Transcript: Unmet needs for people living with NF1
Supported by SpringWorks Therapeutics
Said Farschtschi, MD, PhD
All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
- The biggest unmet needs in NF1 are numerous ones because NF1 is a multisystem disorder not being curable at this stage. And patients vary extremely in severity and also manifestations. And there are some patients needing more neuropsychological support and others needing advanced tumour therapies. But being on a more general level, I would say NF1 needs to be recognised as a multisystem disorder in multiple disciplines, and not only within our very small networks of NF-committed physicians. I think there's a huge difference. And transition of care is a major issue for many genetic diseases, for many rare diseases. But if you look at NF1 in specific, is that the face of the disease is changing completely in between childhood and adulthood.
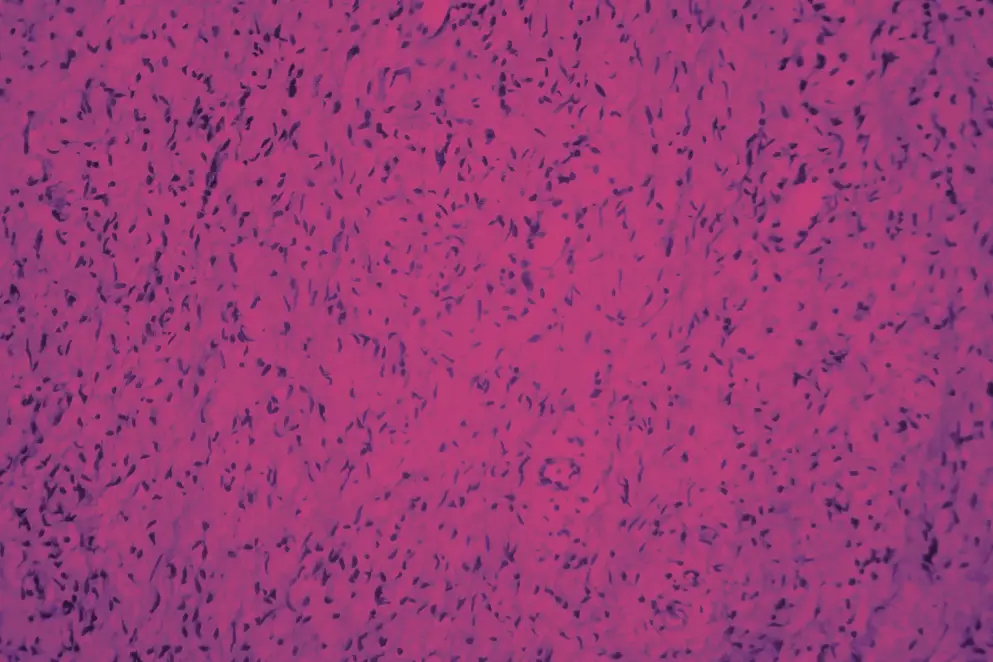
Children very rarely have malignant transformation of tumours, of plexiform neurofibromas, where it's very common and a major complication in adulthood. And I think it's very important to focus on the transition of care for those patients to provide a proper risk stratification. For the plexiform neurofibromas, it's first of all, very important to identify them. It can be very hard on a clinical level when they are very small or only superficial. Not good visibly. And also, we need to think about imaging protocols. When to image for the first time. How to do follow up imaging. And after identifying them, we need a multidisciplinary team to discuss the indication for surgical treatment for the new upcoming systemic therapies which are now on the market.
This is not something one discipline can provide on their own. So we need the discussion between the paediatricians, the surgeons, the neurologists, the oncologists, something which is not well established in every centre. I think providing good information to the patients is crucial. For patients, it might be overwhelming to see that there are now upcoming systemic therapy options. Not being able to decide right away. So it's very important to provide the implications of the therapy, the indications, and also to discuss surgical treatments in deep with the patients. Also, I think it's very important that patients are committed to a treatment plan developed together with their healthcare provider to not be surprised by, for instance, side effects or for unexpected outcomes of the therapy, or also of the effects of a neurofibroma. I think we have a very good structure within the over many years, well-established NF centres, but they are few and they are lacking resources regarding seeing new patients and also being able to provide what we as NF experts regard as essential. For instance, in Germany, we face problems providing whole body MRIs on a regular basis for those patients, which is a very important puzzle piece to discuss treatment indications. Also, it's sometimes hard to bring all the disciplines together to discuss certain cases, and I think we have to strengthen centres. But at the same hand, we also have to inform general practitioners and those who are not deeply involved into NF treatment. But as I regard NF, not really a rare disease. It is rare by numbers, one to 3,000.
