Transcript: Secondary HLH/MAS masterclass
Fabrizio de Benedetti, MD, PhD
All transcripts are created from interview footage and directly reflect the content of the masterclass at the time. The content is that of the speakers and is not adjusted by Medthority.
- I am Fabrizio de Benedetti and I welcome you to the masterclass in HLH/MAS with special focus on secondary HLH. I'm a paediatric rheumatologist. I work at the children hospital in Rome, Italy. What we are going to talk about in this short video, the first one of three is actually the diagnostic puzzles and how we develop early suspicion and how we make early diagnosis of secondary HLH.
We'll start with a case. This is a young girl was admitted for one week duration of fever and rash. She had abdominal pain and hepatosplenomegaly. Her lab chemistry showed increased white blood cells. Platelets were kind of within the normal range, a little bit of ferritin, significant elevation of inflammatory marker and some liver involvement with some tissue damage evident. However, in 48 hours, she rapidly deteriorated. She developed respiratory failure, generalised seizure, and she needed admission into ICU. Her lab chemistry significantly changed very rapidly. You see blood cell dropping still within the normal range. Same is true for neutrophils. Platelet dropped still within normal range. 30 marked increased in only 48 hours to 26 thousands. There was clear activation of intravascular coagulation with D-dimer sky roofed and again decreasing fibrinogen by well within the normal range. And there was significant liver involvement with sharp increase in transaminase and LDH.
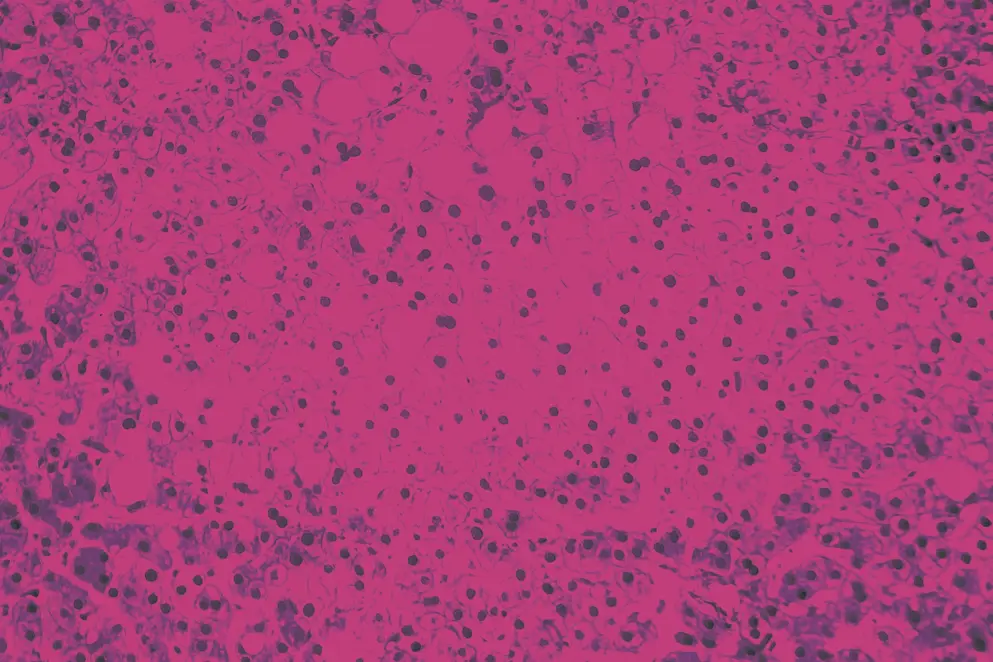
Now what is this? This is what we call hyperinflammation. The bone marrow and cerebral spinous fluid of these girl show both show in hemophagocytosis. Now, what is hyperinflammation? Hyperinflammation is one of the own goals of the immune response and inflammatory responses. Is correct, while we are very familial with the concept of autoinflammation and autoimmunity, hyperinflammation is a bit different, is activation of innate adaptive immunity in response to a reasonable stimulus to do so. For example, a viral infection.
But this responses becomes excessive and leads to damage to the host, and very often this is death. So hyperinflammation can be very dangerous. Now this has become a major issue, particularly during COVID because the world anti-inflammation was used a lot. And in 2019, right before COVID, a process was started pulling together a team of experts from paediatric rheumatology, haematology, infectious disease, ICU people to develop initial point of to consider at the early stage of diagnosis and management of suspected HLH. Now, the first issue was the name HLH/MAS, cytokine storm, this is the name that is used. We often hyperinflammation, we define it.
What are we talking about? These are the diseases of the conditions, if you wish, that we are talking about. And this includes conditions with very different causes as you can see, but they are unified and that they have HLH/MAS syndrome by the recognisable clinical and laboratory pattern, which is really persistent fever, splenomegaly, inappropriately, and I will stress inappropriately low cell counts inappropriately low for the degree of inflammation, hepatic dysfunction, coagulopathy, CNS symptom, and then elevated and or rising ferritin. Now none of these alone is specific obviously, and they must be evaluated collectively, longitudinally over time.
