View transcript .
Chapters
.
View transcript .
Chapters 00:00 Overview of the ReNeu trial
Shivani Ahlawat delves into the NF1 biomarker study, explaining why identifying high-risk patients is critical and how multi-parametric biomarkers could transform surveillance strategies. The interview highlights how genetic risk factors guide patient selection and influence imaging-based screening protocols, alongside key insights from the trial to date. View transcript .
Chapters
Meet the experts
Said Farschtschi is Medical Director of the Phacomatoses Section at the University Medical Center Hamburg-Eppendorf, Germany. He oversees one of the largest neurofibromatosis centers worldwide, integrating multidisciplinary care for more than 1,700 patients annually. Farschtschi has conducted neurogenetic and neurophysiological research in phacomatoses since 2012.
Dusica Babovic-Vuksanovic is a professor of Medical Genetics and Pediatrics at Mayo Clinic, where she serves as Consultant in the Department of Medical Genetics and the Division of Pediatric Genetics. She leads collaborative research efforts in neurofibromatosis through Mayo’s Neuro-Oncology Program and the departments of Radiology and Neurologic Surgery. Her clinical and research focus includes overgrowth syndromes, genetic syndromes, and metabolic disorders.
Shivani Ahlawat is an Associate Professor of Radiology and Radiological Science at Johns Hopkins University, where she directs the Musculoskeletal Fellowship Program. Her expertise includes high-resolution magnetic resonance imaging (MRI) of peripheral nerves, peripheral nerve injury and tumor characterization, and advanced MRI techniques for bone and soft tissue tumors.
Catch up with the latest developments in management and research into NF1-PN, including breaking data from EANO 2025.
- The biggest unmet needs in NF1 are numerous ones because NF1 is a multisystem disorder not being curable at this stage. And patients vary extremely in severity and also manifestations. And there are some patients needing more neuropsychological support and others needing advanced tumour therapies. But being on a more general level, I would say NF1 needs to be recognised as a multisystem disorder in multiple disciplines, and not only within our very small networks of NF-committed physicians. I think there's a huge difference. And transition of care is a major issue for many genetic diseases, for many rare diseases. But if you look at NF1 in specific, is that the face of the disease is changing completely in between childhood and adulthood. Children very rarely have malignant transformation of tumours, of plexiform neurofibromas, where it's very common and a major complication in adulthood. And I think it's very important to focus on the transition of care for those patients to provide a proper risk stratification. For the plexiform neurofibromas, it's first of all, very important to identify them. It can be very hard on a clinical level when they are very small or only superficial. Not good visibly. And also, we need to think about imaging protocols. When to image for the first time. How to do follow up imaging. And after identifying them, we need a multidisciplinary team to discuss the indication for surgical treatment for the new upcoming systemic therapies which are now on the market. This is not something one discipline can provide on their own. So we need the discussion between the paediatricians, the surgeons, the neurologists, the oncologists, something which is not well established in every centre. I think providing good information to the patients is crucial. For patients, it might be overwhelming to see that there are now upcoming systemic therapy options. Not being able to decide right away. So it's very important to provide the implications of the therapy, the indications, and also to discuss surgical treatments in deep with the patients. Also, I think it's very important that patients are committed to a treatment plan developed together with their healthcare provider to not be surprised by, for instance, side effects or for unexpected outcomes of the therapy, or also of the effects of a neurofibroma. I think we have a very good structure within the over many years, well-established NF centres, but they are few and they are lacking resources regarding seeing new patients and also being able to provide what we as NF experts regard as essential. For instance, in Germany, we face problems providing whole body MRIs on a regular basis for those patients, which is a very important puzzle piece to discuss treatment indications. Also, it's sometimes hard to bring all the disciplines together to discuss certain cases, and I think we have to strengthen centres. But at the same hand, we also have to inform general practitioners and those who are not deeply involved into NF treatment. But as I regard NF, not really a rare disease. It is rare by numbers, one to 3,000. But if you look at current studies, mosaicism is very common. And in the end, NF might be a quite common condition. Maybe not as a full blown phenotype, but as parts of the disease may play a role, for instance, in breast cancer. I see big gaps in the education of healthcare practitioners in general, as NF1 is not allocated to one a discipline only, so it is sitting in between chairs. And