But if you look at current studies, mosaicism is very common. And in the end, NF might be a quite common condition. Maybe not as a full blown phenotype, but as parts of the disease may play a role, for instance, in breast cancer. I see big gaps in the education of healthcare practitioners in general, as NF1 is not allocated to one a discipline only, so it is sitting in between chairs. And that leads some even bigger hospitals, NF is not recognised as a distinguished entity and treated in a continuous manner. Some healthcare providers only treat certain aspects of the disease. And in many cases, it's very important to be aware of the whole complex of the disorder to provide proper and long lasting treatment regimen. I think in the paediatric age group, paediatricians and paediatric oncologists are well aware, especially in the bigger centres. Of course, we need to raise awareness in the general practitioner context as NF1 is more common than thought. But in the transition age group and adult age group, I think it's very important to address the needs that needs to be covered by neurologists, by oncologists, and especially also surgeons because many of the surgical problems need a lot of expertise and experience and are not comparable to non-NF manifestations. Now, in the situation that we have for some years an approved drug now added with a second drug approved for children and adults.
This is looking at the many years we haven't had a systemic therapy for plexiform neurofibromatosis 1. Is a very new level. A new level which is also a challenge for the structure of the NF centres because we have to provide follow up regimens. We have to be able to provide proper counselling on the treatment options, something we haven't had on our agenda yet. So this is a challenge and a huge chance, of course, for a subgroup of patients. These treatments are not for every NF patient. This is also something we need to discuss and to build clinical experience on. And we also need to discuss how long and when to implement the therapies. And this is a challenge for upcoming trials, but also for the clinical experience and discussion within the multidisciplinary teams. I think treatment decisions are very differently built. It, on one hand, is dependent from the patient's perspective, whether or not he regards the plexiform neurofibroma as a current threat or not. And on the physician's perspective, how we are able to provide a long-term treatment regimen. We have to be aware that these are not malignant tumours at first sight. These are benign tumours. So it's not about survival, it's about a long lasting treatment regimen. And we are not helping the patient if we're only thinking within a certain timeframe. We need to think about therapy outcomes on the long run. And this makes it complicated. And I think we don't have all answers yet to answer this question. But I would say we need a good multidisciplinary discussion and also new trials to answer these questions. So the current existing treatment options are selumetinib for children with plexiform neurofibromas with inoperable symptomatic plexiform neurofibromas, which will now also be approved for adults.
There was a first study, the SPRINT study, for the paediatric age group, and a double-blinded study, the KOMET study, for the adult patient group. And there's a second drug called mirdametinib, which has just recently been approved in Europe for children and adults. And this is currently not available in all European countries, but will be soon. And those two compounds are both MEK inhibitors, so they inhibit a certain molecule within the pathway specifically being deficient in patients with NF1. And it is able to shrink the plexiform neurofibromas and to make tumor-associated symptoms lower, like pain or neurological dysfunction. And currently, there are no head-to-head trials, so we can only compare the two drugs from the trial outcome measures. But we have to keep in mind that those trials have have different rules of enrollment for patients, for instance. So again, even in that issue, we need to build up our clinical experience and to formulate treatment regimens also on the treatment duration in the near future.
Yeah, currently there are some guidelines on the European level and also on national levels. Just to name a few, I think very important are the guidelines from the European Reference Networks for the tumor-associated symptoms for NF1. And there are also national guidelines. In Germany, for instance, we have guidelines for the treatment of peripheral nerve chest tumours. And we also now wrote a checklist, which we as a few centres think is important in the context of new developing treatment options. But I think we need binding national guidelines that also enable us to demand changes in the healthcare system for our patients with NF1. My perception, it is very important to strengthen the centres because the expertise in treatment of NF-related symptoms mainly is focused in the NF centres. And we have to keep in mind, it's not only about providing medical treatments, but to discuss medical treatments together with surgical options and other therapeutic options. Also, having in mind that NF is not only consisting of plexiform neurofibromas, but can be a very complex setting of multiple manifestations, which can affect decision making regarding the treatment regimen.
And therefore, I would plead for strengthening the NF centres. I think it would be good to include the patients' voices also in formulating guidelines in the healthcare system because the view of the patients may differ gradually from our view as healthcare providers. And that's very important for the the near future. I think it would be a good step in the near future to develop strong national lay groups and patient associations that are able to get involved from political and medical decision making, and also participating in guideline development. If I could formulate a wish for the future, I would say we need to combine the experience, which is very extensive in certain fields, but combine the experience of the different disciplines. For instance, you need to combine the experience from the geneticists together with the clinical paediatricians and neurologists to be able to provide a more thorough understanding of treatment outcomes and treatment development in the near future. Yeah, I think the genetical landscape is a very fast-evolving discipline.
If you, you name it, molecular tumour boards play a very, a big role in decision making for oncological regimen, also the pathological analysis. And if you're able to combine those disciplines for formulating future therapeutic advances, would be a great advance.