Couple of key messages: one, all HLH/MAS patient have elevated ferritin. All the criteria include ferritin with different threshold, whatever. But elevated ferritin is a biomarker when suspecting hyper inflammation, HLH/MAS measure ferritin. We ongoing clinical suspicion or deterioration of the patient measure serial ferritin, sometimes even twice a day because patient can get worse rapidly. Do not think that hemophagocytosis is really needed for the diagnosis of MAS. The first H of HLH is wrong. Hemophagocytic lymphohistiocystosis, Hemophagocytic, is not true. 50% of the patient is like tossing a coin, essentially don't take hemophagocytosis in the bone marrow. If you find it, that's great, but if you don't rule out. You have to perform the aspirate, the bone marrow aspiratory biopsy to rule out malignancy. And this is of upmost importance.
So back to the pattern, which is the really the one that drive your suspicion. And if you look back one second that our patient, the inappropriate low platelet were already there. Ferritin was already rising before she was in it. Okay? So this is something that is being implemented in several hospital. We have ours that the children, the Boston children hospitals have published their algorithm for concerns of HLH/MAS and what they do to put together the multidisciplinary approach and multidisciplinary team, which are needed. Neurologist, IDP, infectious disease people, hemo people, they have to be aware. Now in Boston is the rheumatology who is driving the process, but there might be different people driving it. We also have rheumatology driving the process here and we find it extremely useful. And what I found compelling by the Boston group is that they published the data before and after the introduction of these guidelines.
These are hospital guidelines, okay? And these are very small number. You see them pre evidence-based guideline 10 post only 17. But if you look at the data, I mean it, there is a pre and there is a post mortality is significantly lower. Time to MAS HLH treatment is evidently lower, may not be significantly, but it's evidently lower. So you really need to address the issue with the multidisciplinary team, knowing how you wanna raise concern in your institution. We use ferritin, we have ICU people, IT people testing ferritin. If ferritin is increased, we get paged. Maybe we got called too many times, but that's okay, better to be called too many than too few. And this is really the patient experience in the context of rapidly progressing secondary HLH as it is in our patients, they progress rapidly. They need ICU before diagnosis confirm. They go through broad spectrum antibiotics and the suspicion of infection before hyperinflammation is diagnosis. Sometimes there is hesitation in starting therapy, immunomodulatory therapy because of fear of immunosuppression. And patients are worried about the side effects of high-dose steroids. So this is, again, taken from the paper, which really summarise what you have to do. First of all, you assess, you assess your hyperinflammation using those laboratory markers, repeat them sometimes twice a day. You next investigated the potential underlying conditions. And these are a number of conditions including infections, malignancy, immunodeficiency, whatever. And this is a long, long list that you can find in this paper and this might be of help for you. And then you have to start at least to provide some supportive care. We'll discuss this in the near future.
So there are monogenic disease that cause HLH okay? And these are listed here. The list is increasing, so there's some missing here, but it doesn't matter. It's a list. You'll find a list in the paper more comprehensive. What I want to highlight here is that the monogenic HLH is only 3-10% and particularly in children. In adults is essentially close to zero. So everything else is secondary HLH/MAS. This again is from the papers. Genetic testing is very important, but takes time. And in our experience, if we do it fast, fast, fast, it takes two weeks and that's too long. So actually functional tests which include test for defective cytotoxicity and measurement of IL-18 levels may be obtained significantly faster and therefore help you setting you in the proper direction of a monogenic or non monogenic. A diagnosis of auto monogenic HLH dramatically affects future management.
Bone marrow transplantation becomes an urgent and therefore everything is changed. You have to look for underlying infections. Now there are a number of infection agents that are associated with ability to trigger HLH, Epstein Barr virus being the best one. Leishmania is very good, but it's a long, long list. Two pages long. Again, look at the paper. There is a list you can think about strange contributors or infectious triggers. Frequency depends on local prevalence. So they may completely different in eastern countries. EBV being very common from southern Italy where leishmania is very common for example. So think about this. Sometimes treating the underlying fraction may be all that is necessary for stabilising the patient. This is very true, for example for leishmania. For malignancy associated, it's essentially lymphoma. So you have to look for lymph nodes. PET/CT is usually one of the screening examination.
Again, there is a long list of screening examination in the paper. It is imperative to exclude malignancy in all cases of HLH because without the treatment of the underlying malignancy, essentially the patient is gonna die. So you need nevertheless this malignancy associated have a very severe prognosis. This is the proportion of cases by primary contributors in paediatric and adult. And I just want to underscore the significant difference that I mentioned at genetics is almost absent in adults almost because I've seen patients with monogenic familial HLH with onset in their forties, very rare. But there. Infections are much more common in children. Malignancy is much more common in adults. Almost 50% of HLH in adults are malignancy associated. Their prognosis is very, very bad. Let's go back to the recognisable clinical laboratory pattern here is listed in a different way just to fit this pattern with the available classification and diagnostic criteria. And as you can see, the elements of the pattern are picked up. Not all of them. And not always by by the different criteria with some nuances that we go through them very soon.
