Transcript: Multi-parametric biomarkers in NF1
Supported by SpringWorks Therapeutics
Shivani Ahlawat, MD
All transcripts are created from interview footage and directly reflect the content of the interview at the time. The content is that of the speaker and is not adjusted by Medthority.
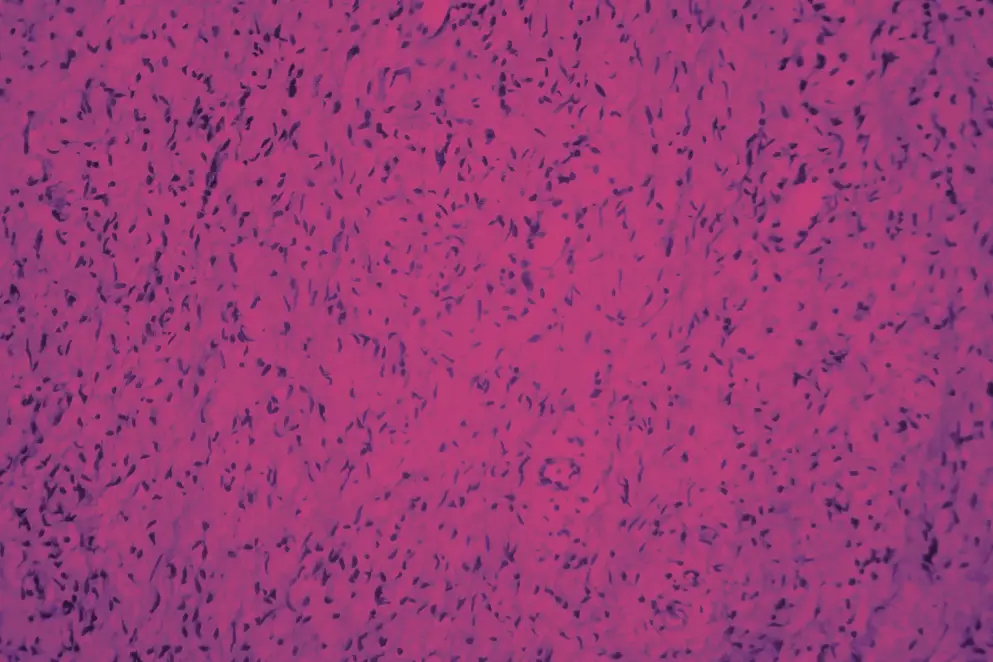
- The NF1 biomarker study is a prospective whole body MRI study on participants with NF1 that we would consider high risk for development of malignant peripheral nerve sheath tumors. MPNST is a dreaded complication of NF1. It's a fatal sarcoma that leads to overall decreased longevity in this population. And so we've tried to capture participants that would be high risk for development of this sarcoma, and we follow them out prospectively using whole body MRI, a non-invasive tool. And the risk factors that we've used as traits of high risk include genetic testing, known internal tumor burden, prior history of malignant peripheral nerve sheath tumor, and prior radiation. So factors like these. And we follow these patients out prospectively with serial whole-body MRI exam, and a clinical exam at our high-volume NF center over the course of five years. And the idea is to see whether they developed any suspicious lesions on imaging, and what those lesions on imaging that we think are suspicious actually turn out to be. And hopefully, we can establish what the imaging biomarker for an MPNST, or a pre-malignant lesion before an MPNST forms can be detecting using whole body MRI. The interesting part about this study is that it is prospective, it uses whole body MRI, which is a tool we use in this population, but we've combined it with diffusion weighted imaging, which is a special sequence that we perform at our institution. It's not proprietary per se, we use it in the brain frequently for the detection of strokes, but here we're using it as a marker for cellularity. So combining these two factors will allow us to characterize any lesion we detect more specifically.
The need to prioritize this high risk population for detection of NF1 related MPNST is, this is the population we think is more likely to develop it, particularly in earlier age. We know from prior retrospective studies. So unlike our study, which is prospective, we know from retrospective studies that patients that have high internal tumor burden are at greater risk for development of MPNST at an earlier age. So if we can capture a pre-malignant lesion in this population earlier, then perhaps we can prevent the future development of MPNST. What would be the potential impact of this study on treatment? The most important impact that might be is if we can capture a pre-malignant or suspicious lesion before it becomes a malignant peripheral nerve sheath tumor, is that it can be treated before it becomes that fatal sarcoma. And that might impact the lifespan of a patient because this is one of the most important causes for this population to have a shorter lifespan compared with their matched cohorts of people that are unaffected with NF1.
