HRR Mutation Testing in mPC
Transcript: Best practices in collection and preservation
Anders Bjartell, MD, PhD, FEBU
Interview recorded February 2026. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
Well, there are several key factors from collecting the samples and the successful outcome. The time from blood drawn to preparation of plasma samples should be as short as possible, not more than two hours would be fine, and for tissue samples fixation or the prostate biopsies, for instance, are usually good, because just when you collect the biopsies, they're put in formalin, so that's usually not a problem, but if you use sample from prostatectomy, the quality of the fixation may vary. But using paraffin material, not more than 10 years since collection, and sometimes we try to make it not more than five years for successful outcome, that's even better. There are many lessons learned from real-world situations. One thing is that what kind of material to use if you will, and as prostate metastasis from prostate cancer, where, especially bone metastases are very difficult in preparation, and you need to decalcify the tissue, so in case we would like to collect metastatic tissue, should we aware of how much tissue we can get, and also that bone metastasis is maybe the only thing we can get, but it may be difficult to prepare and to manage the samples. If we look at liquid biopsies, you can collect plasma samples, but you can also use the streck tubes, which then the, you don't need to process the samples like within two hours, you have more time to, you can send away the samples for preparation, which makes it easier, but it's not always possible to use the streck tubes, also quite expensive. And the final SB rates are usually not what we would like to recommend, because you don't get many cells' material as they're limited, and you don't need really that how much tumor cells and versus other cells that you will collect, and that may also be a concern. So I think that was a few aspects on how to collect, or think about when collecting samples, both for liquid biopsies, and to work with tissue. There are a number of critical pre-analytical factors that may influence the quality and the integrity of tissue and liquid samples, especially when used for the next generation sequencing, and HRR testing. So there are many things to consider, and how to mitigate the risk factors. Time to fixation of prostate biopsies are usually not a problem, because they're put in formalin immediately after the biopsy has been taken, and looking at the liquid biopsies to collect blood for a circulating tumor DNA analysis is how quickly the samples would be processed and prepared, and they're stored in the free surrounding analysis. Streck tube can be used, and then can be stored in room temperature up to a few days until preparation, and that would also make shipping possible. So there are a few things to think about, and when sending samples to distant laboratory, there are always details about the shipping instructions, that is extremely important to follow in detail. It's the timing of the shipping, but it's also temperature you think about, and how you send the samples.
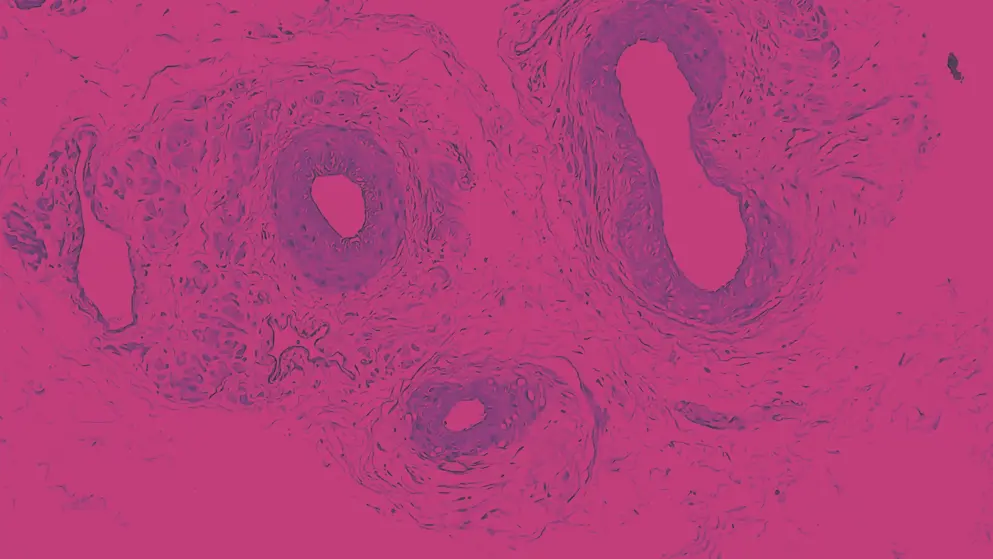
For ctDNA analysis, it's well-known that up to one-third of the samples may not be able to get the successful analysis from, and one can speculate if the proper handling of the pre-analytical handling of the samples, how much that play a role if you don't get a result from the ctDNA analysis. Proper documentation is very important for a better understanding of how we can improve preparation and handling of the tissues. I mean we always, should always document exactly when the sample is being collected, how long it will take until it's prepared, and how long it has been shipped, using careful, if we carefully document everything, they can better understand why, how we can improve, and get a higher success rate in our samples. Collection and preservation practices is different if you look at tissue samples, and if you look at liquid biopsies for ctDNA analysis. I mean, tissues can be stored for a very long time, maybe successful analysis can be formed even if the sample, the paraffin-embedded samples are up to 10 years, so that we don't have a problem with prosthetic, with prosthetic biopsies, or other kind of metastatic tissues. But it's important to understand what is the tumor content in a sample, that is critical for that you have material enough for the analysis. The challenge with liquid biopsies is to that the blood tube should always be filled up, so you have enough material, and also the time from collection to preparation. And besides the technical aspect, a successful analysis depends on if the samples are collected before initiation or treatment, that it can affect the analysis. Even a few days after initiation of hormone therapy, it may be much more difficult to analyze circulating tumor DNA. And the same is true for collecting blood from patients with a modest disease progression. So the turnaround times and storage conditions also differ between if you get tissue or you get blood for an analysis, the turnaround time for blood samples is much more critical than for tissue samples, as I just mentioned. And using prostate biopsies, formalin fixation begins already when the tissue specimens are obtained and the paraffin-embedment procedure, it's well-standardized, I believe most third involvement, we use the STEM procedure so that should not be the problem. The general recommendation is not to use biopsies older than 10 or maybe even five years.