So this is the HLH 2004 criteria. These are designed, these are eminence based. They're not evidence based. They're designed by expert in monogenic HLH. So they are skewed towards the diagnosis of familial HLH due to cytotoxicity defect. You see that cytopenia have to be real, cytopenia not an apparent low real cytopenia. And it's again focusing on absence of cytotoxic activity criteria number seven, for example, you don't need a lot of ferritin here, which I think it's important. And think about this, you don't need dozens of thousands of ferritin. You just have to be aware of the fact that ferritin is raised. Same is true for the MAS criteria, which we have designed specifically for systemic JIA using real data for patient then expert consensus. And again, you see the ferritin is not that high. And I also would like to underscore that platelets threshold is well within normal range as it is fibrinogen thresholds, well within normal range. So it's just slow for the degree of inflammation. You don't need much of an hepatic involvement. A little bit of AST is sufficient. Okay? So again, you don't have to tick the boxes here. These criteria have the go to make you think that you have a suspected HLH. Now their scores, this is is the MAS score, which was designed for MAS. This is more complicated because the mathematical formula involved is pretty complicated. You need a calculator. Ideally you would need an app to do that. Personally don't like it. This is the HScore which was developed for secondary HLH in adults. There was only one patient with Still's disease with systemic HLH, for example. So it's a completely different setting. Again, this is a complicated score. You need to go through a lot of things to calculate it. Again, you will need to up. But again, this scores and this criteria have to make you think you can use each one you want, but they have to make you think that you are in the presence of the suspected clinical factor. You treat with some supportive care. That's obvious. Some of these patients are sick, they are feverish, they have pain. So you need to and you need to do some anti-microbial therapy certainly. However, what really changes the thing is that if the patient is persisting severe or worsening, you need to do empiric immunomodulation even before you have a diagnosis on the contributors or the underlying cause of your MAS/HLH. You start your treatment with empiric numeration. At the same time you continue your investigations of the underlying cause.
Ideally, you should be initiated as early as possible, but on the other hand, you have to wait the effect of your immunomodulatory treatment or on your ability to put forward your etiological workup. High-dose glucocorticoids remain the mainstay of treatment. They are absolutely pivotal will discuss this in the third videos. Keep also into account that anakinra and IVIG do not interfere with differentials. So if you are in the setting where your malignancy has not yet been ruled out, maybe one attitude would be to weigh, to use glucocorticoids and try to stabilise the patient with anakinra IVIG. So this is the end of this presentation. We have discussed the early suspicion and diagnosis, the clinical and laboratory pattern, again, collectively and longitudinally, the role of alerting a multidisciplinary team for HLH/MAS that may really change the outcome of your patients as the Boston Children have shown.
But all of us do know that this happens in our hospital when we do this. We have discussed the available classification diagnostic criteria and scores. We have discussed at least initial diagnostic workup for the underlying conditions and a little bit of the early stabilisation treatment. We'll get into more detail of early immunomodulation, including dosing and time in the third video. So thank you for your attention for now. Okay, we welcome back to the masterclass in HLH/MAS. We are going to discuss in this relatively short video the biomarkers and now we use modern biomarkers in in the diagnosis and management of secondary HLH/MAS patients. Now again, showing these slides about the monogenic diseases because this is where many information came from regarding the understanding of the etiopathogenesis of HLH/MAS. So these very rare patients actually did provide a number of relevant information on acquired polygenic diseases. The first piece of information came when the cytotoxicity defect was identified as a cause. And a young haematologist from Cincinnati did an experiment in mice in which it triggered HLH/MAS in peripheral deficient mice with an infections as in virus and tried to modulate this hyperinflammation in the mice. Essentially he found that by depleting CD8 positive T-cells and by neutralising interferon gamma, but not by depleting other cell types or not neutralising other cytokines, it could rescue the phenotype.
The phenotype in this mice is incompatible with life. All the mice die, and as you can see, you have survival and there were a number of data in other models showing that this was actually true and other genes were affected. And this resulted in an hypothesis that was actually brilliantly demonstrated in a paper published this very year in hypothesis that foresees that when when a T-cell recognise an infected cells, it binds and kills the cells in the presence of defective mechanism of cytotoxicity, whatever that is, the immune synapses is more intense and more prolonged. This leads to overactivation and over proliferation of the cytotoxic T-cells with overproduction of interferon gamma. Interferon gamma activates macrophages and macrophages have compensatory realised compensatory mechanisms that leads to clearance of the infected cells. Indeed, this patient never die of their infection. They die of a cytokine storm induced by the pro-inflammatory cytokines produced by the overactivated macrophages. And really the words "macrophage activation syndrome" sounds very right and but it looks only at one piece of the puzzle. And indeed the puzzles of HLH is, if you make it very simple, it's a vicious circle involving overactivated macrophages and overactivated and over proliferating T-cells it says CD8, but we'll see, maybe it's more than CD8, but nevertheless this is a simplified view and the overproduction of interferon gamma activates macrophages, macrophages produce cytokines that activate T-cells and this leads to a vicious amplifying circle that eventually lead the host to death. Now how do we measure this? Okay, the first evidence come from this paper that we published quite a few years ago now showing that CXCL9, which is a small chemokine, can be used as a proxy of interferon gamma conduction. Measuring interferon gamma is very complicated and it's not really reliable. On the other hand, CXCL9 is very stable in serum and plasma and it's overproduced in the presence essentially of interferon gamma. Nobody else induces the CXCL9 production and therefore CXCL9 in MAS patient was shown to be associated elevated during MAS but not during active disease flare, inflammatory flare and correlated with a number of parameters of that clinical pattern that we discussed before.
