results and the reports for those results for patients with metastatic prostate cancer especially if you're seeing things that are complex or maybe unfamiliar variants on those reports?
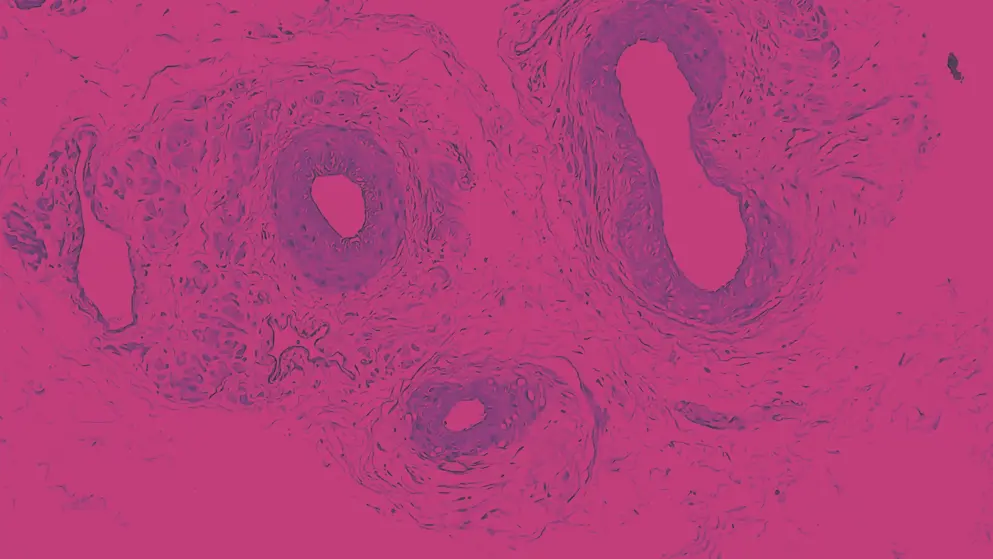
- [Bertrand] Okay, so I think that for the practising physician, I'm not speaking like oncogenetician and all the kind of family impact, but for like urologist, medical oncologist, if we focus, for instance, on homologous recombination repair, I'm gonna say HRR, like everybody say, I think what's very important is to first verify what is the context and the source of the result. Was it tumour tissue, ctDNA, germline testing? Because it will affect interpretation and therapeutic implication. Then there is a series of specific information which is needed, like what is the specific gene we are speaking about? What is the specific gene involved? Is there a variant classification? What is the zygosity, is it homozygous, is it heterozygous? And also it's important to know the allelic fraction and together that will help determine biological reference. I think that especially, you know, when we speak about HRR a very important fact is that we usually consider all this gene to be part of the same family with the same implication for the patient with the same consequences on health's disease, whatever. But one of the first important step is really to know whether is this pathogenic or likely pathogenic, okay. It's very important for genes such as BRCA1/BRCA2, but also it may be more important for genes like ATM, PALB2, CHEK2. Also, it's important to know whether it is biallelic or monoallelic. That's an important information for the PARP inhibitor sensitivity. I mean, if you start somebody on a PARP inhibitor and you have a beautiful response, you could claim, I don't care about that because the patient will be responding very well, you can emit some toxicity. But if you start somebody on a PARP inhibitor and the response is not what you were expected, it's important to go back to that information because then the biallelic versus monoallelic information is important. And also sometimes I really believe that when you fall into situation like this, yeah, you don't have the response to we're expecting, especially for gene like BRCA2, it's important to have a confirmatory test. Sometime it's important to have two different tests. So that's very, very important.