that leads some even bigger hospitals, NF is not recognised as a distinguished entity and treated in a continuous manner. Some healthcare providers only treat certain aspects of the disease. And in many cases, it's very important to be aware of the whole complex of the disorder to provide proper and long lasting treatment regimen. I think in the paediatric age group, paediatricians and paediatric oncologists are well aware, especially in the bigger centres. Of course, we need to raise awareness in the general practitioner context as NF1 is more common than thought. But in the transition age group and adult age group, I think it's very important to address the needs that needs to be covered by neurologists, by oncologists, and especially also surgeons because many of the surgical problems need a lot of expertise and experience and are not comparable to non-NF manifestations. Now, in the situation that we have for some years an approved drug now added with a second drug approved for children and adults. This is looking at the many years we haven't had a systemic therapy for plexiform neurofibromatosis 1. Is a very new level. A new level which is also a challenge for the structure of the NF centres because we have to provide follow up regimens. We have to be able to provide proper counselling on the treatment options, something we haven't had on our agenda yet. So this is a challenge and a huge chance, of course, for a subgroup of patients. These treatments are not for every NF patient. This is also something we need to discuss and to build clinical experience on. And we also need to discuss how long and when to implement the therapies. And this is a challenge for upcoming trials, but also for the clinical experience and discussion within the multidisciplinary teams. I think treatment decisions are very differently built. It, on one hand, is dependent from the patient's perspective, whether or not he regards the plexiform neurofibroma as a current threat or not. And on the physician's perspective, how we are able to provide a long-term treatment regimen. We have to be aware that these are not malignant tumours at first sight. These are benign tumours. So it's not about survival, it's about a long lasting treatment regimen. And we are not helping the patient if we're only thinking within a certain timeframe. We need to think about therapy outcomes on the long run. And this makes it complicated. And I think we don't have all answers yet to answer this question. But I would say we need a good multidisciplinary discussion and also new trials to answer these questions. So the current existing treatment options are selumetinib for children with plexiform neurofibromas with inoperable symptomatic plexiform neurofibromas, which will now also be approved for adults. There was a first study, the SPRINT study, for the paediatric age group, and a double-blinded study, the KOMET study, for the adult patient group. And there's a second drug called mirdametinib, which has just recently been approved in Europe for children and adults. And this is currently not available in all European countries, but will be soon. And those two compounds are both MEK inhibitors, so they inhibit a certain molecule within the pathway specifically being deficient in patients with NF1. And it is able to shrink the plexiform neurofibromas and to make tumor-associated symptoms lower, like pain or neurological dysfunction. And currently, there are no head-to-head trials, so we can only compare the two drugs from the trial outcome measures. But we have to keep in mind that those trials have have different rules of enrollment for patients, for instance. So again, even in that issue, we need to build up our clinical experience and to formulate treatment regimens also on the treatment duration in the near future. Yeah, currently there are some guidelines on the European level and also on national levels. Just to name a few, I think very important are the guidelines from the European Reference Networks for the tumor-associated symptoms for NF1. And there are also national guidelines. In Germany, for instance, we have guidelines for the treatment of peripheral nerve chest tumours. And we also now wrote a checklist, which we as a few centres think is important in the context of new developing treatment options. But I think we need binding national guidelines that also enable us to demand changes in the healthcare system for our patients with NF1. My perception, it is very important to strengthen the centres because the expertise in treatment of NF-related symptoms mainly is focused in the NF centres. And we have to keep in mind, it's not only about providing medical treatments, but to discuss medical treatments together with surgical options and other therapeutic options. Also, having in mind that NF is not only consisting of plexiform neurofibromas, but can be a very complex setting of multiple manifestations, which can affect decision making regarding the treatment regimen. And therefore, I would plead for strengthening the NF centres. I think it would be good to include the patients' voices also in formulating guidelines in the healthcare system because the view of the patients may differ gradually from our view as healthcare providers. And that's very important for the the