And since that observation, there have been a number of studies from several laboratories showing the CXCL9 is really elevated, but the graph on your left shows a paper from Scott Canna's lab showing essentially that CXCL9 is elevated in any HLH. It's elevated in MAS, it's elevated in infection associated HLH is elevated in primary monogenic familial HLH. This is the graph on your left is recent data that shows clearly that it's elevated in any secondary HLH. This secondary HLH group included a number of patients with different contributors from metabolic to inborn narrow of immunity, infections unknown because a number of them are unknown unfortunately. And so glucocorticoids do not mess up with CXCL9 measurement. And these are data from two different laboratories showing that high level of CXCL9 discriminates MAS from a flare of active systemic JST disease, cutoffs are different.
So there's still work to be done, but we are getting there. This can be used and if used in your centre you will have your own cutoff. So this is CXCL9 in our little girl, it's increased normal value below 600 and as you can see CXCL9, it's increased at admission and really skyrockets after 48 hours together with the worsening of the patient. The second adaptive immunity, let's say culprit is certainly CD8 positive T-cells. From the papers that I've shown you in mice. It took us the community, I mean the community, the HLH/MAS community, almost 15 years to figure it out that you could measure this in patients and they were very, very effective in differentiating patients with HLH/MAS from other patients. The two papers essentially one from Boston, Cincinnati and one from us showing that these T-cells are expanded. They show feature of recently activated and persistently activated T-cells.
They produce interferon gamma and they are effector memory T-cell, which is very consistent with the hypothesis that the community has been generated, has been generated about the role of CD8 positive T-cell. And this shows again the area under the curve differentiating familial, infection, various type of secondary HLH from flare of Still's disease on versus sepsis. And you see that the AUC is really high insensitivity and specificity are really important. And I think this is something relatively trivial that you can do in any laboratory who has a cytometry is a four colour cytometry really easy to do, okay? There are recent data from the Boston group showing that it's not only CD8 but also CD4 and NK T-cells or NK cells that are activated during MAS and they decline following MAS treatment, which is perfectly consistent with the hypothesis of adaptive immunity cells being hyperactivated and leading to a production of interferon garment. So to make a long short start 15 years, CXCL9 can be CXCL9 serum level can be used as a proxy of interferon gamma production. There are a huge number of data showing that this is true, including data from patient treated with the antiviral gamma antibody. You can use activated CD8 T-cells as a measure of hyperinflammation. So this is our little girl again, 6.8, that's close, that's not high, but by the time she worsen, she has significantly increased level of activated CD8 T-cells. That's not the entire story. However, the circles, the vicious circles involve IL-18 and gained information provided by studying patients with rare monogenic diseases. They're called IL-18opathies, they are characterised by skin rash, fever, splenomegaly, recurrent HLH/MAS, very early onset, very severe patients.
What is the feature of this disease? They produce high level of IL-18 moderate levels of IL-1 beta, but very high level of IL-18 in unstimulated conditions. If you take monocytes and macrophages from this patient, they release full, they're full blown releasing IL-18. And interestingly in this patient during MAS episode, the red symbols, you see an increase in CX9 levels that is correlated with ferritin levels. Now, the working hypothesis is the working hypothesis. The mechanism here is the presence of the ability is the ability of IL-18 to induce interferon gamma production by T-cells and NK cells. So this is really closing the vicious circles that I've shown to you. Again, a number of paper showing that IL-18 is market increase in MAS is also increased in sJIA and we discussed this in the third presentation briefly. It's increased, variable increase in infectious associated HLH but it's not increased in familial HLH which are due to defective cytotoxicity. And this is interesting and I talked to this up a little bit in the future, it's clearly distinguished MAS from active flare of inflammation Still's disease again a few papers. So really the vicious circles here allowed us to identify the number of biomarkers that we can easily measure and that we can use in clinical practise to help us in solving the diagnostic puzzle.
And as I told you, you can get into HLH if you have a monogenic disease, you can get into HLH either by overactivation of adaptive immunity because you have defective cytotoxicity or you can get into MAS/HLH into the vicious circle by overacting, overactivated macrophages which produce a lot of IL-18. Now the role of IL-1 is always in this vicious circles and we'll come back to that. The evidence in animal models and in vitro is relatively low, but the evidence from treating the patient is very high. So IL-1 should be part of this vicious circle. However, it should be pointed out that we cannot realise reliably measure IL-1 and therefore IL-1 is not a useful biomarker in the clinical practise. So this is our patients, again, very high level of IL-18. Here are the normal values and you can see it's skyrocketing IL-18. Now skyrocket IL-18 poses an issue on the background triggering condition of this patient will get back to that during the third presentation. And I'd like to finish by going back to the story of this patient. She was treated with a lot glucocorticoid. She required ultra filtration with Cytosorb. She was treated with IV cyclosporine targeting very high level. She stayed in ICU for three weeks, hospital admission, almost two months, no more than two months. High dose methylprednisolone for almost two months. And she developed all sorts of side effects. So I think this is what you don't want to see, okay? You want this patient to be treated more effectively and we discussed this in the third video.