- [Moderator] I think those are all such, those are really critical pieces of the way that we do this. Understanding the source, making sure you understand if it's pathogenic as an alteration or maybe just a variant of uncertain significance. And then understanding biallelic/monoallelic as we interpret the patient's ultimate response. You know, from your perspective, what are the most common challenges that we face when interpreting these results? Because it sounds simple when you describe those steps that we just talked through, but what challenges do you face? - The question we have the most, I must say, is for non-BRCA1/2 HRR mutation, okay. That's really where it's becoming critical. And not only for treating patient, but also for impact on long-term. And I would say that the typical discussion we have is, you know, the variants of uncertain significance in gene, like you know, ATM, it's a very big gene. So many of these variants are insignificant in CHEK2. And that's where, you know, I'm very privileged to be working with oncogeneticist and they would usually access large database to match the mutation we found into this large database. So that's an advice. I mean, as a clinician, try to learn the basic, I mean like I had to do like three, four years to go back to school because, you know, that was kind of long time ago. And if you are uncertain, there is a lot of publication, you know, publish paper on what is the functional, what is the function, what the evidence around the functionality of that mutation, that is very important. BRCA1/BRCA2, I know many people they want to go into detail, but honestly, clinically speaking, patient responding super well it's much frequent that patient responding super bad. But, you know, there was a lot of discussion around gene, like ATM, whether we should check them and no, and I think that the yes/no answer was absolutely contaminated by all amount, a large amount of variants of uncertain significance. And what we realise is that accessing base, like, you know, we sometimes use the cosmic database. I mean, you can get information and that can reinsure you about treating or not a patient with an ATM mutation. So that's important because beyond the preclinical data, sometime we lack robust clinical data for many of these variants. You know, to be honest, I think last year, we saw two patients with CHEK2 mutation for, I don't know, 50 with BRCA2. So it is very rare even so you don't expect everybody just look at the report and say, oh, that's a good one. No, you have to dig in and you have to do some preliminary work. That's the most important thing. That's the most important thing is that the message we have when we listen to many of the presentation, it's like, it's a single channel, OPO. You have that mutation, you are HRR. If you've got PARP inhibitor, it's gonna be working. No, it's not like that, I would say except for BRCA even. But come on, we could admit that we could act like this for BRCA1 and BRCA2 but for the other one, we have to look at, we have to look at this and even I would say for, even for BRCA2, okay, everybody would say it's very likely to be pathogenic, but if it doesn't work, it could be like a monoallelic or a low allelic fraction in the plasma. So I would say that it's extremely important to begin when you initiate drug like PARP inhibitor, because if you have a beautiful response, you can live with that, actually you don't want to even know what's happened if the patient responds very well, but if the patient doesn't respond well, you should not keep a treatment going where from the better understanding of the genetic report, you increase the doubt on the likely pathogenic thing. So that's to me the most important. And I think that's to me, that will disappear in four, five years. With the combination of knowledge, data, AI, I dream of a system where we are not gonna have to do all that work ourself. Like you're gonna send the tube of load or the piece of tissue and they're gonna answer on your behalf. Is it likely to respond to olaparib or , and actually this is this work we are doing and this work, it's really about what mutation looking at DLL and not hesitating when you have any doubt to look at what the literature is saying about this mutation, this rare mutation.
- [Moderator] Yeah, so you raised so many good points. I wanna just dig into a couple of those. So if these patients fell into a grey zone, that can be for many reasons, it may be a variant of uncertain significance, the VUSs, it may be that there was a low allelic fraction. It may be that there was something off about the sample. How do you work through these answers that may be kind of falling into a grey zone? Do you lean on your genetic counsellors? Do you lean on your multidisciplinary team? Do you go to the databases that you mentioned, like ClinVar or others? What do you do and what advice would you have for others who are trying to work through this?
- [Bertrand] I mean, that you can see to me, you can see it both way. The first way would be to say you speak to the patient, you try the treatment, but you inform before starting the treatment, that is a certain level of chance that it will not respond to the treatment. And that's where you have to be extremely careful and extremely demanding on the initial response. To me, the problem will be more when we are gonna use these drug in combination. Because if you use for instance, the combination of an RP and a PARPi, you cannot rely on that initial response because the initial response is driven mostly by the PARPi. I mean, if we are speaking about patient with metastatic CRPC progressing on a line of RP, I would say that the need to dig in detail for element of functionality can be replaced by a therapeutic trial. Okay, because you see that if the PSA doesn't decrease, if your patient doesn't improve, then you make, then I think it's important you go back to learn and to enrich these database and enrich that. Where we are getting more and more concern is when we treat in combination, because that's where I believe the result as they've been given like TELEPRO or PROpel, they haven't done, we haven't seen that in depth correlation with, you know, alleles single CT and all of this, because that's where, and I think usually we approach that in the multidisciplinary panel and we feed from the oncogenetician and we rely on their advice and then that's where we have to make a decision. Because unfortunately, as for today, as I said a little bit before, the physiology may not inform you with 100 person safety. But clearly if, I mean, if you have somebody with ATM and lower allelic count you're not gonna give and that is not a RP, if you have an ATM mutation and looking back at the database, you see that exact mutation was associated with three response on PARP inhibitor, you're gonna give it a try. So that's where all that preparatory work is important. And I think it's gonna, as you know, we're expecting very nice results soon in the metastatic hormone-sensitive prostate cancer. Keep in mind the benefit will be high, but the danger to treat people with no chance of response with BI as well. So we gonna have to do, and if we only see, if we only say, oh no, we only treat biallelic BRCA2 mutation, we will deprive the chance of being treated by a combination to a lot of patient for who by looking in detail at the genetic analysis, we could say, oh my God, that one is got good indication that it could respond. So that's why it's gonna be very interesting to work around. - [Moderator] Yes, it's definitely interesting. There's a lot changing, there's definitely updates that are coming each day. I wonder, have you ever gotten a notice from a testing company that says, oh, we had this previous VUS, but now we think that it's going to be, you know, this new outcome, whether it's pathogenic or we're categorising it as benign. Has this ever happened to you in your practise and if it has?