near future. I think it would be a good step in the near future to develop strong national lay groups and patient associations that are able to get involved from political and medical decision making, and also participating in guideline development. If I could formulate a wish for the future, I would say we need to combine the experience, which is very extensive in certain fields, but combine the experience of the different disciplines. For instance, you need to combine the experience from the geneticists together with the clinical paediatricians and neurologists to be able to provide a more thorough understanding of treatment outcomes and treatment development in the near future. Yeah, I think the genetical landscape is a very fast-evolving discipline. If you, you name it, molecular tumour boards play a very, a big role in decision making for oncological regimen, also the pathological analysis. And if you're able to combine those disciplines for formulating future therapeutic advances, would be a great advance. - The ReNeu study is a very important study, which is evaluating drug, mirdametinib, in the patients with plexiform neurofibromas, due to condition NF1 or neurofibromatosis type 1. So, this is very important study because it is bringing evidence that MEK inhibitor, mirdametinib, can be used in management of these complex tumours. So, obviously there is an unmet need for patients with neurofibromatosis because currently we only have a surgical treatment. We have option of observation only. And the only other systemic therapy, that is currently on the market is another MEK inhibitor, which is called selumetinib. And mirdametinib, is a second drug, which is bringing hope to these patients. What is known about this drug so far, it is standing out as a drug which does have effect on treatment of plexiform neurofibromas by decreasing their size. It can also improve quality of life, and help with the pain control in patients with NF1 plexiform neurofibroma. Side effects of these drugs are also relatively tolerable, which is standing out compared to some other oncological drugs. Mirdametinib showed efficacy in about half of adult and paediatric patients with a tumour shrinkage 20% or more. 20% is considered partial tumour response. And about roughly 50% of individuals treated with drug for at least 24 months did experience improvement, meaning that they had experienced shrinkage of the tumour. So, the deep response means that the patient had at least 50% in a tumour reduction, and a majority of treated patients who experienced tumour regression in a mirdametinib trial actually had a deep response, which is very remarkable. They did not know which patients are going to respond better based on a tumour size, or based on a tumour allocation, or their age or gender. So, there is really no way that we can know which patient is going to respond positively or a patient who will not respond. Well, what is really exciting is that in a long term follow up, we did observe additional responders. So, patients who were treated after 24 cycles of therapy, in a long-term follow-up, a few of them experienced a shrinkage of the tumour, and they continued to experience improvement in pain control and quality of life. So, patients treated with mirdametinib did experience improvement in the pain, in overall quality of life, and decreased in the pain mostly. So, that was a really remarkable response. We did not observe any additional, concerning side effects during the follow-up phase. Patients who were treated for longer than 24 cycles continued to experience similar toxicity like diarrhoea and nausea and skin rash, but no additional, concerning side effects. There was a very small difference in a safety profile of the drug between children and adults. Children appear to tolerate the drug a little bit better than adults, because we had a higher rate of dropouts from the study in adult cohort. But, the toxicity was similar in both groups. I think this is very exciting news for clinicians, because for a long time they did not have any treatment available. Now we have additional drugs. This is second drug which is showing efficacy in plexiform neurofibroma, and this time we have a drug which is marketed also for adult population, which was completely missing in the past.
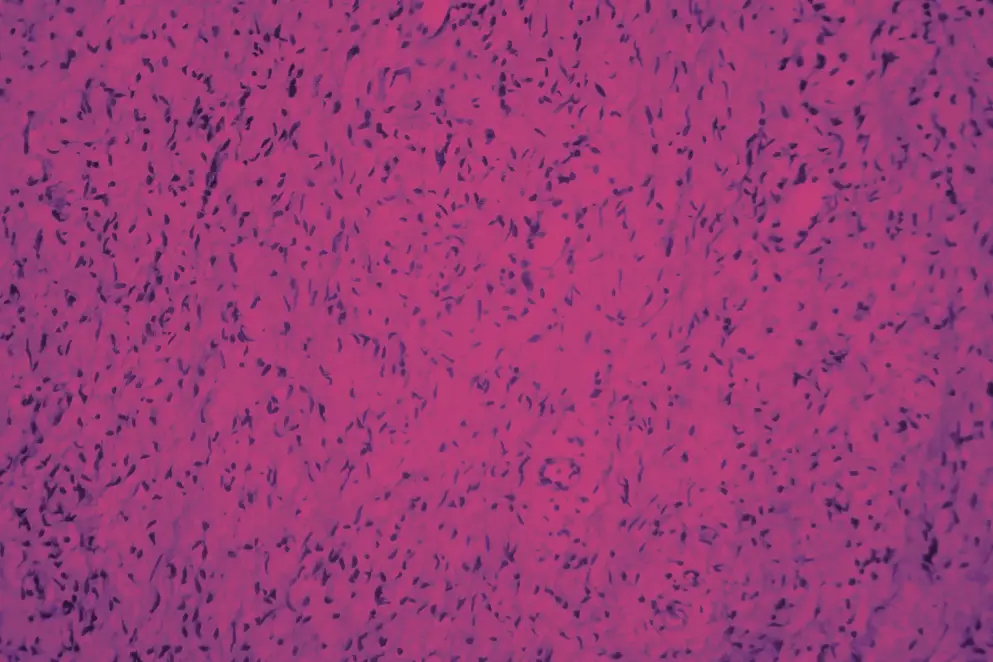
- [Dusica] This is possible. This drug still does not have effect in a 100% of patients, so additional drugs probably will be developed over time. Perhaps some combination treatments will become available, but this drug certainly has potential to be long-term treatment for many patients with NF. I just wish we continue our efforts to develop new drugs, and overall, to increase awareness of neurofibromatosis type one, because improved awareness and engagement may result in better outcomes for these patients. I think that most of specialties should know about neurofibromatosis type one because it's a multi systemic condition, which can involve pretty much any part of the human body. So, we need dermatologists, ophthalmologists, neurologists, the surgeons of any sort, endocrinologists. And, we also have to make sure that adult providers are very well aware of neurofibromatosis, because currently we have most of these providers effect of being involved