Can we use biomarker to predict the disease? And yes we can. So we developed a score, which we call the MAS clinical severity score that underlines a few of the things that actually our young patient went through a lot of glucocorticoids and ICU admission, length of hospitalisation, and obviously death. Luckily she survived. So she has severe disease, severe MAS by our cutoff. And essentially in our series of patient, 60% of the patient have mild MAS and 40% of the patient has severe MAS. What if we look at biomarkers, the traditional biomarker, ferritin, platelet, transaminase, or we look at the more evolved biomarkers. CXCL9, IL-18, didn't talk about neopterin, but this is a proxy of interferon gamma production as well. None of them alone predict mass severity with a clinical relevant reliability. You see sensitivity specificity you don't really like to use in clinic.
However, when Ariana in our lab played around with multiple combination to identify the suitable multi parameter score to define biomarker driven risk stratification, she came up with this score that included CXCL9 that had the ability essentially to pick up all severe MAS with a specificity of 74%. That's not too bad. They could be using clinical practise to identify patient that may have a very severe cause and therefore require potentiation of treatments. It's not only onset, it's also the course of the disease. We have studied CXCL9 in depth and we found that levels at one to two weeks after starting treatment initiation predict the ability to achieve MAS remission at two months. This is the probability of MAS remission at two months depending on your CXCL9 levels. And you know this simply logistical analysis shows that your probability to achieve MAS remission at two months if you have CXCL9 levels below 800 at two weeks is 9.3-fold greater. This is significant. It helps you to identify patient that may require that are not responding so efficiently to the first round of treatment.
They may therefore require intensification. Again, back to our vicious circles in which the biomarkers, some of them can be used not only for diagnosing but for prognosis and monitoring your response to treatment when you're managing one of these severe patient. So I'd like to finish again, showing what we don't want now to happen. We don't want these kids. This girl was diagnosed with 2016, the biomarkers were not there, the targeted therapies were not there yet and therefore she underwent a really severe course with a lot of glucocorticoids. I think this is all for for now and I hope to see you in the third video regarding treatment. So welcome back to this third video of three videos of this HLH/MAS masterclass.
We are going to discuss today treatment pathways in various form of secondary HLH/MAS. So again, we will start from the point to consider published in 2023 that saw a rather large team of specialist in HLH/MAS convening together and discussing early management and early diagnosis, which we have discussed in the other videos. I'm showing to you one of the overarching principle in which I underline the word urgency. In some of these patients, and you have seen one of such a case in the previous videos do worsen very rapidly. So in this setting, HLH/MAS may become a treatment urgency. So this is the algorithm published in the point of consider. We have already looked at it in a few issues. Treatment, there is a need for supportive empiric, anti-microbial prophylaxis therapies. I'm not going to talk about those. You are all physicians and you know what you have to do. Just keep in mind that this patient are at risk of receiving prolonged immunosuppression. So that why when designing your supportive of empiric anti-microbial therapies or prophylactic anti-microbial therapies, take this into account.
Now the second major pillar of the management is early immunomodulation. And we discussed patient who have persistent severe or worsening even rapidly worsening inflammation or organ dysfunction. These are the patient that you should target even before completing your investigations for underlying trigger of the disease. Now the three pillar of early immunomodulation are glucocorticoids and anakinra and IVIG. Except for glucocorticoids, everything I'm going to talk about today is off-label with a couple of exception, which I'm actually going to mention. So keep in mind everything is off-label except the two exceptions I'm gonna mention. So this is the case we discussed in the previous two videos and that we used to drive us through the early diagnosis and the biomarkers thing. Now this is a patient who received very heavy treatment, particularly very heavy glucocorticoid treatment. She was treated with cyclosporine IV, a number of pulses, 12, she required ICD remission ultra-filtration with cytosome. She paid a price for this, she survived, but she paid the price for this in terms of systemic side effects of glucocorticoids. Now why glucocorticoids are the mainstays? Because they are highly effective in many patients because of the broad anti-inflammatory immunosuppressive effects.
And actually this is what you may need for some patients. The cons, well we know glucocorticoids maybe since I was born, to tell you the truth and they have a number of side effects that are listed here and you know them when more than I do. However, keep in mind that glucocorticoids are potentially damaging if a misdiagnosis is made, particularly a malignin is missed. So when using them take into account, they may affect your diagnostic workup. Now, dosing regimen. There are no guidelines. They are very variable. This is what the point of recommendation states. If you're gonna use IV, you should use IV. A high dose in the adult world, am a paediatrician, remember, it's one to two milligramme per kilogramme per day. I feel this is low dose. Dexa should be used when there is CNS involvement because dexa crosses the blood brain barriers. Usually high dose IV methyl prednisolone is usually done with pulses. Dosing varies significantly between 10 to 30 milligramme per kilogramme per day. This is my opinion, one to two milligramme per kilogramme per day is too low. It's by far too low. Even when you are switching from pulses to IV dosing, one milligramme is far too low in your risk to lose controls. Dexa, dexa is fine, but keep in mind that one milligramme 10 milligramme per metre square are equals to four per kilogramme of prednisone or methprednisone.
