HRR Mutation Testing in mPC
Transcript: Nick James on key PC insights from ESMO 2025
Nick James, BSc, MBBS, PhD, FRCP, FRCR
Interview recorded October 2025. All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- The presentation I'm most looking forward to is the presidential session, which includes the PSMAddition trial, because I mean, I have a, declare an interest here. The STAMPEDE2 trial is assessing PSMAddition in newly diagnosed patients as well, but with a different design to PSMAddition in that we're permitting the use of chemotherapy. Also, we've got, we're using a different, more intense schedule than the PSMAddition. Now the rumours are that it's a positive trial, but the detail has not yet been seen.
And why we know it's a positive trial is they've done a press release. So, that is potentially practice changing. Now, the thing about that is that you've got problems logistically around delivering PSMAddition. We know in the UK most centers are not able to do it because it's currently not funded treatment, and there's similar sort of issues globally. It's an expensive treatment. It requires, you know, referral to nuclear medicine in some way, shape or form. It requires a reconfiguring of their own services, potentially requires adding PET imaging and stuff on top.
So, there's a lot of complexity. It's not like prescribing pills. So, will be very interested to see what the magnitude of the effect is and how convincing it is. But it, almost certainly, is gonna be potentially practice changing. So, I think that is, for me, the most important thing. The other thing that I'm very interested in is there's a whole new, there's a whole lot of new, new sorts of treatments like bispecific T-cell engagers, just to pick one example, that are potentially very exciting. I mean, these are not, yeah, proceeding through phase three, but there's a whole lot of data around these sorts of things that are new. They're not just another way of targeting the AR pathway and there's other ways of targeting radioisotopes as well.
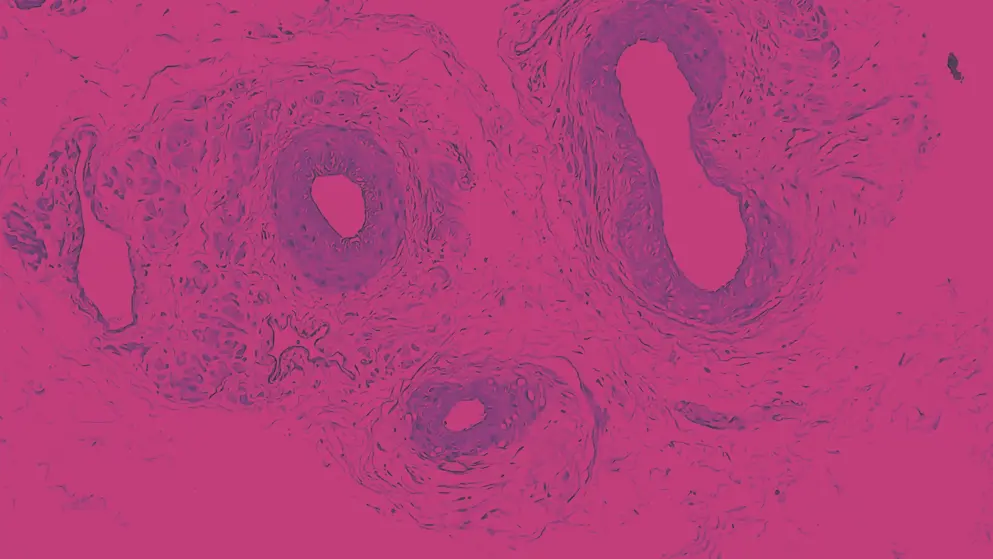
So, there's gonna be a whole lot of emerging data around things that I think are gonna be transformational in the future, but not quite yet. So, I think prostate cancer, yeah. The other thing that is, is still a sort of a hotly debated topic is around PARP inhibitors. So, my personal view is that the data looks the most compelling for patients with BRCA1 and BRCA2, and a very closely related package of very similar, you know, tumor mutations. But there is data, there are data rather that support unselected use. And for me, that data, those data are simply not that strong. So, but, we, for example, saw data yesterday, suggesting that it's active without needing to pre-select the BRCA mutations.
And it's kind of a slightly different class of PARP inhibitors than some of the existing ones. So, I think those sorts of things, yeah, remain an unresolved question as to whether we need to test or not to give these drugs. My personal opinion is we probably will still need to test. Yeah, probably things like saruparib are gonna be driven by, maybe, unknown DNA damage repair mutations in some way, shape or form. But, I think those sorts of things are very important. The other thing that's really very much of interest to me is the opposite end of the spectrum, how we diagnose people. So, PSA based screening is, remains controversial.
There remains potentially ways of improving it, adding in MRI scans, adding in polygenic risk scores, adding in things like trying to find BRCA2 in particular carriers. Because my colleague, Ros Eeles, is showing data here showing that we should be screening those, because they have a earlier presentation and a nastier disease biology. So, there's a whole lot of stuff around diagnosis linked to that. There's a whole, whole realm of stuff around inequalities of access.
So, patients from poorer backgrounds, from ethnic minority backgrounds, and particularly from black backgrounds, have poorer outcomes than white patients. Now, most of the screening trials were done in overwhelmingly white populations. So, we don't really know how PSA screening performs if you actively go into areas with high rates of deprivation, high rates of ethnic diversity, and I think that scenario requires a lot more work in the future, and there is work going there.
Developed by EPG Health. This content has been developed independently of the sponsor, Pfizer, which has had no editorial input into the content. EPG Health received funding from the sponsor to help provide healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content. This content is intended for healthcare professionals only.