in treatment of children. But, in adulthood, this condition is not so very well recognised. So we just need to increase awareness among adult medical providers. And, also remember, this is hereditary condition, so you have entire families affected with neurofibromatosis. So, it can be very emotional, and very, very special for patients who have treatment, and who have providers who are taking care of them. - The NF1 biomarker study is a prospective whole body MRI study on participants with NF1 that we would consider high risk for development of malignant peripheral nerve sheath tumors. MPNST is a dreaded complication of NF1. It's a fatal sarcoma that leads to overall decreased longevity in this population. And so we've tried to capture participants that would be high risk for development of this sarcoma, and we follow them out prospectively using whole body MRI, a non-invasive tool. And the risk factors that we've used as traits of high risk include genetic testing, known internal tumor burden, prior history of malignant peripheral nerve sheath tumor, and prior radiation. So factors like these. And we follow these patients out prospectively with serial whole-body MRI exam, and a clinical exam at our high-volume NF center over the course of five years. And the idea is to see whether they developed any suspicious lesions on imaging, and what those lesions on imaging that we think are suspicious actually turn out to be. And hopefully, we can establish what the imaging biomarker for an MPNST, or a pre-malignant lesion before an MPNST forms can be detecting using whole body MRI. The interesting part about this study is that it is prospective, it uses whole body MRI, which is a tool we use in this population, but we've combined it with diffusion weighted imaging, which is a special sequence that we perform at our institution. It's not proprietary per se, we use it in the brain frequently for the detection of strokes, but here we're using it as a marker for cellularity. So combining these two factors will allow us to characterize any lesion we detect more specifically. The need to prioritize this high risk population for detection of NF1 related MPNST is, this is the population we think is more likely to develop it, particularly in earlier age. We know from prior retrospective studies. So unlike our study, which is prospective, we know from retrospective studies that patients that have high internal tumor burden are at greater risk for development of MPNST at an earlier age. So if we can capture a pre-malignant lesion in this population earlier, then perhaps we can prevent the future development of MPNST. What would be the potential impact of this study on treatment? The most important impact that might be is if we can capture a pre-malignant or suspicious lesion before it becomes a malignant peripheral nerve sheath tumor, is that it can be treated before it becomes that fatal sarcoma. And that might impact the lifespan of a patient because this is one of the most important causes for this population to have a shorter lifespan compared with their matched cohorts of people that are unaffected with NF1. How can we use imaging biomarkers to stratify patients for surveillance or treatment? So what we've been working on so far is trying to identify pre-malignant lesions before they become an MPNST. Our current retrospective data shows that a distinct nodular lesion on MRI, so that is a peripheral nerve tumor that does not have an expected target pattern, is an imaging marker for an atypical neurofibroma, or an atypical neoplasm of unknown biologic potential. We don't know much more than that. We know maybe they tend to be more than three centimeters in size. They tend to grow rapidly. They may be FDG-avid on PET-CT, they may not. And we know a wide range of FDG values that overlap with both benign and malignant tumors. So we hope to find out more specific imaging characteristics of distinct nodular lesions that are indeed actually atypical or pre-malignant. And if we can find those lesions and characterize the distinct nodular lesion more specifically, then the suspicious lesion can be removed prior to MPNST development. So earlier treatment and MPNST development would be the optimal outcome of this biomarker study. How do imaging and genetic factors work together in this study? So we are trying to capture patients that we think are at greater risk for MPNST formation. And we know from prior data that's specific genetics and specific imaging features. So genotype as well as phenotype that can be seen by whole body MRI are associated with higher risk of MPNST development. So specific genetic testing like micro-deletion, or specific internal tumor burden, which is a more of a gray area and we hope to learn more about it, would be important risk factors on how you screen a patient. So how early you perform a whole body MRI, how often you perform a whole body MRI, and whether you modify the protocol with the addition of more sequences like diffusion weighted imaging and perhaps make the scan longer for a patient. So personalize the screening strategy for that patient would be an ideal outcome also. How do genetic factors impact screening findings and screening strategies? We know based on retrospective data that certain genetic factors like