So you are not giving a high dose of glucocorticoid . So maybe dexa sometimes it's used on top of high dose pulses. Pulses are an issue. It says max one gramme per day. This is written all over the place. Well if you weigh 30 kilogrammes, you're going to get one gramme. If you weigh 60 kilogrammes, you're going to get one gramme. So you are going to be undertreated if you are above 30 kilogrammes. Keep this in mind when you're using high dose glucocorticoid. There was a study that I'm gonna mention a couple of times in the presentation. It's called the METAPHOR study has been a survey for treatment of anything in MAS and secondary HLH. Most of the patients were Still's disease because this was done in a rheumatology environment. But as you can see here, some patients receive glucocorticoid monotherapy. The great majority received glucocorticoids with other communications. Those was very variable, 60% of them. So more than half received pulses. Again, very varying dose dose regimen. So the the take a message here, we all use glucocorticoid, they remain the mainstay of treatment. There's no form of clinical trial, but there is however, a risk for delayed or inadequate response in severe case. And this is really outlined by the fact that most of the patient did not receive glucocorticoid alone. How do you define glucocorticoid refractory MAS/HLH so that you can step up treatment if you are using a step up approach. There's no definition. It's pretty clear that most of us have used something else. So we are stepping up treatment. In the only trial in MAS, which is the emapalumab trials, this was the definition, in adequate response to high dose intravenous glucocorticoids defined by the treating physician. So there is no threshold anywhere defined as unsatisfactory response to greater than two meaning per kilo per day. Again, capped at 60, but this is written all over the place and there's nothing we can do. And pulses are included but not limited to. I would suggest that this is a little bit that pulses should be done to everybody. Let's switch to anakinra. Anakinra again is off label is there's no clinical trials only case serious reported. The great advantage is that we know, and the task force was pretty adamant about this, that does not interfere with diagnostic workup for malignancy infectious disease or primary HLH.
So you should be relatively unconcerned in using anakinra in the context of early immuno, sometimes without glucocorticoid. If you are not yet there, eh, excluding a malignancy. As I mentioned, no formal trials. However, there was a post-hoc analysis of a sepsis trial that uses very high doses, 40 milligramme per kilogramme per day iv, and that's much more that was in the label, which is max two milligramme max 100 milligramme per day. There are multiple case series with different underlying triggers and there are data from metaphor studies. The take home message and that there is all over these studies, high rates of satisfactory response. Let me show you a couple of example. This is the sepsis trial. These are patients with proven sepsis in ICU treated with anakinra. The doses that I described before, as you can see, there was an effect only when you consider patient who had hyperinflammation.
And this study, everything was not measured, but there was liver function tested D dimer measure. And this were used as proxy of hyperinflammation. When this patient were analysed treatment with anakinra for only three days led to a 50%, led to significantly proven in survival. And I think this is a major finding because it underscores not only the efficacy in hyperinflammtion sepsis or hyperdynamic sepsis, but also underscore the safety of anakinra in the context of of very critically ill patients with infections. The METAPHOR studies have looked at anakinra. These are the take home message. A lot of patients, those very variable, again, as I mentioned from two, the label to the sepsis trial dose high dose was reported at least for approximately a few dozens of patients. All of these after 2020, and we will call I dose anakinra at least five milligramme per kilogramme day, which is what I advise. This is expert opinion, if I'm not expert, to use in your patient if you decide to use anakinra. The response rate was very variable. The best response rate was observed in HLH/MAS patients. If you wanna look at the case series, I think this is one you should looked at. There are different causes for secondary HLH overall mortality still 27%, which is far from being very satisfactory, but it's better than what used to before. And I think I will underscore the association of the early use of anakinra with reduced mortality to kind of support the rationale of using it. Why using your, I'm not going to talk about IVIG. IVIG, there's nothing there on IVIG essentially, but it is believed that is on one hand it is anti-inflammatory, the other hand may help in treating the other underlying infectious triggers viral often if there. So why you do the early modulation? You keep assessing and you keep investigating because this is your virtual circle in MAS. Early immunomodulation assessing and keep on investigating the underlying disease.
Now this is a busy slide. It shows the five overarching principle, one of each I've already shown to you number, the last one. However, these are important. We have already discussed the clinical pattern. Each one of these elements should be viewed collectively and longitudinally. We have already discussed the role of hyperferritinemia in video one. We have already discussed the underlying predisposing conditions or inflammatory triggers. I just urge you to look at the overarching principle D. Investigating and creating modifiable contributor is essential and sometimes it's the only thing you have to do. So keep this in mind. HLH/MAS should be treated with an urgency. This we have discussed at the very beginning. I like to underline the overarching principle F the management of this patient requires expertise. So the statement says, may benefit from consultation with experts in these disorders. And this is particularly due because the new emerging therapies that we are going to discuss in the near future are not available everywhere, but may really change the life and the outcome of these patients. So this is our little patients. Again, she was treated a long time ago. She was treated in 2016 and there was nothing except glucocorticoid. She had a very, very difficult cause of disease with relapsing remitting HLH like feature for a couple of years. In the end she developed a flare with persistent fever rash. She developed full blown arthritis and diagnosis of sJIA was made.