However, there are not many studies on this topic to be honest. There are maybe examples illustrating when liquid biopsies have been beneficial, or when it's more challenging. I would like to emphasize to consider the optimal timing of liquid biopsy ctDNA analysis is before starting a new treatment, or at a very clear disease progression. There are many examples where you don't get an answer from the ctDNA analysis, and that is because you may not be able to detect enough circulating tumor in the circulation in certain situations. If the patient is still under treatment, that has good effect, then it's not possible. So timing on where in the disease journey you get to collect the blood is very important. There are many institutional and logistic factors that may influence the sample quality in a real-world setting. There is a variation between large centers and small centers with more or less experience of genetic testing, and feels like many centers are still in the beginning of establishing a good program to handle the bio samples. Regarding tissue samples, it's important to work with an experienced and interested pathologist who can look at the tissue quality and tumor content. So if you select the best samples you can find from a patient, that is really important for a successful outcome. Multidisciplinary coordination is also a very important, a successful outcome of the analysis depends on the collaboration between clinicians and pathologists, those who will analyze the samples, and everyone involved in the chain from collecting samples, until it's shipped and analyzed. Clinicians need to understand how to best get the sample, obtain the samples, nurses who will prepare the biopsy, prostate biopsies, and also technicians who will handle the samples. And of course the pathology is to select the best samples of high quality.
Quality assurance measures should be considered in every institution, it's of great importance to know exactly when the samples are collected, and how they were prepared, and this is true both for tissue and blood samples. Having access to that information will make a quality assurance program possible, and then we will better understand why analysis in some situations failed. I strongly believe that discussions at multidisciplinary team meetings, where you bring up, where you discuss the outcome of the analysis is important, where you have a oncologist, urologist, pathologist, clinical geneticist together, and that is part of the quality assurance program that you sit down together, and go through, especially cases, select cases, where you expected to find something, but the analysis didn't show anything, and also where you have maybe unexpected findings in the analysis, and then I think everyone can learn, and this is really teamwork that the multidisciplinary group will work together on to, on the improvement of everything from collecting the tissue, until understanding the analysis. Looking at the approaches that work well for training clinicians on sample collection and preservation, there's a lot to discuss. Optimization of sample collection and preparation is a multidisciplinary task, and these include selecting the right patient, collecting samples at the right moment, and following a standardized protocol for handling and preparation of the samples. And also documentation exactly when was the sample collected and when was it prepared. And besides obtaining samples from the right patient at the rate time, clinicians must get feedback on the test results, if they were successful or not successful, and then they will better understand what kind of improvement is needed, but this is, again, a multidisciplinary team question, and the team need to solve it together, and in a quality assurance program. The aim is of course to reach as high as possible success rate in liquid biopsies and the tissue biopsies.
The multidisciplinary team conferences for quality reassurance, where the clinical geneticist attend is something that I think we will see more of in the future, I don't think there are too, so many centers today, where clinical geneticists are present at the MDTs and give feedback to the clinician, I think this is something we need to develop much more in the future. I think it is most important to educate the clinicians who will collect the samples about the protocol for optimal collection of tissues, and for getting the plasma samples, especially the timing on when in the patient decision you can, you will, you should collect the samples for the best successful outcome. But also the pathologist who need to guarantee that the best samples have been selected for tissue analysis with the highest tumor content, and also that the material is as fresh as possible. If we don't have access to more recent tissue in paraffin-embedded tissue, then we should consider to take a biopsy. It can be a metastatic biopsy, but it can also be if there is a level of progression in the prostate. If we look ahead, I think we need to consider a number of things to improve sample quality and accessibility for advanced genetic testing. I strongly believe that we should develop collection of the plasma for ctDNA analysis, and because it's so easy to take a blood sample from a patient compared to finding tissue for testing, and especially if the patient has undergone many different treatments, where the paraffin-embedded material has a number of years since it was obtained, so I think we should, there's a lot of benefit in further developing ctDNA analysis that it can be performed at more and more centers, there is less need for shipping to certain centers, but we should also think about the quality of how of in analysis, the analysis of ctDNA, what gene panel, what methods is used, and so a quality insurance program, how you analyze ctDNA is also very important. And then regarding tissue, I already mentioned, that tissue for testing should not be too old, and with a high tumor content in the samples that we analyze. So I strongly believe that there's much we can do to further develop and implement genetic testing at more and more centers, and we should think about high quality that in every moment of the processing of tissues, collection of tissues and the analysis. And also to educate the clinicians to read the analysis, to understand the analysis, what mutations are important. So there is a need for education at every level in every specialty to make things better in genetic testing.
AI is everywhere today, and with machine learning, design of AI, and I mean you can probably use AI in a quality assurance program if you collect data, large amount of data, and you use an AI model to understand and interpret the data. And that may include the time from collecting the samples, and the processing, handing of the samples, and also the age of the tissue samples, and maybe shipping time, and of course the method of analysis, genetic analysis. There is the use, different panels are used today, and also different methods, and that can also be analyzed using AI, but I'm not sure AI at this moment will solve the problems, but it's interesting to think about, and there is a potential in using AI, absolutely. I strongly believe that the guidelines need to be improved on when to perform genetic testing, how to produce, how to perform genetic testing, and what to expect from genetic testing. So I think we're still, unfortunately, still in the beginning of the era of implementing genetic testing in many more patients than we do today.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

