Cushing's syndrome
Cushing’s syndrome is a rare but serious endocrine disorder caused by prolonged exposure to elevated glucocorticoid levels – either from endogenous overproduction or chronic steroid therapy. While exogenous steroid use remains the most common cause, clinicians should also consider ACTH-secreting pituitary adenomas, adrenal tumors, or ectopic ACTH production in the differential diagnosis. The condition affects multiple systems and can be easy to miss in its early stages. Early recognition and initiation of targeted treatment can significantly reduce long-term complications and improve patient outcomes.
What is the estimated annual prevalence of Cushing’s syndrome?
Cushing’s syndrome affects approximately 10–15 individuals per million annually, most often adults aged 20–50. Around 70% of cases occur in women, making female patients a key demographic for screening and diagnosis.
What are the causes of Cushing’s syndrome?
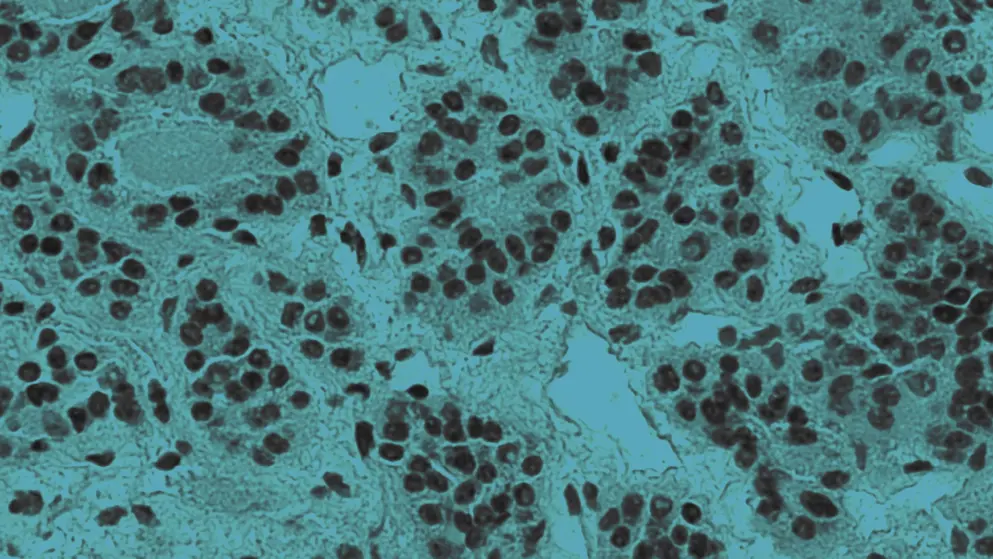
Long-term use of high-dose glucocorticoids – such as prednisone – is the leading cause. However, endogenous cases may result from ACTH-secreting pituitary adenomas (Cushing disease), adrenal tumors, or ectopic ACTH secretion from non-pituitary tumors.
What symptoms are commonly associated with Cushing’s syndrome?
Patients often present with central weight gain – most notably affecting the face, neck, dorsocervical region, chest, and abdomen – alongside proximal muscle weakness, easy bruising, violaceous striae, mood disturbances, and metabolic issues such as hypertension and glucose intolerance. Women may also experience reduced libido, menstrual irregularities, and hirsutism. Although rare in pediatric populations, Cushing’s syndrome typically manifests as rapid weight gain with stunted growth.
What treatment options are available for Cushing’s syndrome?
Treatment depends on the etiology of Cushing’s syndrome. Options include tapering or discontinuing glucocorticoids, surgical resection of tumors, radiation therapy, and pharmacologic interventions such as steroidogenesis inhibitors, pituitary-directed therapies, glucocorticoid receptor antagonists, and adrenolytic agents.
Developed by EPG Health for Medthority, independently of any sponsor.