We went back and measured IL-18 in the samples obtained at admission and indeed there was plenty of IL-18 there. At that point the patient had a number of relapse and flare and was treated with different drugs. And again, she received almost everything that's available in this setting. To describe the treatment, we'll go back to the vicious circles that was presented to you in video two, the vicious circles between innate and adaptive immunity with activated T-cells producing a number of cytokines and particular interferon gamma who activates and expands macrophages. The macrophages produce IL-18 and IL-1 and other inflammatory cytokines that leads to the cytokine storms IL-18 and IL-1 also interns do activate CD8 positive T-cell leading to this vicious circles that we have discussed when we were discussing the biomarkers that are used. Now we will use the same vicious circles to discuss treatment approach. First drug that I like to discuss is janus kinase inhibitors. This is not really a targeted treatment. This is a very immunosuppressive evolved treatment that targets the targets immune cells, JAKs are highly, they are required, JAKs are required for critical function.
They're highly conserved and non-redundant JAK ISO from deficiency knockout mice or knockout humans, have a severe clinical phenotypes. Some of them are not compatible with life. Actually most of them are not compatible with life unless HSCT is performed. Now let's keep this in mind. IL-1 and IL-18 receptor do not signal it through juxta. So in that vicious circles you are targeting adaptive immunity. The objective is not to block the JAK pathway completely because this is compatible with life is, the objective is to reversibly reduce deem, I would say the activity of one or more of the JAK isoform here are the six receptor families and the number of cytokines that one is going to inhibit with the JAK inhibitors. None of the JAK inhibitor is similar to each other. They have different affinity for the different isoforms. So they will differentially inhibit different cytokine receptor families and therefore one, they cannot be mutually transferred one to each other. There are a number of case records, these are some. There keep appearing responses satisfactory in certain setting, less satisfactory in others. Certainly the window of opportunity, the window of the therapeutic windows with this drug is rather narrow. This is even very clear in mouse models. I'm not going to go through these details, but in mouse models there are publications showing very narrow therapeutic window with the use of a number of JAK inhibitors. So targeting the JAK stat pathway may be useful. Keep in mind this is not really targeted therapies.
This is deeming multiple cytokine receptors. Approximately 30 cytokines is not wiping off it's dimming the signalling from these receptors. We have mentioned interferon gamma when we talked about biomarkers, not because interferon gamma is a biomarker itself, but because CXCL9 , that is a proxy of interferon gamma production is a biomarker. Now interferon gamma is highly over expressed in all animal models of HLH/MAS and when neutralisation was tested, it turns out to be beneficial in the animal models and there are a number of data showing that this is the case. Now interferon gamma inhibition in hyperinflammation can be achieved with a drug. It's an interferon gamma. Fully human interferon gamma neutralising monoclonal antibodies called the emapalumab has been tested in a trial in primary HLH. We'll see the results in a second and in trials the second is not yet published in MAS. The the dosing regimens that were used were different based on different rationales. We won't get into the details of this. This is the exception. Emapalumab is FDA approved for the treatment of MAS in sJIA and for the treatment of primary HLH. This is the trial in primary phagocytic lymphosteocytosis. As I mentioned in my previous videos, these are very rare instances.
These are patients who failed standard of care, usually HLH 2004 protocol. The survival in first line HLH 204 is usually around 50-60%. The survival in second line patient is very difficult to define, but in this studies was above 70%. It should have been significantly lower. This although open label led the FDA to approve the drug, the efficacy and safety of emapalumab was tested in a trial inpatient with MAS in the context of what we now call Still's disease adult in children. It was an open label trial in patients who had failed high dose glucocorticoids. Most of them had failed also on anakinra and of cyclosporine. There was a prompted decrease in CXCL9 levels demonstrating effective neutralisation. These are the demographic features. I don't think I have to stress anything except that the majority of patient had received pulses and that the majority of patient had received either cyclosporine or anakinra or both. This is the efficacy outcome, it's the mass remission criteria. This criteria of response was designed for this study and it's the only outcome measure of MAS is available. Essentially it says normalisation of MAS clinical sinus symptom on MAS and normalisation of laboratory parameters as shown down here, including white blood cell platelet count, liver enzyme, fibrinogen and ferritin. And here you see a survival core for time to first MAS remission, which was achieved by 13 out of the 14 patient enrolled in the study. Here you see glucocorticoid tapering during the study. This is shown as mean glucocorticoid dose per day in the week, either preceding emapalumab treatment or in the week following emapalumab treatment. And you can see that in the week preceding emapalumab treatment, the median average daily dose was 15.7 milligramme per kilogramme of prednisone equivalent. It was down to 1.8 during the second week of treatment with emapalumab. Here are some of the trends of laboratory features. You see ferritin very rapid decrease in ferritin. By week two you are down essentially very close to normal. Same is true for liver enzyme shown here, but this is true also for many other parameters safety wise.