- [Bertrand] No, from a company no, but from our on oncogeneticists, yes. - Ah, okay. - And actually what is good is that they keep that in the database, and I must say in the last six months, I received three emails from them saying, hey, by the way, we look at that patient, he had that very unknown mutation. And we have no new data making us believe that actually it could be a significant buy-in. And that's important because then we know it, it's gonna be annotated in the dossier. So that's why I think that you need to keep, and that's not easy. No, I mean, I'm very privileged, not gonna do advertisement, but we are working on epic, so we can keep all these thing in the patient EMR, and that's very important to have at the level of institution, some kind of, what I would say, oncogenetic covigilance, you know, people looking at data, updating the database. And I think it's gonna come more and more because actually that information could come only from patient who tested PARP inhibitor in variant of unclear significance and reported very nice response. So that's why we are really at the dawn of all that project. And that's why it is very important to have access to that, because it's surprising or fast sometimes these database are updated, but to me, the experience of situation like this came clearly from some ATM missense variants where if you look, I mean two years ago people would've said, no, it doesn't work. We would stop the treatment and no, with new information, sometime for the exact same patient, we would anyway stop the PARP inhibitor. So that's this kind of multidisciplinary approve, this multidisciplinary approach is essential. Nobody, I mean, unless you have always a lot of brilliant people, but I don't believe that as a practising doctor, we have the time and the result to keep updated. So it is very important somebody do the job in the hospital.
- [Moderator] That's great advice, and I think the multidisciplinary theme is one that we have heard many times as we've talked to folks about this. It can't all fall on one clinician because certainly that's going to be insufficient to keep up with the changes that happen. I guess as more and more teams are coming online, implementing these testing strategies, trying to interpret these reports, what advice would you give to clinicians who are new to interpreting these HRR reports for patients with metastatic prostate cancer, whether they're urologists or others? What would that advice be?
- [Bertrand] I think that I would advise what I did, I did spend, like, I remember it was one afternoon drawing day off a very good course on the internet when you can really get the basis, you know, a few weeks ago I was attending a meeting and I was asking, it was a urology, medical oncology meeting. People were speaking about TELEPRO. And clearly I realised that there was a low understanding on what we were speaking about. And then I asked, but honestly, who knows the difference between things like germline and somatic heterozygous, you would be surprised that there's still a low level of understanding. And that level, realising that and realising the importance of that is critical because then if you realise you don't know, you have two options, either you can learn because it's easy we are doctors or you can decide to associate with oncogeneticists. What I fear a little bit is the really shortcut of going from a commercial company providing NGS and other technology producing a paper report and doctor reading it. I think that's, I don't know, maybe with AI it's gonna be much, much better than any multidisciplinary board, but that's a shortcut we see more and more. And that's dangerous because then you lack that ability of learning what is what and that's very important. And another aspect is also, and I was very surprised of that is to really train doctor on pre-analytical parameters. Okay, that they don't realise it's not a chest X-ray. I mean, I think that people miss chest X-ray in maybe one person of the case. Here it is not rare, I won't say frequent, but it's not rare that the material is not appropriate, that the amount of ctDNA is not there. And that the quality of the detection of alleles and all of that is not optimal. So I think this is something which is not yet fully integrated. For instance, now in MRI of the prostate, they have designed that PI-QUAL indicator will give immediately to the clinician, oh, I provide you with a report, but that report is everything but sure because the quality is low. That's also something you, working with biomarker for 20 years, people always underestimate the importance of the pre-analytical parameter. If you provide tissue, it's got to be good tissue, it provide ctDNA, it's a bit done properly. So that's very important because in the end, if you add the poor quality, a poor misunderstanding, then you accumulate risk of errors. So that's very, very important also. That always that to me, it's always every time you look at the result, I would say, you know what, I tell urologists, it's like PSA. When your PSA is elevated, the first thing you ask is not you have prostate cancer is, did you have any urinary infection in the last two weeks? So that's what I call the context of DSA. So the quality and the context we have at least to teach that because it's very, very important and sometimes in case you have doubt, uncertainty, you should not hesitate to retest on a different platform.
- [Moderator] So many good pieces of advice there. First, ensuring that we have that opportunity to engage in education, even brief education around the difference between germline, somatic, whether someone has a homozygous or heterozygous deletion of something and understanding those parameters that are necessary to ensure a good and quality test is able to be performed. Looking at whether there was sufficient tissue, whether it's going to be a quality ctDNA analysis is really, really critical too as we understand. Surrounding ourselves with a multidisciplinary team that can help us with interpreting these complex reports when we ourselves are having challenges or understanding who do I reach out to at a company, at my local institution to help try to clarify some of the areas of grey is critically important as well. And recognising that an ongoing education as this field continues to evolve will also be important. Whether we learn ourselves, whether we decide to outsource and then rely on our colleagues whether we work in a multidisciplinary team to make sure that these answers are really arrived upon. It's critical for us to do one of those things or find our own strategies to make sure that we have quality testing, quality reports and quality application of the findings to our patients and recognise that we may need to update those over time as new information comes in. Bertrand, you have given us so much to think about, so many things and ways that we can continue to do better. I really appreciate your time today.
- [Bertrand] Thank you, my pleasure.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.
Updates in your area
of interest
of interest
Articles your peers
are looking at
are looking at
Bookmarks
saved
saved
Days to your
next event
next event