How can we use imaging biomarkers to stratify patients for surveillance or treatment? So what we've been working on so far is trying to identify pre-malignant lesions before they become an MPNST. Our current retrospective data shows that a distinct nodular lesion on MRI, so that is a peripheral nerve tumor that does not have an expected target pattern, is an imaging marker for an atypical neurofibroma, or an atypical neoplasm of unknown biologic potential. We don't know much more than that. We know maybe they tend to be more than three centimeters in size. They tend to grow rapidly. They may be FDG-avid on PET-CT, they may not. And we know a wide range of FDG values that overlap with both benign and malignant tumors. So we hope to find out more specific imaging characteristics of distinct nodular lesions that are indeed actually atypical or pre-malignant. And if we can find those lesions and characterize the distinct nodular lesion more specifically, then the suspicious lesion can be removed prior to MPNST development. So earlier treatment and MPNST development would be the optimal outcome of this biomarker study. How do imaging and genetic factors work together in this study? So we are trying to capture patients that we think are at greater risk for MPNST formation. And we know from prior data that's specific genetics and specific imaging features. So genotype as well as phenotype that can be seen by whole body MRI are associated with higher risk of MPNST development.
So specific genetic testing like micro-deletion, or specific internal tumor burden, which is a more of a gray area and we hope to learn more about it, would be important risk factors on how you screen a patient. So how early you perform a whole body MRI, how often you perform a whole body MRI, and whether you modify the protocol with the addition of more sequences like diffusion weighted imaging and perhaps make the scan longer for a patient. So personalize the screening strategy for that patient would be an ideal outcome also. How do genetic factors impact screening findings and screening strategies? We know based on retrospective data that certain genetic factors like micro-deletions tend to have patients with higher internal tumor burden. So those pieces of information could be combined. One is something we can gather from a blood test while the other we can see by imaging, and those would predispose the patient to a greater risk for MPNST and that particular patient would benefit from earlier and more frequent screening. But we base this information on previously gained retrospective data. So more prospective data is needed, particularly for what we consider high internal tumor burden. We don't know quite yet based on the existing data what a threshold for high versus low is. And so we base it as radiologists, sometimes just qualitatively looking at whole body MRI. Meanwhile, there are other centers across the world that measure that tumor burden using volumetric techniques and quantify it. But even if you quantify it, there is no threshold in existence yet that says, this particular person has X amount of tumor burden, and as such is considered a high internal tumor burden and would benefit from a different screening strategy. So that's all information we're trying to gain from this study in addition to other studies that are taking place across the US.
What are the most significant findings from the trial so far? The significant findings from the trial so far include that we've been able to enroll about 80 participants for this serial exam. And we noted that amongst the 80 people, especially at their baseline whole body MRI, number of patients actually had distinct nodular lesions. So about almost a fourth of that population had distinct nodular lesions, but only a small subset of those patients actually had a suspicious distinct nodular lesion that ultimately went on to either biopsy or surgery. So what we've learned is that distinct nodular lesion by itself is not the marker that we thought to be of MPNST. It needs, in addition, something else, whether it's a distinct nodular lesion plus growth, plus pain, plus prior radiation. So those are the factors we're still working on figuring out. So distinct nodular lesion itself is not the mere marker of MPNST, even though that's what we've thought on prior data. There's more to it and that's what we're learning. How can this prospective full body MRI study shape future management of patients? One of the main things we hope to point out is what additional features of distinct nodule lesion, or DNL as we call it sometimes, a distinct nodule lesion is truly pre-malignant. Whether there's a size criteria, or there's an imaging criteria, or there's a clinical criteria, or it's a size plus genetic criteria. So that's what we are still unraveling from this study. And if we can identify that, then we can more specifically identify the patients and the tumors within those patients that need to be intervened upon, and perhaps successfully prevent future development of MPNST or capture it earlier in its course.
We do think that the results of this prospective whole body MRI study on high risk people with NF1 would impact screening guidelines, and particularly identify which patients. So more information about the person level risk factors in addition to which tumors. So more imaging per tumor risk factors that would benefit from greater intervention, and it might influence how often we screen these patients and how we perform that screening. Whether it's whole body MRI alone plus whole body MRI in conjunction with a sequence that I told you about diffusion weighted imaging, and how that would inform our decision making in intervening on specific DNLs versus observing them on serial exams.
This study has been ongoing for about four and a half years, and we enrolled all of our baseline patients that have had baseline whole body MRI. We're still gaining more exams on an annual basis. So we need to complete the entire whole body MRI acquisition and interpretation for all five years, and we want to see who actually developed tumors. We also hope to apply more artificial intelligence and machine learning tools to see if we can predict on serial exams, who develops tumors, and which tumors end up being suspicious. Whether that addition, which will be again, a non-invasive addition, could impact our results. So we're still completing the study. What we've done is analyzed baseline characteristics, which I shared with you earlier. Which specialties could benefit from learning more about NF1 and its various disease manifestations? I think there are two main groups of medical specialists. One would be the general practitioner that could benefit from learning more about NF1, because we've learned a lot about how we screen this population.
We've learned a lot about other disease manifestations. For example, osteoporosis, breast cancer risk. So the general practitioner could learn more. And then a radiologist, a general radiologist, because we've learned so much about peripheral nerve tumors in the last 10 years alone. And application of diffusion weighted imaging and disease characterization, which patients have suspicious lesions, which lesions actually need biopsy, and when to refer this person to a comprehensive NF center.