Now there are humans with functional interferon gamma deficiencies, which are either interferon gamma receptor deficient, which are very rare, but also patient who have other antibodies interferon gamma, the large cohort of patient in the study with auto antibody interferon gamma. So they're functional interferon gamma deficient. They manage cellular, but they have zoster, they have cryptococcus infection, they have infections with intracellular bacteria, salmonella and mycobacteria, makes sense activation of macrophages, and they have infection from this nasty fungus that luckily we don't have in the western world. In the trials with the for design prophylaxis with acyclovir, there was a screening for mycobacteria and salmonella and there were no cases. There were five events of CMV. One was a reactivation reported a serious adverse events and four test positive, which were a little bit of a surprise because CMV is not in this table. However, all of them responded to standard of care treatment with valganciclovir. And so we advise that you keep an eye on CMV if you're using emapalumab. As I mentioned it, CXCL9 dropped. As you can see, not in all patients. There are patients who really, this is a log scaler. There are patient in which either they stay high or they increase wards. So keep this in mind.
You may need to adjust dosing and we'll see an example. CXCL9 levels at the end of treatment are associated with response. These are probability to achieve complete response. These are data from the primary HLH study showing that the lower your CXCL9, the higher the probability of having achieved response. Again, the the more efficiently you neutralise, the higher the probability to achieve response. And this is a case that you have to look into a little bit detail on the left hand side, you see ferritin increasing after emapalumab treatment a little bit, the purple line and you see emapalumab levels going down a little bit, not managing until we went to a twice daily dosing interval, substantially increasing the dose of, but this allowed to control to achieve higher levels of emapalumab in the blood to control disease activity. There were some flares of the underlying sJIA observed during the study. Six flares were observed in patients who had either discontinue anakinra before emapalumab or had not previously received and were not receiving anakinra during the study. We therefore designed an amendment in the study allowing anakinra to be used together with the emapalumab that were have no SJ flares observed in the five patient who continued anakinra after initiating emapalumab. Importantly, there was no increase in the rate of infectious adverse events during emapalumab and anakinra treatment compared to patients receiving emapalumab alone. This table shows you the adverse events and the rates and the infections adverse events and their rates and there was no significant, no difference at all among the two little. So in summary, emapalumab has been used in HLH/MAS.
It's approved for primary HLH FDA-approved for primary HLH and patient with MAS in the context of Still's disease. There are several published with different cause of HLH/MAS and it appears to be effective all over the board. Malignancy associated HLH is always very difficult to treat. So the numbers here are not as good as there are real world data in HLH/MAS on over 100 patients that have been using hemo essentially in the US. Safety appears predictable and preventable with a question mark on CMV, which is a little bit of a surprise and there was a possibility to increase there is a possibility to increase dose based on response. This is due to the fact that some patient produce very high level of interferon gamma and in this case, target mediated drug disposition comes into play. So here it is, the second drug, the interferon gamma appears to involve across all HLH four.
CXCL9 can be used as a proxy of interferon gamma production and as a measure of response to interferon gamma inhibition and emapalumab is FDA a approved for primary HLH and the context of Still's. IL-18 is the last target I would like to talk about. It's increased in mass, it's increased in some of the infection associated HLH. Therefore again, if you think about that vicious circles, some of the patients do get into the vicious circle, not by overactivation adaptive immunity but by overactivation of innate immunity. I cheated a little bit when I showed this table because most of the MAS secondary HLH models in mice are highly team mediated one way or the other. And indeed there there are two drugs, tadekinig-alpha, who is a recombinant aine binding protein and the bispecific antibody that neutralises IL-1 with one arm and IL-18 with the other arm, which is called MAS825, which you know is being built with a rational that inhibiting both IL-1 and IL-18 may results in better efficacy. They're aware, two trials ongoing, both of them are concluded. A phase three study was assess the technique NLRC4 XIAP deficiency, the neuropathies we discussed in video number two, and a similar study in NRC4, CDC42cterm and deficiency in with with MAS825. Let me just go back one second to Still's disease.
There are patients very rare who have relapsing persistent recurrent MAS. These are very difficult treat. This is actually the patient that I show it to you. And indeed there is a phase two trial due to begin before the end of this year with MAS825 in MAS difficult to treat Still's disease patients. Let me finish with our patients. Shared a long story as I mentioned to you. Received anything, received anakinra and anakinra dose received two trials of emapalumab. One is not shown here. Actually in the end she received MAS825. This is a happy ending story because she had finally a complete response. She's in remission since now almost three years with everything is normal. She's now prolonging the dosing. Did develop MAS825.
So this is a happy ending story, but things are fairly complicated. And I like to finish by mentioning again, the experts of the overarching principle with the expert. They are particularly useful in the context of treatment, specific context, apologies. And there's a list of drugs here. Some of them we have mentioned it in this presentation, some of them we have not. Certainly we have not talked about HSCT, which is a resource in certain setting. So I like to finish encouraging people to consult experts, particularly for difficult patients.
They're all here essentially. I'm sure you'll find somebody that if you look at the names of the paper. So I like to thank them for the work we have done together with the task force and with this I finish. Thank you very much.
Developed independently by EPG Health, which received an educational grant from Sobi, awarded to EPG Health to help provide its healthcare professional members with access to the highest quality medical and scientific information, education and associated relevant content.
Updates in your area
of interest
of interest
Articles your peers
are looking at
are looking at
Bookmarks
saved
saved
Days to your
next event
next event