micro-deletions tend to have patients with higher internal tumor burden. So those pieces of information could be combined. One is something we can gather from a blood test while the other we can see by imaging, and those would predispose the patient to a greater risk for MPNST and that particular patient would benefit from earlier and more frequent screening. But we base this information on previously gained retrospective data. So more prospective data is needed, particularly for what we consider high internal tumor burden. We don't know quite yet based on the existing data what a threshold for high versus low is. And so we base it as radiologists, sometimes just qualitatively looking at whole body MRI. Meanwhile, there are other centers across the world that measure that tumor burden using volumetric techniques and quantify it. But even if you quantify it, there is no threshold in existence yet that says, this particular person has X amount of tumor burden, and as such is considered a high internal tumor burden and would benefit from a different screening strategy. So that's all information we're trying to gain from this study in addition to other studies that are taking place across the US. What are the most significant findings from the trial so far? The significant findings from the trial so far include that we've been able to enroll about 80 participants for this serial exam. And we noted that amongst the 80 people, especially at their baseline whole body MRI, number of patients actually had distinct nodular lesions. So about almost a fourth of that population had distinct nodular lesions, but only a small subset of those patients actually had a suspicious distinct nodular lesion that ultimately went on to either biopsy or surgery. So what we've learned is that distinct nodular lesion by itself is not the marker that we thought to be of MPNST. It needs, in addition, something else, whether it's a distinct nodular lesion plus growth, plus pain, plus prior radiation. So those are the factors we're still working on figuring out. So distinct nodular lesion itself is not the mere marker of MPNST, even though that's what we've thought on prior data. There's more to it and that's what we're learning. How can this prospective full body MRI study shape future management of patients? One of the main things we hope to point out is what additional features of distinct nodule lesion, or DNL as we call it sometimes, a distinct nodule lesion is truly pre-malignant. Whether there's a size criteria, or there's an imaging criteria, or there's a clinical criteria, or it's a size plus genetic criteria. So that's what we are still unraveling from this study. And if we can identify that, then we can more specifically identify the patients and the tumors within those patients that need to be intervened upon, and perhaps successfully prevent future development of MPNST or capture it earlier in its course. We do think that the results of this prospective whole body MRI study on high risk people with NF1 would impact screening guidelines, and particularly identify which patients. So more information about the person level risk factors in addition to which tumors. So more imaging per tumor risk factors that would benefit from greater intervention, and it might influence how often we screen these patients and how we perform that screening. Whether it's whole body MRI alone plus whole body MRI in conjunction with a sequence that I told you about diffusion weighted imaging, and how that would inform our decision making in intervening on specific DNLs versus observing them on serial exams. This study has been ongoing for about four and a half years, and we enrolled all of our baseline patients that have had baseline whole body MRI. We're still gaining more exams on an annual basis. So we need to complete the entire whole body MRI acquisition and interpretation for all five years, and we want to see who actually developed tumors. We also hope to apply more artificial intelligence and machine learning tools to see if we can predict on serial exams, who develops tumors, and which tumors end up being suspicious. Whether that addition, which will be again, a non-invasive addition, could impact our results. So we're still completing the study. What we've done is analyzed baseline characteristics, which I shared with you earlier. Which specialties could benefit from learning more about NF1 and its various disease manifestations? I think there are two main groups of medical specialists. One would be the general practitioner that could benefit from learning more about NF1, because we've learned a lot about how we screen this population. We've learned a lot about other disease manifestations. For example, osteoporosis, breast cancer risk. So the general practitioner could learn more. And then a radiologist, a general radiologist, because we've learned so much about peripheral nerve tumors in the last 10 years alone. And application of diffusion weighted imaging and disease characterization, which patients have suspicious lesions, which lesions actually need biopsy, and when to refer this person to a comprehensive NF center.
 Said Farschtschi, MD, PhD
Said Farschtschi, MD, PhD Dusica Babovic-Vuksanovic, MD
Dusica Babovic-Vuksanovic, MD Shivani Ahlawat, MD
Shivani Ahlawat, MD
